Transcription
MADE TO LEAD: EMPOWERINGA HIGHLY COMPETENT ANDENGAGED NURSE WORKFORCEStandardized education and strong frontline leadershelp hospitals overcome top nursing challengesIN PARTNERSHIP WITH
Made to Lead: Empowering a HighlyCompetent and Engaged Nurse WorkforceStandardized education and strongfrontline leaders help hospitalsovercome top nursing challenges.High-performing healthcare organizations depend on awell-educated, engaged nurse workforce to deliver evidence-based care that meets increasingly strict patient safetyand quality guidelines. Yet, many still struggle to attractand connect with nurses in ways that motivate them to trulybe a part of the organization. “One of the top challengesfor improving engagement, retention, and recruitment iscreating and sustaining a culture that empowers nursesto practice clinical excellence,” says Tammy Purcell, MSN,RNC-OB, clinical nurse executive at Elsevier.Organizations that excel at engaging and retaining nursesunderstand and address what drives nurses, both personally and professionally. “They consistently create astimulating, supportive, and professional work environment while helping nurses build a successful career path,”says Purcell. Achieving these goals requires hospitals to usea variety of resources and tactics. In our recent research,respondents indicated two key tactics: standardizingevidence-based education and competency management,while developing strong frontline nurse leaders.ENGAGING NURSES THROUGHEVIDENCE-BASED CONTINUINGEDUCATIONA recent HealthLeaders Buzz Survey polled 129 seniorexecutives and clinical leaders, asking how nurse educationand leadership development are helping them build anengaged nurse workforce. Survey respondents say overall,evidence-based continuing education and strong frontlinenurse leaders play critical roles in improving nurse engagement, recruitment, and retention.2“When nurse leaders create theright environment and department culture in which nurses waitin line for a job opening, we couldbegin to see significant changes innurse retention and recruitment.”—Tammy Purcell, MSN, RNC-OB, clinical nurseexecutive at ElsevierRespondents say they are deploying several tactics toimprove nurse retention, including offering the following:standardized orientation and onboarding programs fornew nurses (76%), in-person ongoing nurse education(60%), online continuing education (53%), and compensation packages (53%). Additionally, close to half say theyare developing strong frontline leaders to grow retention.Notably, compensation packages rank lower than standardized orientation and onboarding programs, as well asin-person education, when it comes to retaining nurses.“This is because orientation, training, and education are aninvestment in a nurse’s career development and long-termsuccess,” says Alison Mason, MS, RN, national director ofclinical quality informatics at Englewood, Colorado–basedCatholic Health Initiatives (CHI). “Ultimately, when youTAMMY PURCELLMSN, RNC-OBclinical nurse executiveElsevierwww.elsevier.com
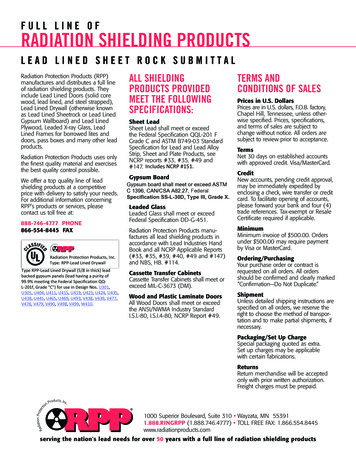
help nurses become betterpractitioners, you’re givingthem the ability to advancetheir careers and make moremoney,” she notes. “There’smore staying power to that.”Nurses also expect education programs that are highlyprofessional and offer themost current clinical information and evidence-basedcontent. To that end, Purcellsays healthcare organizationsare becoming more consistent in providing standardizededucation and competencymanagement. “We have alsobegun to see this consistencymove outside of the four wallsof the hospital and into theambulatory space, and I expectthis trend will continue.”Improving Nurse Retention What resources/tactics does yourorganization currently use to improve nurse retention?Standardized orientation and onboardingprograms for new nurses60%Ongoing nurse training (in-person)Online continuing education courses to supportclinical practice/professional development53%Compensation packages (e.g., tuitionreimbursement/retention bonuses)53%Development of strong frontline nurse leaders47%Shared governance47%Performance management tools to track and manage nursegoals, assess competencies, and monitor improvement44%36%Nurse externships/residencies24%Nurse mentorship/ambassador programAt CHI, nurse engagement and professional developmentare important goals, says Mason. “Nurse engagementmeans a nursing workforce that’s happy in what they’redoing; they’re satisfied, energetic, and dedicated toboth their profession and the organization,” she says.