Transcription
Issue 10 2019IQVIA APAC Insight
Table of contentsPatient-centric decision making in the digital age4Introduction5Understanding the healthcare decision journey5Importance of involving the patient in decision making6Ways to involve the patient in decision making6Future outlook9Conclusion10Innovative funding models for treatment of cancer and otherhigh-cost chronic noncommunicable diseases12Bringing quality and affordable medicines to populations14Universal Healthcare Coverage (UHC) in Southeast Asia: An overview and progress15Challenges in ensuring access to quality and affordable medicines17Importance of providing access to affordable and quality medicines for UHC20Future horizons: Improving population health outcomes for UHC21Delivering patient-centric care with digitalization in MedTech24Digital health is already delivering patient-centric care24Digital health is rapidly gaining traction in MedTech26Digital health is here to stay: Adapt or be left behind27The next generation of care29Claims substantiation in Southeast Asia32Significant needs, vast opportunities32Claim selection and substantiation32Big data & the big picture: Innovation in claims37The future38Keys to success38
iqvia.com 3
Patient-centric decision making in the digital ageThe importance of the patient’s voice and approaches toincorporating it in healthcare decision making4 Patient-centric decision making in the digital age
Introductiondelivery system. Decisions made in the deploymentA patient’s involvement in healthcare decision makingnot take into account the patient’s perspective. Theis typically limited to the period between diagnosisquestion then is, whether these decisions are trulyand the initiation of the treatment pathway. Therepresentative of the patient voice and if patientshealthcare provider generally has direct control overshould contribute more towards matters concerningthe patient’s clinical management, with payers andtheir health and wellbeing.of an appropriate method of treatment often doesgovernment agencies exerting some influence overthe availability and accessibility of treatment options.Medicine is a complex subject with multiplespecialized domains of knowledge. DespiteThe healthcare system’s traditional gatekeepinghaving access to a plethora of information online,paradigm – experts should decide the best treatmentsthere remains a gap between information that isfor patients – has resulted in a largely product-centricavailable to healthcare professionals and patients.approach to healthcare decision making, where eachFurthermore, the healthcare industry is highlyregulated to uphold safety standards. Consequently,regulators in most settings do not permit direct-product or healthcare technology is assessed anddiscussed individually. A product is evaluated first byregulators for its safety, quality and efficacy beforeto-patient promotional activities of any medicalbeing granted marketing authorization. Thereafter,products. All information and activities involvingpayers and policy makers assess the product’s valuepatients are scrutinized and often require approvalfrom health authorities. Policymakers and payers arealso involved but play different roles in ensuring theprovision of safe, effective, quality, affordable andUnderstanding the healthcaredecision making journeyfor inclusion in their country’s public health insurancebenefit package. Finally, physicians discuss this‘available’ treatment option with their patients (Figure 1).value-for-money services through the healthcareKey decision maker(s)and stakeholder(s)PhaseFigure 1: Product-centric approach: The traditional healthcare decision making journeyResearch &developmentMarketingauthorization Manufacturers Investors Researchers RegulatorsPricing &reimbursement Payers Policy makers HTA agencyPatient's influence and understanding is limitedDecision pointTreatmentPatient accessto treatment Physicians Healthcareproviders Physicians Healthcareproviders PatientsPatient's sphereof influence in theproduct-centricapproachiqvia.com 5
Importance of involving thepatient in decision makingDigital is driving change across industries and thehealthcare industry is no exception. The availabilityof information and the accessibility to digitaltechnologies have given rise to the ‘connectedpatient’ who now takes charge of his or her own wellbeing, enabled via online tools, the internet, peer-topeer sharing, consumer health devices, and mobileapps. The rise of digital has empowered patientsto take charge of their own health, granting themgreater confidence and autonomy over decisionsrelating to their health.Some other advancements include the availabilityof telemedicine, home care and concierge care.These care delivery models offer attributes such asconvenience, timeliness, value, communication andattention, which might be important to patientsbut sometimes overlooked by healthcare decisionmakers. A growing educated and technology-savvypopulation