Transcription
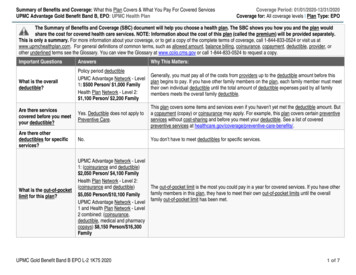
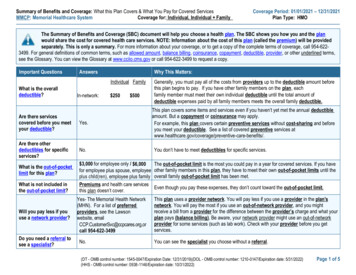
Summary of Benefits and Coverage: What this Plan Covers & What You Pay for Covered ServicesMMCP: Memorial Healthcare SystemCoverage for: Individual, Individual FamilyCoverage Period: 01/01/2021 – 12/31/2021Plan Type: HMOThe Summary of Benefits and Coverage (SBC) document will help you choose a health plan. The SBC shows you how you and the planwould share the cost for covered health care services. NOTE: Information about the cost of this plan (called the premium) will be providedseparately. This is only a summary. For more information about your coverage, or to get a copy of the complete terms of coverage, call 954-6223499. For general definitions of common terms, such as allowed amount, balance billing, coinsurance, copayment, deductible, provider, or other underlined terms,see the Glossary. You can view the Glossary at www.cciio.cms.gov or call 954-622-3499 to request a copy.Important QuestionsAnswersWhy This Matters:Individual FamilyWhat is the overalldeductible?In-network: 250 500Generally, you must pay all of the costs from providers up to the deductible amount beforethis plan begins to pay. If you have other family members on the plan, eachfamily member must meet their own individual deductible until the total amount ofdeductible expenses paid by all family members meets the overall family deductible.This plan covers some items and services even if you haven’t yet met the annual deductibleamount. But a copayment or coinsurance may apply.For example, this plan covers certain preventive services without cost-sharing and beforeyou meet your deductible. See a list of covered preventive services fits/.Are there servicescovered before you meetyour deductible?Yes.Are there otherdeductibles for specificservices?No.You don’t have to meet deductibles for specific services. 3,000 for employee only / 6,000for employee plus spouse, employeeplus child(ren), employee plus familyPremiums and health care servicesthis plan doesn’t cover.The out-of-pocket limit is the most you could pay in a year for covered services. If you haveother family members in this plan, they have to meet their own out-of-pocket limits until theoverall family out-of-pocket limit has been met.What is the out-of-pocketlimit for this plan?What is not included inthe out-of-pocket limit?Will you pay less if youuse a network provider?Do you need a referral tosee a specialist?Yes- The Memorial Health Network(MHN). For a list of preferredproviders, see the Lawsonwebsite, emailCCP.CustomerSvc@ccpcares.org,orcall 954-622-3499No.Even though you pay these expenses, they don’t count toward the out-of-pocket limit.This plan uses a provider network. You will pay less if you use a provider in the plan'snetwork. You will pay the most if you use an out-of-network provider, and you mightreceive a bill from a provider for the difference between the provider’s charge and what yourplan pays (balance billing). Be aware, your network provider might use an out-of-networkprovider for some services (such as lab work). Check with your provider before you getservices.You can see the specialist you choose without a referral.(DT - OMB control number: 1545-0047/Expiration Date: 12/31/2019)(DOL - OMB control number: 1210-0147/Expiration date: 5/31/2022)(HHS - OMB control number: 0938-1146/Expiration date: 10/31/2022)Page 1 of 5
All copayment and coinsurance costs shown in this chart are after your deductible has been met, if a deductible applies.Common Medical EventIf you visit a health careprovider’s office orclinicIf you have a testServices You May NeedLimitations, Exceptions, & OtherImportant InformationPrimary care visit to treat aninjury or illness 20 copay / visitNot CoveredSpecialist visit 50 copay / visitNot CoveredNo chargeNot Covered 50 copayNot Covered 100 copay / testNot CoveredMRI, CT/PET scans require priorauthorization 10 copay / 30 day retailsupply, 30 copay 90 dayretail supply, 20 copay /90 day mail- order supplyNot CoveredNoneNot CoveredNoneNot CoveredIn the event a Tier 1 equivalent medicationis available the member will be responsiblefor a co-pay of 40% (a minimum 50 and amaximum of 150) plus the cost differencebetween the Tier 1 equivalent and the Tier 3medication.Not CoveredOnly covered at MHS pharmacies and theCRx Specialty Pharmacy.Preventive care/screening/immunizationDiagnostic test (x-ray, bloodwork)Imaging (CT/PET scans,MRIs)Generic drugsIf you need drugs totreat your illness orconditionMore information aboutprescription drugcoverage is availablefrom Southern Scriptsat 1-800-710-9341 orsouthernscripts.netWhat You Will PayNetwork ProviderOut-of-Network Provider(You will pay the least) (You will pay the most)Preferred brand drugsNon-preferred brand drugsSpecialty drugs 35 copay / 30 day retailsupply, 105 copay 90day retail supply, 70copay / 90 day mailorder supply40% ( 50 minimum, 150maximum) / 30 day retailprescription, 40% ( 150minimum, 450 maximum90 day retail supply,40% ( 70 minimum, 210maximum) / 90 day mailorder supply40% ( 150 minimum 300 maximum)* For more information about limitations and exceptions, call 954 622 3499.NoneChiropractor: 40 copay/visit (60 visitmaximum)You may have to pay for services that aren’tpreventive. Ask your provider if the servicesyou need are preventive. Then check whatyour plan will pay for.No Charge for Labs.Page 2 of 6
