Transcription
MMP and HCBS ProviderIntroduction and EducationSessionFebruary 26, 2016
ObjectivesThe objectives of this meeting are to: Increase HCBS Provider understanding ofHealthy Connections Prime Explain HCBS Provider Contracting Outline Claims and Billing processes Introduce HCBS Providers to MedicareMedicaid Plans (MMPs)
Background andTimeline
WHAT IS PRIME?Background New program for seniors age 65 andolder with Medicare and Medicaid Healthy Connections Prime is part ofa national initiative jointlyadministered by CMS and SCDHHS,designed to integrate all the servicesof Medicare, Medicare Part D, andMedicaid under a single MedicareMedicaid plan (MMP) In South Carolina, Medicare-Medicaidplans are called Coordinated andIntegrated Care Organizations(CICOs).
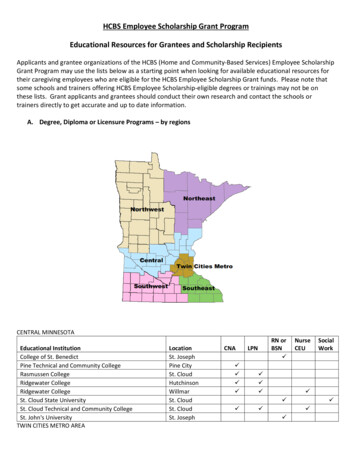
EnrollmentIndividuals may be eligible to enroll if they are: Age 65 or older;Have Medicare benefits;Have full Healthy Connections Medicaid benefits; andAre living in the community.Enrollment PhaseOpen Enrollment( 51,000 eligible enrollees)Passive Enrollment( 12,800 eligible enrollees)Information Ongoing Medicare-Medicaid enrollees choose toparticipate with Healthy Connections Prime Will occur in two initial phases, and is on goingmonthly Eligible enrollees are automatically assigned toa Medicare-Medicaid planHealthy Connections Prime is voluntary. Members may disenroll at any time,and eligible enrollees may choose not to participate.
TimelinePassive Enrollment Timeline*Wave 1Wave 2 Effective April 1, 2016 Effective July 1, 2016 Upstate Region Coastal Region and CLTC WaiverPopulation Projected Eligibles 5,300 Projected Eligibles 7,500 Waiver participants 2,263*Members with comprehensive insurance orwho have previously been passively enrolled intoa standalone prescription drug plan are excludedfrom passive enrollment.Note: Aiken and Dorchester counties are eligible for “choice only” enrollment. In addition, the followingcounties are not participating in Healthy Connections Prime : Lancaster, Horry, Darlington, Sumter and York.
TimelineWave 2 Communications to Members (2016)April 22May 25July 160 Day Noticesmailed30 Day NoticesmailedEarliest Effective Date,New members enrolled!AprilMayJuneApril 14April 25May 28MMP maycontact newmembersNew membersreceive 60 DayNoticesNew membersreceive 30 DayNoticesJuly
Assignment CriteriaPassive Enrollment Intelligent Assignment CriteriaRule 1 –EnrollmentHistoryUses previous 6months ofenrollment historyConsiders howmemberdisenrolled fromprevious plan:Rule 2 – MostFrequentlyUtilized ProviderIdentifies mostfrequently utilizedprovider (MFUP)through historicalclaims dataUses MFUP toassign plan Voluntarily, or InvoluntarilyUses Rule 3 if theMFUPs arecontracted withmultiple plansRule 3 – FamilyHealth PlansAssigns memberto the same planas the otherfamily memberAssigns memberto the plan withthe majority ofthe familymembersUse Rule 4 toassign member tohealth plan, if atie.Rule 4 – HealthRisk ScoreBalance theassignment to theavailable plans inthe county basedon health riskscore.
HCBS Transition
WHAT IS PRIME?How does this impact CLTC waiver serviceproviders?Does not changeChangesUse of PhoenixProvider contractsProvider CredentialingOversight of Waiver CMLTC LOC Initial AssessmentsLTC LOC ReassessmentsSelf-DirectionKeep your waiver participantsPLUSClaims processing andpaymentServe non-waiverindividualsProvider ReimbursementPart of a care team
HCBS Transition2016 Changes SCDHHS will transition the following responsibilities tothe MMPs. Service Plan Approval Monitoring LTC Annual Reassessment Provider reimbursement Provider contracts
HCBS TransitionNewHCBS Service PlanReferral madeto CLTCMember mustmeet bothfinancial andmedicalnecessitycriteriaAny entity (i.e.beneficiary,family,physician, etc.)may make areferralNurseConsultantPerforms levelof caredeterminationCLTC CaseManager IIDevelops initialservice planSends providerchoice list toparticipantand/or primarycontactParticipantselects waivercase managerfrom MMPnetworkWaiver CaseManagerConducts inhome visitwithin 30 daysUpdatesservice plan asnecessarybased uponneeds notaddressed ininitial serviceplan )MMP CareCoordinatorReviews ServicePlanApproves and/ormodifiesupdated serviceplanConducts ongoingmonitoring ofservice planApproves ordisapprovessubsequentmodifications andservice plan changes
HCBS TransitionClaims and Billing Providers will continue to use Phoenix for billing Billing agreement required (to be discussed later) Claims generated based on authorized services Providers are currently paid by the state and payment recoupedfrom each MMP May 1, 2016 - anticipated implementation of claims processing andpayment by MMPs Reimbursement based upon Fee-For-Service rate floor Reimbursement schedule does not change
HCBS TransitionWhy Contract with MMPs?HCBS providers are encouraged to join one or more MMPnetworks. To be a part of the health plan provider network To continue serving members beyond 6 month Continuity ofCare period To receive future referrals for waiver and waiver-likeservices
HCBS TransitionContinuity of Care 6-month continuity of care periodParticipants maintain providers and servicesMaintains service authorization levels for waiver services, unless changein service needsOut-of-network providersreimbursed at currentMedicare and Medicaid feefor-service rates
Prime ProviderAgreement
Provider AgreementPurpose In order for SCDHHS to submit claims to the MMPfor waiver participants, providers need tocomplete a Healthy Connections ProviderAgreement.The agreement must be signed and completedelectronically.The agreement is located in Phoenix ProviderPortal under the “Profile” tab.
Provider Agreement Log into the Phoenix Provider Portal athttps://providers.phoenix.scdhhs.gov/loginClick the Profile tab
Provider Agreement Click the Agreements tab The screen will show the “Healthy ConnectionsPrime agreement waiting to be signed by yourcompany.
Provider Agreement Clicking “Healthy Connections Prime Agreement”displays the document on the screen to bereviewed.After reading the agreement, check the boxstating I agree to the Terms and Conditions.Type the name and title of the person acceptingthe terms and conditions on behalf of theprovider agency
Provider Agreement Click the Sign Agreement button
Provider Agreement To print the signed agreement, click theDownload Signed Copy button.The user will be asked to enter a password.The password is the user’s login ID.Click your web browser’s print button or rightmouse click on the document to print.
Additional Resources
Contact us by email:primeproviders@scdhhs.govOr visit our website at:www.scdhhs.gov/prime FAQsEducational eventsMember storiesProgram dataLatest updatesProvider toolkitAdditional materialsContacts
Questions?
Timeline Wave 1 Effective April 1, 2016 Upstate Region Projected Eligibles 5,300 Wave 2 Effective July 1, 2016 Coastal Region and CLTC Waiver Population Projected Eligibles 7,500 Waiver participants 2,263 Passive Enrollment Timeline* Note: Aiken and Dorchester counties are eligible for choice only enrollment.