Transcription
GRADUATE PROGRAM IN PUBLIC HEALTHSPRING/SUMMER 2020 – Issue 14The Director’s ColumnDr. Nils Hennig, Program DirectorI hope this issue of the Scoop findshealth education, practice and leadership is during this pandemic.you healthy and safe. These areI could not be more grateful to continue training our studentshistoric times for Public Health. Newthis term.York City and Mount Sinai has beenright in the epicenter. I have never beenmore proud of our students, facultyand staff than in their response to theCOVID-19 pandemic. Whether throughclinical care, research or volunteering,I am thankful to you for all your efforts.Our students have organized into taskforce teams working in the followingareas: PPE, pharmacy, telehealth, administrative, operations, labs, andmorale. Our students have become an essential part of the supportsystem Mount Sinai needs to save lives and care for the communitiesit serves. Our faculty is on the frontline of diagnostic testing, vaccinedevelopment, epidemiologic studies, and the development and rapidimplementation of therapeutics. It is extremely inspiring to see howthe community at Mount Sinai is coming together for an extraordinaryresponse. In our program I see an unwavering dedication to theIn the months to come we also have to have an honest look atthe failures which brought us to the current situation. The WorldHealth Organization has been warning for many years thatinfectious diseases are spreading more rapidly than ever beforeand new infectious diseases are being discovered at a higherrate than at any time in history. SARS, MERS and Ebola are just afew examples from which we could have learned during the mostrecent years. Instead, initially Wuhan authorities covered up thecurrent outbreak, ordered to stop tests, destroy samples, suppressthe news, and silenced the doctors who raised early concerns.The Trump administration’s initial response was characterized bymissed warnings, conflicting messages, and broken promises. TheWhite House, through some combination of ignorance, arrogance,and incompetence, failed to heed the warnings of its own experts.Even the surgeon general and chief medical officer for the UnitedStates downplayed the coronavirus threat, pointing out that “friedpublic’s health. We are all reminded how important the role of publiccontinued on page 5Student Leadership: COVID-19 ResponseThis Spring has been especiallychallenging. This article recognizesjust some of the work that our studentshave done related to COVID-19 reliefefforts in March and April 2020. IcahnSchool of Medicine at Mount Sinaistudents have shown the capacitytaken action, offer support, and servetheir communities during New YorkCity’s response to this pandemic.A Coalition of Student VolunteersThe COVID-19 Student WorkForce isa student-led workforce of over 500medical and graduate students fromthe ISMMS, addressing COVID-19specific needs throughout the MountSinai Health System in order toalleviate burdens on the healthcaresystem. The group operates taskforces encompassing 6 areas:Pharmacy, Administrative Services,HospitalOperations,Telehealth,Labs, and Morale. The WorkForcecollaborates with school and hospitalleadership to assist in filling variousneeds, and the volunteers have madean impact by supporting the hospitalstaff and researchers, at all levels,to contribute to patient care and thecombating of the spread of COVID-19.- Rohini Bahethi, MD Candidate,COVID-19 Student WorkForceCo-LeaderI have been volunteeringwiththeStudentWorkForce’s Patch 24Telehealth project. Inthis role, I have beenalleviating call volumeby taking calls fromacross the Mount Sinaisystem and patchingthem through to theappropriate palliativecareattendingphysicians and fellows.– Brittney Parillon,MPH Candidate
Members of the COVID-19Student WorkForce teamedup to move dozens of highflow oxygen machines froma warehouse to a stagingarea,thenassembledand prepared them to bedelivered to affiliate hospitalsthat same day. Volunteer MitiSaksena, MSCR Candidate,poses with a cart of supplies.Picture from AlexandraAgathis, MD Candidateand Shravani Pathak, MDCandidate.I worked with the NYCDOHMH located at the JavitsNew York Medical StationCommand Center. I 9 positive patients.I also communicated withhospitals throughout the fiveboroughs to intake COVID-19positive patients from theirfacilities to either JavitsNew York Medical Stationor USNS Comfort hospitalship. Now, I am a laboratorycoordinator working onimplementing serial testingof nursing home residents forCOVID-19 throughout NYC.- Rebecca Burns, MPH2Ivolunteeredalongsidemedical and nursing studentsin the pharmacy departmentat Beth Israel Hospital. Ihelped refill the supply ofessential medications forCOVID-19 patients, backfilledthesecondarysupplymedications that we wererunning low, and assisted withinventory management.