has raised the awareness of treatmentoptions and bridged the knowledge disparity betweenthe patient and the physician. These new technologyenabled care delivery models enable the inclusion ofthe patient’s voice in the treatment journey in wayswith an opportunity to re-evaluate what classifies as‘outcome’ or ‘quality-of-life’ from the perspectives ofthe patient. This in turn can drive critical appreciationof existing health technology evaluation frameworksand drive the adoption of these technologies basedon criteria beyond just its cost and efficacy alone, withthe intention of benefitting the patient.Therefore, insights generated through patient-centeredapproaches can help to shape research and policypriorities, guide the development of market access andpricing strategies of a treatment, and provide additionalengagement opportunities among stakeholders.Manufacturers share in their role in realizing this goalbut may also greatly benefit from patient insightsto determine research priorities, understanding thepain-points and behavior patterns of the end-user,develop market access and pricing strategies, andengagement opportunities with gatekeepers.Ways to involve the patientin decision makingIncorporating patient-reported outcome (PRO)data into marketing authorization decisionThe importance of considering PROs alongsidewhich might not have been possible a decade ago.biomarkers of health improvement in clinical drugThe Institute of Medicine (IOM) defines patient-in parallel to advances in patient-centric healthcare,centered care as: “Providing care that is respectfulas evidenced by the increased use of PROs as clinicalof, and responsive to, individual patient preferences,endpoints in clinical trials (Figure 2).research has increased over the past two decadesneeds and values, and ensuring that patientvalues guide all clinical decisions”1. Through digitaltechnologies, patients now have a desire and abilityto take a more active role in decisions related to theirFigure 2: Number of PROs used as an endpointin clinical trialshealth. This alters the patient-physician relationship30%dynamic and enables conversations that facilitate25%a healthcare choice together. This is the Shared20%Decision Making approach. Studies have shown that15%patient involvement in decision making has a positive10%association with their health outcomes2,3.5%0%Given the complexities in health and healthcare,the other benefit of incorporating the patient voiceis that it provides stakeholders and industry alike6 Patient-centric decision making in the digital ageThe use of PROs as anendpoint in clinical trialsduring 2004-20074The use of PROs as anendpoint in clinical trialsduring 2007-20135
PROs transform a qualitative endpoint into aquantifiable outcome and in the process, these add apatient’s perspective on the impact of treatment ontheir health outcomes. In doing so, value created forthe patients can be weighed against other traditionalclinical outcomes. There are several available validatedtools to measure a patient’s health status. HealthRelated Quality of Life (HRQoL) is the endpoint thatassesses various dimensions such as the physicalfunction, social function, pain severity, and mentalstatus. HRQoL is recognized as one of key outcomesbecause it can measure the patients’ health state andcan also be translated into utility values and QualityAdjusted Life Year (QALY) which are commonly used asindicators for health care resource allocation as wellas reimbursement decisions worldwide. The NationalInstitute for Health and Care Excellence (NICE), forexample, recommends the use of QALYs as a measureof health benefit for their ‘reference case’, to enablea standardized approach for comparing economicevaluations across different healthcare servicesand technologies6. Several countries in Asia such asAustralia, South Korea, Singapore and Thailand followthe same recommendation. Hence, HRQoL has becomea vital endpoint for most clinical trials.PROs transform a qualitativeendpoint into a quantifiable outcomePatient preferences should complement PROs andprovide a more comprehensive understanding ofthe needs, values and priorities of patients for theirtreatment and care. Patient preference elicitationmethods such as conjoint analysis, time trade-offand Willingness-To-Pay (WTP) have become popularmethodologies for outcomes research as they allowflexibility in addressing various research questions.For example, it can determine the total cost and valueof a health intervention, evaluate how patients valuean existing treatment versus a simulated one beforeit is really implemented, and address issues relatedto treatment adherence or process. WTP studiesare particularly insightful as more countries movetowards universal health coverage and establish theirHealth Technology Assessment (HTA) processes7.WTP can guide the development of threshold rangesand justify cost-effectiveness and reimbursementdecision for proposed new treatments. Countriessuch