“Increasingly, today’s nurses want to be viewed as contributors and professionals.” Evidence-based practice advancesprofessionalism in nursing, she continues. “Therefore, asleaders, we have an obligation to make certain our education and competency programs are in alignment withnursing evidence.”Since 2009, CHI has offered an online evidence-basednursing procedure and practice resource, helping to reducecare variation across its enterprise of over 100 hospitalslocated in 18 states. The nonprofit started with one maindatabase for all its hospitals, eventually adding severalmore stand-alone databases that are synced across thesystem, says Mason. “There’s an expectation we will usethis resource and identify it as our source of truth for evidence-based practice,” she says. “Our belief is it shouldn’tmatter where you walk in the front door; you shouldreceive evidence-based care.”376%Other9%Base 129Multi-responseMason says providing evidence-based education at the pointof care has led to powerful results at CHI, including strengthening nurse and patient engagement. “It allows nurses toshow that they are using the most current evidence as theywork with their patients,” she says. “It also has a downstreameffect of improving patient quality and outcomes.”Mason points to a recent situation involving a new nurseat a CHI critical access hospital who was struggling to perform a patient procedure. The nurse was working the nightshift and needed to perform a procedure she was checkedoff as competent in, but had not actually done before onALISON MASON,MS, RNnational director of clinicalquality informaticsCatholic Health Initiativeswww.elsevier.com
DELIVERING A HIGH-VALUEEDUCATION PROGRAM TO PROMOTEA CULTURE OF SAFETY AND QUALITYa patient. “She was able to pull up our online skills andprocedures resource, watch a demonstration video, readthrough the procedure, and then perform that procedurewith confidence and a good outcome,” says Mason.Top Three Nurse Training Program Priorities What are your organization’stop three priorities when developing a nurse training program?72%Promote a culture of safety and qualityImprove retention rates43%Promote consistent, standardized care43%41%Maximize nurse engagement32%Drive evidence-based practice27%Develop top clinical talent12%Improve nurse onboarding speed and qualityDecrease readmission rates9%Ensure a higher level of compliancewith accrediting organizations7%6%Reduce administrative overhead2%OtherBase 129Select threeMeasuring Nurse Clinical Competence How does your organizationtrack and measure the clinical competence of nurses?81%Completion of competency checklists53%In-house resources (home-grown solutions)47%HCAHPS or other CMS survey43%Learning management system (LMS)36%National Database of Nursing Quality Indicators (NDNQI)Knowledge inventory tools—online benchmarking/training tool to identify and remediate knowledge gapsOtherBase 129Multi-response421%8%According to the buzz survey,respondents say their top nurseeducation program prioritiesinclude promoting a cultureof safety and quality (72%),improving retention rates(43%), promoting consistent,standardized care (43%), andmaximizing nurse engagement(41%). “It is no surprise that thetop priority of nurse educationprograms is to promote a culture of safety and quality,” saysPurcell. These are evergreenareas healthcare organizations are constantly seeking toimprove. “Improving retentionrates and maximizing nurseengagement could supportthese efforts,” she adds.When it comes to tracking andmeasuring nurse clinical competence, respondents say theyuse several resources, includingcompetency checklists (81%),in-house resources (53%),HCAHPS or another CMSsurvey (47%), and a learningmanagement system (43%).Purcell agrees that competencychecklists are one of the mostvaluable tools used in measuring nurse competence. “It is asingle source of truth for a specific competency. When usedwith a learning managementsystem, competency checklistsbecome an even more powerful way to measure nurseclinical competency and assignremediation,” she observes.www.elsevier.com
“The electronic competency checklist is an importantcomponent in the total learning picture, but we need tobe creative in how we use it,” says Mason. “I do think thatthe use of a simulator model is most likely to be the mosteffective tool in measuring competence, and the checklistis a component of that. But I think when you talk aboutengaging the nurse, simulators do that. It’s somethingthat appeals to younger nurses. It’s what they use inschool, so it is what they expect when they come out inthe workplace.”EMPOWERING FRONTLINE LEADERSTO ENGAGE NURSESWhile education sets the foundation for a successful nursing program, strong, proactive frontline nurse leaders playimportant roles as well. The HealthLeaders Media 2017report Nursing Excellence: Leadership Development, Culture,and Retention identified nurse retention, recruitment, andengagement as the top three nursing challenges and concluded, “Without strong frontline leaders, many retentiontactics will be difficult to implement and sustain.” Purcellconcurs. “When nurse leaders create the right environmentand department culture in which nurses wait in line foran opening, we could begin to see significant changes innurse retention and recruitment,” she says.Healthcare leaders say their main reasons for developing and supporting frontline leaders include improvingefficiency and quality of patient care (73%), maximizingnurse engagement (60%), driving retention and recruitment (44%), and having clinical experts who will driveevidence-based practice (38%).