– Anne Loftus, MPH CandidateI am volunteering at theNYC DOHMH in the HealthSystems and Support Branchwhere I am supporting workto surge and maintain healthcare access. As a physician,I am reviewing the medicalrecords of people detained inICE detention centers to helprelease those with high-riskhealth conditions. Finally,I am organizing a groupof physicians to work onadvocacy toward a strongerpublic health response thataddresses structural inequityand racism.– Betty Kolod, MD, MPHCandidateDuring the past few weeks, Ihelped set up the Samaritan’sPurse patient care tentsin central park. I have alsobeen working with SinaiInpatient COVID teams tocontact family members ofhospitalized patients andupdate them on the statusof their loved ones care andanswer whatever question orconcerns they may be having.– Aisosa Omorogbe, MDMPH CandidateTelehealth: Optimizing Care for More and More UsersTelehealth is a means of providingpersonalized, secure on-line testresults,messaging, and other services,using telecommunication technology.Telehealth has seen a drastic increasein the number of users, and as part ofthe Student WorkForce, I help newlydischarged patients and their proxiessign-up for the MyChart telehealthplatform over the phone. I have had theprivilege of encountering some wonderful individuals and familieswho were not aware of these services and benefitted greatly. Onesuch example was a mother of 2 who also serves as a patient-proxyfor 3 family members living in different boroughs. With telehealth, shehas been better able to manage the care of her relatives alongside thenew home-schooling requirements. My public health training helpedme identify and bridge the communication gaps with many patientsand their families. This volunteer role is now transitioning to a pilotprogram with the help of the nursing staff and clinical social workers.– Tania Chen, MPH CandidateThe East Harlem Health Outreach Partnership is a student-runfree clinic dedicated to the healthcare of underserved patients inthe Mount Sinai neighborhood. As part of the student leadershipteam, I am helping to implement a telehealth program that allowspatients to continue to receive time-sensitive primary care fromvolunteer Mount Sinai physicians and students, and that servesas a bridge to COVID-19 prevention and outreach. Adaptingthis role to the unique needs of the current pandemic has beenan instructive and meaningful experience. Above all, it hasreinforced my conviction that our world cannot advance withoutattaining universal health coverage and creating preferentialoptions for those who have been excluded from the traditionalhealth system. For all the suffering that it has generated, theCOVID-19 crisis urges us to transform our interconnectednessfrom a vulnerability into a strength through more equitable healthpractices, prioritization of vulnerable groups within society, andheightened focus on population and preventative health.- Esha Bansal, MD-MPH Dual Degree CandidateResearch SupportI am volunteering for a non-concurrentcohort study that falls under qualityimprovement analysis protocols forCOVID positive patients in The MountSinai Hospital. The goal of the study is tosee if current treatments are working. Myrole involves reviewing patient charts forkey patient information including durationof intubation and time spent in intensivecare so that we can study the effects ofthe drug Tocilizumab on COVID patients.Dr. Stephanie Factor is leading the groupof students assisting in this work.– Adrienne Dean, MPH Candidate
Public Health AdvocacyThese times of crisis areexactly when our rofessionals must be putinto practice. I have had theprivilege of contributinginmanyways,fromexpanding patient access totelemedicine to sinpandemics.Notably, I have collaboratedwith engineers, physicists,and biomedical scientistsacross the country todevelop a way for hospitalsto use existing infrastructureto facilitate UV irradiationof PPE for decontaminationand reuse. Most recently,I have been working onSinai’sconvalescentplasma transfusion andTocilizumab clinical trials todetermine if these are viabletreatments. Specifically, wehave created a seamlessprocess for plasma donationfrom recovered COVID patients and set up theworld’s largest convalescentplasma transfusion program.Our current efforts seekto automate longitudinalmonitoringofpatients’health outcomes and tounderstand the efficacyof this novel treatmentfor COVID.- Charles Sanky, MPH,MD CandidateI’ve been doing a lot of socialmedia chats, putting out blogposts and creating videos tocreate awareness for whywe need to practice socialdistancing and consider theimmunocompromised, elderly,and other high-risk individualsduring this time. I did anInstagram Live with News 12 NewJersey to explain what it meansto be immunocompromised andhave invisible illnesses duringthe pandemic. I also did anInstagram Live with a renownedgastroenterologist on how tomanage Crohn’s and ulcerativecolitis from a distance duringthis pandemic, and a FacebookLive with the Crohn’s andColitis Foundation on Copingwith Anxiety and Stress Duringthe Pandemic. As a patientinfluencer, I’m working with theAmerican GastroenterologicalAssociation to bring guidanceforward to patients and theircaregivers during such a difficulttime. Recently, I did a video withthe patient advocacy companyInspire for their #KeepUsAllSafecampaign. There’s a lot moreI’m working on, including blogposts of patients who haverecoveredfromCOVID-19and stories of internationalpatients and what they’re goingthrough with the pandemic.