as Thailand have developed their own thresholdthrough WTP studies8. During the HTA process,Integrating patient preference and involvementthe focus is often on the product’s value as well asin the HTA processaffordability due to limited government healthcareThe use of PROs alone is not enough to lead thebudgets. Unsurprisingly, clinical outcomes and costsparadigm shift towards patient-centered healthcare.often dominate these conversations but there haveCase study - Listening to the patient’s voice:The reimbursement of cochlear implants in Taiwan9Patients, caregivers or patient groups are invitedare also considered in the reimbursement decisionto submit their inputs on the National Healthmaking process. The involvement of patients led toInsurance Administration (NHIA) website up to 14the reimbursement of cochlear implants for hearing-days prior to a scheduled Pharmaceutical Benefitimpaired patients under 18 years old in Taiwan sinceand Reimbursement Scheme (PBRS) meeting. TheseJuly 2017. Undoubtedly, the involvement of patientsinputs are collected and summarized by the HTAin the HTA process are not without limitations anddivision. Additionally, patient representatives couldbarriers. Continuous efforts are still needed to refinebe invited to the PBRS Joint Meeting to representthe input collection methodology and establishthe patient voice and express their opinions. Otheran efficient patient-HTA process. And the NHIA isthan clinical and economic evidence, patients’ inputscommitted to progress along this journey.iqvia.com 7
been encouraging developments where patients’Getting more ‘value’ out of the value propositionperspectives have been given greater weightage.A value dossier is one of the most important tools inAustralia has actively pursued mechanisms to do thismarket access. A compelling value proposition clearlyand started the Patient Voice Initiative in 2015 . Thedemonstrates the evidence-based benefits a productinitiative brings together professionals from industryhas to offer as compared to its cost, and against itsand academia with patient presentative groups tocompetitors. Essentially, people buy when they seediscuss methods and approaches to incorporatevalue. Perception of value, however, is subjective.patient perspectives on value assessments. Similarly,Traditionally, healthcare professionals and payersTaiwan has started involving patients in the HTAwere the primary focus of product value messaging.decision making process since 2015 .This is due to the established healthcare paradigm,109One framework that has been leveraged by severalcountries to integrate patients’ perspective inreimbursement decisions is Multi-Criteria DecisionAnalysis (MCDA). MCDA is a structured technique thatexplicitly incorporates several criteria including patientperspectives into healthcare decision making. MCDAhas been used for health resource allocation andpolicy prioritization in several European countries andhas been explored in the region in countries such asThailand and Taiwan.8 Patient-centric decision making in the digital agewhere manufacturers serve patients through thesestakeholders with limited or no direct interaction withthe patient. However, what matters to a healthcareprofessional or a payer might differ from what mattersto a patient. This difference in value perception stemsfrom the difference in needs and perspectives. Byincorporating evidence generated from patient’s voice,a solid value proposition which is relevant across allstakeholders can be achieved.
Empowering patients through decision aidsAI would also help in bringing the patient’s perspectiveDecision aids are tools which can help patients makewhich truly reflects specific needs from patients andinformed decisions regarding their own health. Thesesupport a more patient-centric healthcare decision making.tools are helpful in the context of Shared Decision Makingwhere physicians work together with patients to decideon interventions based on evidence as well as patient’spreference. It has been shown that initiating treatmentsbased on patients’ preferences improves treatmentadherence and satisfaction with care11. Leveraging theadvancement in technology, a web-based decision aid cannow be developed with minimal cost. Studies have shownCase study - ArtificialIntelligence (AI) at its bestin China: The Ping An GoodDoctor16that a web-based format performs similarly to conventionalThe Ping An Good Doctor portal provides a linkbetween patients, healthcare providers and payers.printed or video materials in terms of decision-qualityIt connects 265 million users with healthcareoutcomes12. The web-based approach increases patientproviders from thousands of clinics and pharmacyaccess to decision aids as it is readily available andoutlets across China. The app provides a one-stopmaintains the anonymity of patients. Web-based decisionsolution to cater for all healthcare needs. Patientsaids are increasingly used across