Common Medical EventIf you have outpatientsurgeryServices You May NeedFacility fee (e.g., ambulatorysurgery center)Physician/surgeon feesEmergency room careEmergency medicaltransportationUrgent care If you need immediatemedical attention If you have a hospitalstayCVS Minute Clinic/WalgreensMemorial PrimaryCareHoly Cross UrgentCare CentersMHS Urgent CareCentersMemorial Pembroke24/7 Care Center(Douglas Rd)MDNOW UrgentCareSelected BrowardHealth locationsFacility fee (e.g., hospitalroom)Physician/surgeon feesIf you need mentalhealth, behavioralhealth, or substanceabuse servicesOutpatient servicesIf you are pregnantOffice visitsInpatient servicesWhat You Will PayNetwork ProviderOut-of-Network Provider(You will pay the least) (You will pay the most)Not Covered, except in 250 copayan emergency 0 copayNot Covered 150 copay / visit, 150 copay / visit, waivedwaived if admittedif admitted 50 copay / event 50 copay / eventLimitations, Exceptions, & OtherImportant InformationSome services may require priorauthorization.NoneNoneNon-emergency transportation requires priorauthorization 20 copay / visit 20 copay / visit 20 copay / visit 20 copay / visit 75 (Non-MemorialUrgent Care Center)None 150 copay per day (5day max)Not Covered, unlessadmitted through anemergency room5 day max. Requires Prior Authorization 0Not CoveredNone 20 copay / per visitNot CoveredNone 50 copay / visit 75 copay / visit 75 copay / visit 150 copay per day(5 day max) 150 physician copay /pregnancy* For more information about limitations and exceptions, call 954 622 3499.Not CoveredNot CoveredCopay applicable to first 5 days of eachadmission. Requires Prior AuthorizationNo prior authorization required for initialvisit, but is required thereafter.Page 3 of 6
Common Medical EventServices You May NeedChildbirth/deliveryprofessional servicesChildbirth/delivery facilityservicesHome health careWhat You Will PayNetwork ProviderOut-of-Network Provider(You will pay the least) (You will pay the most) 0Not Covered 150 copay per day (5day max)Not Covered 15 copay / dayNot Covered 20 per dayRehabilitation servicesIf you need helprecovering or haveother special healthneedsIf your child needsdental or eye careCardiac Rehabilitationcovered in FullNot CoveredHabilitation servicesNot CoveredNot CoveredSkilled nursing care 0Not CoveredDurable medical equipment 0Not CoveredHospice services 0Not CoveredChildren’s eye exam 0Not CoveredChildren’s glassesNot CoveredNot CoveredChildren’s dental check-upNot CoveredNot Covered* For more information about limitations and exceptions, call 954 622 3499.Limitations, Exceptions, & OtherImportant InformationNoneCopay applicable to first 5 days of eachadmission. Requires prior authorization.Requires prior authorization. Limited to 60visits per calendar year.Physical therapy, occupational therapy andspeech therapy visits are limited to sixty (60)visits per calendar year.Cardiac rehabilitation is limited to 36 visitsper episode.NoneRequires Prior Authorization; limited to 45days per calendar year.Some services may require priorauthorization. Subject to medical necessityreviewRequires prior authorization; limited to amaximum benefit of 10,000. Limited to lifeexpectancy of less than six months.Limited to one exam per calendar year forcovered children as a preventive service. Aseparate vision plan is available.Not covered under the medical plan.A separate vision plan is available.Not covered under the medical plan.A separate dental plan is available.Page 4 of 6
Excluded Services & Other Covered Services:Services Your Plan Generally Does NOT Cover (Check your policy or plan document for more information and a list of any other excluded services.) Cosmetic surgery Long-term care Routine eye care (adult) Dental care Non-emergency care when traveling outside the Routine foot care Habilitation ServicesU.S. Weight loss programs Private-duty nursing Infertility treatment (diagnosis only is covered)Other Covered Services (Limitations may apply to these services. This isn’t a complete list. Please see your plan document.) Acupuncture Chiropractic care Hearing aids Bariatric surgeryYour Rights to Continue Coverage: There are agencies that can help if you want to continue your coverage after it ends. The contact information for thoseagencies is: the U.S. Department of Labor, Employee Benefits Security Administration at 1-866-444-3272 or www.dol.gov/ebsa, or the U.S. Department of Health andHuman Services at 1-877-267-2323 x61565 or www.cciio.cms.gov.Other coverage options may be available to you, too, including buying individual insurancecoverage through the Health Insurance Marketplace. For more information about the Marketplace, visit