“While Baby Boomers are morelikely to stick around in hopesthat things might change, millennials most definitely will leave.”—Alison Mason, MS, RN, national director of clinicalquality informatics at Catholic Health Initiatives“The development of frontline nurse leaders should bea key initiative for today’s healthcare organization,” saysPurcell. “Yet it is often entirely overlooked or marginalized.Without a robust development program, we are not doingthe best we can to encourage retention, engagement, andprofessional development.”Purcell says frontline nurse leaders should model behaviorsthat show their passion for nursing, including promoting clinician improvement;advocating for standardized,evidence-based care acrossRole of Frontline Nurse Leaders Our organization develops andthe continuum; and drivingsupports frontline nurse leaders because they .patient safety and qualityoutcomes. “They need to beDrive improvements in efficiencyopen communicators who are73%and quality of patient careunafraid to question the statusMaximize nurse engagement by creating a60%quo,” she says.positive and supportive work environment44%Help drive nurse retention and recruitment effortsServe as clinical experts that driveevidence-based practice38%Evaluate nurse performance and monitorunit-based performance indicators21%20%Facilitate education and orientationOther5%Base 129Select three5Nurse leaders also mustbe astute in engaging newnurses, especially millennials, who comprise a growingpercentage of the nurse workforce, says Mason with CHI.Millennial job satisfactiondiffers from that of othergenerations. They want awww.elsevier.com
stronger work-life balance, a well-structured orientation,involvement in decision-making, and engagement inchange processes. “While Baby Boomers are more likely tostick around in hopes that things might change, millennialsmost definitely will leave,” says Mason.NURSE LEADER EDUCATION ANDDEVELOPMENT STRATEGIESPurcell says it is critical to support frontline nurse leadersthrough evidence-based online continuing education.“Without it, we risk veering off track and simply educating others the way it has ‘always been done,’ regardless ofwhere that methodology came from, rather than basingour education and actions on what the evidence proves isbest.” This approach also ensures new nurse leaders arecreating a standardized foundation of knowledge basedon research.Nurse leader development programs should also includeboth classroom and independent learning opportunities,says Purcell. Development opportunities such as robusttuition reimbursement for advanced degrees, shadowingwith experienced clinical leaders, nurse leadership conferences, and outside networking opportunities can all beused to help groom frontline nurse leaders as well.A learning management system combined with onlineleadership and professional development courses is alsoimportant in helping a direct care nurse advance into aleadership role. Learning management systems make iteasy for organizations to deploy continuing educationcourses to effectively orient, educate, and develop specificcompetencies for new nurse leaders, while tracking andidentifying knowledge gaps.CHOOSING A NEW PATHAs healthcare organizations develop nurse educationprograms, they must focus on advancing important retention, engagement, and professional development goals.“Approaches such as a sign-on or retention bonus haven’t proven to be all that effective,” says Purcell. “Nurseswant to work for a professional, inspiring, and authenticorganization that gives them superior educational andmentorship opportunities. Learn what your nurses want inan education program and start to create new approaches.”It’s also time to use technology more strategically to standardize education programs and develop new efficiencies,she adds. Finally, when it comes to nurse retention, recruitment, and engagement, “don’t underestimate the power ofleadership development programs, because without strongnurse leaders, it will be difficult for hospitals to makeimprovements in these areas.”About Elsevier Learning and Competency Management SolutionsElsevier is a leading provider of clinical solutions — delivering performance management, professionaldevelopment, skills training, and knowledge acquisition tools to help your organization develop, retain,and maintain a high performing engaged team. This ensures top performance in patient care, whilehelping your clinicians build a successful career path.LEARN MORE ON ADDRESSING YOUR TOP NURSING CHALLENGES WITH ELSEVIER.6Produced by HealthLeaders Custom Solutions, H3.Group
A recent HealthLeaders Buzz Survey polled 129 senior executives and clinical leaders, asking how nurse education and leadership development are helping them build an engaged nurse workforce. Survey respondents say overall, evidence-based continuing education and strong frontline nurse leaders play critical roles in improving nurse engage-