different therapeuticcan utilize the app to access the healthcare systemareas such as oncology and immunology13,14,15.and request for online consultations. The artificialFuture outlookThe evolution of digital health has transformedtraditional healthcare. Tools can now readily beleveraged to connect the dots between patients andvarious other stakeholders, in order to support patientcentric healthcare decision making.Gathering patient insights from AI and big dataPowered by technology, data related to patientpreferences and treatment outcomes are increasinglybecoming cheaper and faster to obtain. Technologies suchas Artificial Intelligence (AI) have transformed patients’lives and healthcare experience. Wearables can be usedto pick up events, outcomes and behaviors of interest.Patient preference could be elucidated from app usage,search histories, and medical records. AI may in futurebe able to infer hidden priorities and criteria that patientsand clinicians themselves might have been unaware of.The possibilities are endless.intelligence (AI) assisted online consultation collectsrelevant information from patients. A preliminaryreport will be generated and sent to a doctor forfurther consultation. The doctor’s decisions arecaptured and entered into a machine learningsystem. This enables the AI model to continuouslyimprove its diagnoses and predictions with thegoal of being able to treat patients completelyindependently of human input. Patients can also filltheir prescriptions and purchase drug through theapp. The costs of treatment are borne by payerswhich are linked on the same portal.Transforming PROs data collection withelectronic platformPRO methodologies have wholeheartedly embraced digitaltechnologies to effortlessly collect information on patient’soutcomes in a seamless workflow from recruitmentto analysis. There are many standardized PROs thathave been validated and integrated into electronic datacollection templates. While this reduces the errors andIn China, tech giants are transforming the healthcaremanpower requirements inherent in any manual datasystem with AI. AI is increasingly being used to supportentry and improve administrative and data managementclinical management in many areas such as medicalprocesses for researchers, the accuracy of self-reportedimaging and diagnosis. Faster and more effective optionsdata is still dependent on the patient and biases stillare available to cope with the increasing demand forremain. A technology-driven era of high connectivityhealthcare services and providing accessibility to qualityhas led to the high penetration of smart devices furtherservices in the remote rural areas. Insights generated fromencouraging and enabling the facilitation of PRO studies.iqvia.com 9
The concept of Bring Your Own Device (BYOD) is taking rootand is a viable alternative for PROs data collection. Patientsor subjects can use their own devices, to complete theTable 1: Some methods that add value to the decisionmaking process through patient-centric approachesMETHODSsurvey via a web-based portal or through a downloaded Better alignment of researchmobile app. BYOD allows patients to self-administer thequestionnaire remotely and conveniently while at the sametime, allowing the Principal Investigator access to a widerefforts and resource allocation toPatient ReportedOutcomespool of patients or subjects. Although BYOD has clearliteracy and penetration of smart devices may not be as Richer data to showcaseimprovements in clinical outcomeprioritization of research gapsMultiple CriteriaDecision Analysisto complete the value story ofproducts and services Structured explicit approach tohigh as the European counterparts.Conclusionthe demands of the market Clear identification andadvantages, some challenges in its execution remain to beaddressed, especially in emerging markets in Asia, whereBENEFITSdemonstrate value of products forappraisal committees, cliniciansPatient Preferencesand private patientsAdoption of mechanisms that incorporate thepatient’s voice in healthcare decision makingprocesses in Asia PacificKeeping the human touch at the core of digital healthWith Australia and Taiwan taking steps towardsidea is to understand the patient in order to improveincorporating patient perspectives in their healthcarepatient outcomes, while the challenge is to leverage thedecision making process, the trend is likely to continue toconvenience which technology brings bearing in mindcountries within the region regardless of the maturity ofthe ‘human’ at the center of care. With patients beingthe healthcare system. In a heavily regulated industry suchthe vulnerable consumers in healthcare, empathy is theas healthcare, patient’s voice provides a way to connect withkey element to a good patient experience. After all, thethe end-users of our industry and ensures that they aregoal of healthcare is to improve patients’ health-relatedable to reap the benefits of healthcare innovations (Table 1).While technology is used to expand the access to qualitycare, it should not come at the cost of humanity. Thequality of life. And it is imperative to preserve thehuman touch in our efforts moving forward.Continue the conversation with:Sirinthip Petcharapiruch, sirinthip.petcharapiruch@iqvia.comCallix Wong, callix.wong@iqvia.comJonathan Chua, .9.10.11.12.13.14.15.16.Institute of Medicine (US) Committee on Quality of Health Care in America. “Crossing the Quality Chasm: A New Health System for the 21st Century.” National AcademiesPress (US), 2001. , Christianne L., Robert Greevy, Kenneth A. Wallston, Tom A. Elasy, Lisa Kaltenbach, Kristen Kotter, Robert S. Dittus, and Theodore Speroff. “Patient Centered PrimaryCare Is Associated with Patient Hypertension Medication Adherence.” SpringerLink. Springer US, December 16, 2010. https://doi.org/10.1007/s10865-010-9304-6Thompson, Laura and McCabe, Rose. “The Effect of Clinician-Patient Alliance and Communication on Treatment Adherence in Mental Health Care: a Systematic Review.” BMCPsychiatry. BioMed Central, July 24, 2012. 0.1186/1471-244X-12-87J. F. Scoggins, and Donald L. Patrick. “The Use of Patient-Reported Outcomes Instruments in Registered Clinical Trials: Evidence from ClinicalTrials.gov,” March 25, 2009.https://doi.org/10.1016/j.cct.2009.02.005.E. Vodicka, K. Kim, E. B. Devine, A. Gnanasakthy, J. F. Scoggins, and D. L. Patrick. “Inclusion of Patient-Reported Outcome Measures in Registered Clinical Trials: Evidence fromClinicalTrials.gov (2007–2013),” April 18, 2015. https://doi.org/10.1016/j.cct.2015.04.004.National Institute for Health and Care Excellence. “The Guidelines Manual.” National Institute for Health and Care Excellence (NICE), November 30, J. F. Bridges, Onukwugha, E., Johnson, F., and Hauber, A. “Patient Preference Methods: A Patient-Centered Evaluation Paradigm.” RTI International. ISPOR Connections, 13(6), 4 - 7., 2007.Montarat Thavorncharoensap, Yot Teerawattananon, Sirin Natanant, Wantanee Kulpeng, Jomkwan Yothasamut, Pitsaphun Werayingyong. “Estimating the Willingness to Payfor a Quality-Adjusted Life Year in: CEOR.” ClinicoEconomics and Outcomes Research. Dove Press, January 10, 2013. https://doi.org/10.2147/CEOR.S38062Chang, Chao-Ming. “Patient Involvement In HTA Process In Taiwan”. Presentation, Tokyo, Japan, 2018.“Patient Voice Initiative”. Patient Focused Medicines Development. 2019. -initiative.“An Introduction To Patient Decision Aids”. BMJ 347 (jul23 2): f4147-f4147. 2013. https://doi.org/10.1136/bmj.f4147Sofia Baptista, Elvira Teles Sampaio, Bruno Heleno, Luís Filipe Azevedo, and Carlos Martins. “Web-Based Versus Usual Care And Other Formats Of Decision Aids To SupportProstate Cancer Screening Decisions: Systematic Review And Meta-Analysis”. Journal Of Medical Internet Research 20 (6): e228. 2018. doi:10.2196/jmir.9070Nota, Ingrid, Constance H. C. Drossaert, Heleen C. Melissant, Erik Taal, Harald E. Vonkeman, Cees J. Haagsma, and Mart A. F. J. van de Laar. “Development of a Web-BasedPatient Decision Aid for Initiating Disease Modifying Anti-Rheumatic Drugs Using User-Centred Design Methods.” BMC medical informatics and decision making.BioMed Central, April 26, 2017. doi:10.1186/s12911-017-0433-5Rhodri Evans, Natalie Joseph-Williams, Adrian Edwards, Robert G Newcombe, Patricia Wright, Paul Kinnersley, and Jeff Griffiths et al. “Supporting Informed Decision MakingFor Prostate Specific Antigen (PSA) Testing On The Web: An Online Randomized Controlled Trial”. Journal Of Medical Internet Research 12 (3): e27. 2010. doi:10.2196/jmir.1305Miller, David P, John G Spangler, L Doug Case, David C Goff, Sonal Singh, and Michael P Pignone. “Effectiveness of a Web-Based Colorectal Cancer Screening Patient Decision Aid:a Randomized Controlled Trial in a Mixed-Literacy Population.” American journal of preventive medicine. U.S. National Library of Medicine, June 2011. doi:10.1016/j.amepre.2011.02.019Braun, Alexander, and Niklas Häusle. “China’s Tech Giants Use Internet to Deliver Smart Health Services.” The Business Times. The Business Times, July 18, h-services.10 Patient-centric decision making in the digital age
iqvia.com 11
SummaryINNOVATIVE FUNDING MODELS FOR TREATMENTOF CANCER AND OTHER HIGH-COST CHRONICNONCOMMUNICABLE DISEASESIn a global landscape study, 105 innovative funding solutions were identified as potential solutionsto addressing the funding gap challenge. Results highlighted collaboration and knowledge sharingas the key success factors.GLOBAL LANDSCAPEGlobally, noncommunicable diseases (NCDs) are rising in prevalence,particularly in low and middle income countries (LMICs). NCDs canbe categorized into cardiovascular diseases, diabetes, respiratorydiseases and cancers. 41Mn people die globally from NCDseach year1Management of NCDs requires long term and ongoing therapy, andin the case of cancer—expensive interventions, posing an increasinglyhigh burden of disease to achieve optimal patient outcomes. 