– Tina Aswani Omprakash,MPH CandidateTina is a minority healthadvocate and MPH studentsharing her experiences as animmunocompromisedpatientduring COVID-19. Find her workon ownyourcrohns.com andfollow @ownyourcrohns for moreinformation.I’ve been helping by assistingpatients in creating MyChartaccounts for telemedicineappointments, and I’ve beenbabysitting for a physicianwho was reassigned to workwith COVID patients and can’tbe home with her four yearold son.– Jordan Francke, MD, MPHI have been volunteeringwith the Mount SinaiHuman Rights Program tosend groceries and basicmedical items to clients.Their clients are individualswho are seeking asylum inthe United States and haveexperienced human rightsabuses or torture in theircountries of origin. Given thecurrent political climate anduncertainty, these individualsare especially vulnerable tofood insecurity. I have alsobeen volunteering with theStudent WorkForce. At first, Iwas helping The Mount SinaiHospital contact the familymembers of COVID patientswith daily updates, but nowwe’re starting to focus onMount Sinai patients whohave been identified as atrisk patients for drug andalcohol abuse. Many of thesepatients have gone withoutproperharmreductioneducation and resourcesdue to the pandemic. Thus,we provide a telehealthtrainings about naloxone incoordination with mailingNarcan kits.– Sanjana Inala, MPHI connected with GrowNYC,a nonprofit focused onimproving NYC’s quality oflife through environmentalprograms. I volunteer withtheir Fresh Food Box programto hand out fresh producefrom local farms to familiesin Brooklyn. I have also beenrecently hired as a COVID-19contact tracer for NYC Health Hospitals.– Dijon Parker, tainty, and increaseddepression, anxiety, andother mental health issues.I decided to join the CrisisText Line which helps guidetexters through a currentmental or emotional crisisthey might be going through.If anyone is going througha crisis during this time, bigor small, text SHARE to 741741. I have also joined theStudent Morale Task Force’sPhone-Based Well-BeingResource at Mount Sinai.This phone line is open toall Mount Sinai memberswho need help navigatingMount Sinai’s well-beingresources such as therapygroups, childcare, carpool ortransportation, etc.– Cristina Liriano Cepin,MPH33
New York Eye and Ear Infirmary, a Long-Term PartnershipOver the past 5 years, a number of ISMMS students have completed their MPH Applied Practice Experience requirement by interning atNew York Eye and Ear Infirmary of Mount Sinai (NYEE). The Applied Practice Experience (APE) is an integral part of a student’s learningexperience in a public health setting. Below are interviews with ISMMS alumni and current MPH candidates.Alexandre Ly van manh, MPH, 2016In Fall 2015, while working as a researchcoordinator, I saw an opportunity toconnect with the New York Eye andEar Infirmary (NYEE) Ambulatory CareServices leadership and interviewed withthe APE over the years, but also theand pairing transparency about your goalsProgramsupportwith an ambition to make an impact canISMMS students and help them create newyield promising results. Recognizing theopportunities within or beyond Sinai.benefits of a team-oriented collaborativeadministratorswhoapproach to problems was also critical toDominique Pean, MPH, 2018my experience.both the division director and the practiceWhat would you like students to knowmanager. In parallel, the Graduate Programabout the NYEE APE?in Public Health staff supported me in theCompleting the APE at NYEE is a uniquecreation of my project and voilà: the NYEEexperience that can support your growth asAPE was born.a budding public health professional. This isThe exciting part of the APE was thea chance to apply what you have learnedexposure to leadership and seeing theduring class in a real-world setting and canimplications for initiatives and operations.be a springboard for many other careerThe team helped me develop my “voice”opportunities. The NYEE APE providedby asking for my insights as we discussedme with an environment that cultivatedpotential solutions to implement. However,mythe most meaningful part of this APEindependent thinking, and guided mewas the personal bond I created with thetoward the completion of a very gratifyingAmbulatory Care leadership.practicum experience.After my APE ended, I saw a need forthe Ambulatory Care team to fill my roleand at the same time, I wanted to sharemy experience with other