www.HealthCare.gov or call 1-800-318- 2596.Your Grievance and Appeals Rights: There are agencies that can help if you have a complaint against your plan for a denial of a claim. This complaint is called agrievance or appeal. For more information about your rights, look at the explanation of benefits you will receive for that medical claim. Your plan documents alsoprovide complete information on how to submit a claim, appeal, or a grievance for any reason to your plan. For more information about your rights, this notice, orassistance, contact: Appeals Coordinator, c/o Community Care Plan 1643 Harrison Parkway, Suite 200, Bldg. H. Sunrise, Florida 33323.Does this plan provide Minimum Essential Coverage? YesMinimum Essential Coverage generally includes plans, health insurance available through the Marketplace or other individual market policies, Medicare, Medicaid,CHIP, TRICARE, and certain other coverage. If you are eligible for certain types of Minimum Essential Coverage, you may not be eligible for the premium tax credit.Does this plan meet the Minimum Value Standards? YesIf your plan doesn’t meet the Minimum Value Standards, you may be eligible for a premium tax credit to help you pay for a plan through the Marketplace.Language Access Services:Spanish (Español): Para obtener asistencia en Español, llame al 954 622 3499.To see examples of how this plan might cover costs for a sample medical situation, see the next section.PRA Disclosure Statement: According to the Paperwork Reduction Act of 1995, no persons are required to respond to a collection of information unless it displays a valid OMB controlnumber. The valid OMB control number for this information collection is 0938-1146. The time required to complete this information collection is estimated to average 0.08 hours per response,including the time to review instructions, search existing data resources, gather the data needed, and complete and review the information collection. If you have comments concerning the accuracyof the time estimate(s) or suggestions for improving this form, please write to: CMS, 7500 Security Boulevard, Attn: PRA Reports Clearance Officer, Mail Stop C4-26-05, Baltimore, Maryland21244-1850.* For more information about limitations and exceptions, call 954 622 3499.Page 5 of 6
About these Coverage Examples:This is not a cost estimator. Treatments shown are just examples of how this plan might cover medical care. Your actual costs will be differentdepending on the actual care you receive, the prices your providers charge, and many other factors. Focus on the cost-sharing amounts(deductibles, copayments and coinsurance) and excluded services under the plan. Use this information to compare the portion of costs you mightpay under different health plans. Please note these coverage examples are based on self-only coverage.Peg is Having a BabyManaging Joe’s Type 2 DiabetesMia’s Simple Fracture(9 months of in-network pre-natal care and ahospital delivery)(a year of routine in-network care of a wellcontrolled condition)(in-network emergency room visit and follow upcare) The plan’s overall deductible 250 Specialist copay 50 Hospital (facility) copay 150 per day(5 day max) Other coinsurance0% The plan’s overall deductible 250 Specialist copay 50 Hospital (facility) copay 150 per day(5 day max) Other coinsurance0% The plan’s overall deductible 250 Specialist copay 50 Hospital (facility) copay 150 per day(5 day max) Other coinsurance0%This EXAMPLE event includes services like:Specialist office visits (prenatal care)Childbirth/Delivery Professional ServicesChildbirth/Delivery Facility ServicesDiagnostic tests (ultrasounds and blood work)Specialist visit (anesthesia)This EXAMPLE event includes services like:Primary care physician office visits (includingdisease education)Diagnostic tests (blood work)Prescription drugsDurable medical equipment (glucose meter)This EXAMPLE event includes services like:Emergency room care (including medicalsupplies)Diagnostic test (x-ray)Durable medical equipment (crutches)Rehabilitation services (physical therapy)Total Example CostTotal Example CostTotal Example CostIn this example, Peg would pay:Cost SharingDeductibles 12,700 250In this example, Joe would pay:Cost SharingDeductiblesCopayments 400Coinsurance 0What isn’t coveredLimits or exclusionsThe total Peg would pay is 60 710 5,600 2,800 250In this example, Mia would pay:Cost SharingDeductibles 250Copayments 800Copayments 500Coinsurance 0Coinsurance 0What isn’t coveredLimits or exclusionsThe total Joe would pay is 20 1,070What isn’t coveredLimits or exclusionsThe total Mia would pay is 0 750The plan would be responsible for the other costs of these EXAMPLE covered services.Page 6 of 6
MHS Urgent Care Centers Memorial Pembroke 24/7 Care Center (Douglas Rd) MDNOW Urgent Care . 50 copay / visit 75 copay / visit 75 copay / visit 75 (Non-Memorial Urgent Care Center) None If you have a hospital stay Facility fee (e.g., hospital room) 150 copay per day (5 day max) Not Covered, unless admitted through an .