75% occur in low middle incomecountries2 97Mn people fell below the povertyParticularly in LMICs, lack of sufficient funding often leaves patientswith the choice between abandoning treatment or facing financialhardship. Despite meaningful efforts within the health system,current traditional funding models will struggle to close the gap.line as a result of out-of-pocket health carespending (2010)3EXISTING CHALLENGESThe funding gap between optimal treatment and available funding continues to widen—a gap notable inLMICs as patient numbers increase. Within this funding gap, key challenges are:Shift in healthcaredelivery needsHigh demand ontraditional fundingLimited access tostandard of careReach of typicalfinancing platformsAgeing populations andincrease of chronic diseaseprevalence compared to acutediseasesPools of funding are stretchedand patients are exposed tohigh out-of-pocket costsResources (equipment,specialists, infrastructure ) aresupporting a higher caseloadDifficulty delivering funding to ademographic that is unable toset up bank accounts/traditional insuranceINNOVATIVE FUNDING MODELSInnovative funding models can be leveraged as part of the solution to address these challenges throughnew means of raising funds and providing alternative financing delivery options. In collaboration, Rocheand IQVIA conducted an in-depth analysis of innovative funding models in a global landscape studycompromised of:Coverage of 5 regions aroundthe world (Africa, Asia, Europe,Latin America, Middle East) aswell as highlighted cases from17 countries123Identification of 105 innovativefunding models, from researchanalysis supported by 32 expertinterviews from government,NGO and industry sector36 showcased examples to enable readers to betterunderstand different possibilities for innovative fundingmodels. Models were found to focus on unlocking newfunds, pooling resources or to target distribution anddelivery of said funds –or a combinationWeb article. “Noncommunicable diseases”. Details of Noncommunicable diseases. Last accessed on January 3rd, 2019Web article. “Cancer” Details of Cancer. Last accessed on January 3rd, 2019Report. World Health Statistics 2019: Monitoring health for the SDGs, The World Health Organization. Last accessed September 24th, 201912 How digital health is adding value to medtech companies’ approach towards patient-centric care
TYPES OF INNOVATIVE FUNDING MODELSGlobally, diverse and innovative approaches are successfully being used to address funding challenges. Below are 4examples from the landscape study report:In Poland, War on Cancer mobile game was createdto raise funds for cancer patients through in-apppurchasing and by targeting young professionalmales, a group considered to be less involved incharity workIn Panama, hard earmarked sin taxon sugar-sweetened drinks is applied,where 75% of the amount collected isdirected to the health sector, and 40%of the total funds are hard earmarkedto target NCDsIn Thailand, 5 leading insurance companiessold microinsurance policies throughconvenience stores to provide low-costinsurance policies for lower income,typically uninsured, populationsAfrican Access Initiative (AAI) uses strategic partnershipsto pool funding and expand access to cancer medicines/technologies by establishing affordable pricing agreementsbetween companies and African governmentsIMPLEMENTATION OF INNOVATIVE FUNDING MODELSThe report analysis of different models identified common key factors that support the long-term success andsustainability of an implemented innovative funding model.Key success factorsTrusted localstakeholdersengaged aspartnersCancer andhigh-cost NCDsmainstreamed asa governmentpriorityPartnershipmodels that arewin-win for allstakeholdersSimple modelsthat minimizeambiguity/simplify paymentsfor patientsLong-termgovernance plansto supportoperationalsuccessCALL TO ACTIONInnovative fundingmodelsInnovative funding models are necessary toaddress gaps and support treatment accessdue to affordability, but alone are insufficientto address the growing burden of cancer andhigh-cost NCDs.Within the broader health system, thefunding gap can be significantly reducedthrough: Broader healthsystem changes Incorporating proven value-based interventionsinto Universal Health CoverageActively engaging in strategic partnerships toimprove outcomes across the patient journeyCustomizing successful global or regionalstrategies to local contextThere is an opportunity for diverse stakeholders to collaborate andshare knowledge to drive funding innovation and change.Financing onsNon-profitorganizationsHealthcare providersCONCLUSION
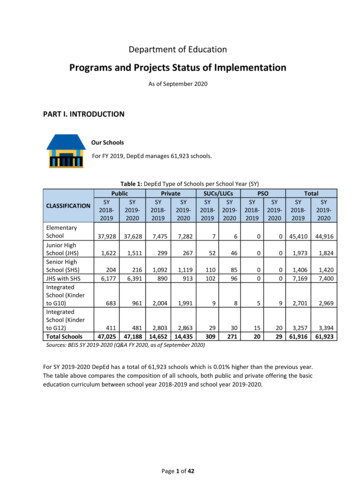
Universal Healthcare Coverage (UHC) in Southeast Asia: An overview and progress 15 Challenges in ensuring access to quality and affordable medicines 17 Importance of providing access to affordable and quality medicines for UHC 20 Future horizons: Improving population health outcomes for UHC 21