students. TheGraduate Program in Public Health staffprofessionalgrowth,encouragedAnaika Azimyt, MPH, 2020Dominique Pean and APE Preceptor JohannaSica, RN, MSN, ANP, CEN on the last dayDuring my time at NYEE, my mainof APE.projectconsistedofmeasuringthepatient volume for appointments usinghelped refine the details and we welcomedMy Applied Practice Experience at NYEEour first intern in Summer 2016. The NYEEMeditech, a software that tracks the totalAmbulatory Care Services focused onAPE has now been running several yearsnumber of appointments booked, missed,implementing a POD system, a team ofand our interns have become an essentialcancellations and no shows. With the data,one attending physician, two residents,support for the Ambulatory Care ServicesI determined which days had higher noone registered nurse, and one nursing aideleadership, from working with data toshows or cancellations and, as a team, weworking as a team and assigned to seehelpingtried to understand the factors involved andspecific patients.find ways to add or reduce our ambulatorywithimprovementprocesses.As healthcare keeps evolving towards apatient centric model, there is a need tokeep enhancing strategies and operationswithin Ambulatory Care Services and anopportunity for MPH students to be partof this effort. The success of the NYEEAPE can be attributed not only to thetalented individuals that have completed4While working at NYEE, the most compellingcare services.lessons I learned were the importanceWhat are you learning through your workof diligence in systems evaluation andat NYEE?the value of self-direction to accomplisha goal. Being proactive in pursuing newIn my time at NYEE, I learned how toobjectives and having a supportive mentoreffectively work on an operations-basedallowed me to succeed in ways I couldn’tteam within a healthcare system. Thishave imagined. Communication is crucial,internship gave me the confidence and
tools I needed to understand and succeedprocessesamong the many tiers and different levels ofproviding quality care.grow in the Mount Sinai community.A few weeks into my APE, I was not onlyThe skilled Ambulatory Care leadership teamexposed to the many moving parts of NYEE’sare incredibly talented professionals and careoutpatient Eye and Ear clinics, I also feltdeeply for their patients - which made thisthat my contributions made an impact. Theexperience all the more inspiring and affirmedprojects that we worked on were discussedthat I am on the right career track!leadership and organization that exist in theclinic setting.Katie Maguire, MPH Candidate 2021I initially chose to pursue my APE at NYEEbecause I was looking for more exposurein the healthcare management field. Iwanted to understand more about whathappens behind the scenes in ambulatorycare settings and understand the thoughtandstrategyinvolvedinand implemented almost immediately. Ifelt that I was able to be a part of importantconversations, and I had never felt thatbefore. My APE was a wonderful experiencein which I could directly apply my publichealth training, learn from accomplishedhospital administrators, and continue toMy advice to future students interningat NYEE is to be creative and confident.NYEE Ambulatory Care Services is agreat learning environment where newperspectives are welcome.The Director’s Column (continued from page 1)food” and “sitting on your couch” were more likely to lead to yourimagine an end to racism and oppression without a clear break anddeath. Locally, the Governor of New York State and the Mayor of Newsystematic change. The Graduate Program in Public Health at theYork City promised widespread testing and contact tracing after theIcahn School of Medicine at Mount Sinai is committed to anti-racisminitial patient tested positive for SARS-CoV-2 in New York City, butand health equity. It is our social responsibility as both membersthat did not happen. Unfortunately, the list of missed opportunities isof society and public health professionals to tackle these systemslong. In general, countries or parts of a country where the responseand push back against racism and bias. Achieving justice requiresto the COVID-19 pandemic is guided by science and public healthaction, not just words. Uprising brings visibility to a movement. Weexperts, are faring much better with lower infections and mortality.stand in solidarity with those campaigning for racial justice and anThe point of looking at mistakes made is not to point fingers butend to all forms of oppression.to avoid them next time and learn for the future. The GraduateOur program pledges to accelerate our commitment to addressProgram in Public Health at the Mount Sinai School of Medicineracial injustice by teaching skills to advocate for the essentialis part of this learning process. Here, our students are acquiringpublic health values of compassion, empathy, justice, and equity,the skills to implement best public health practice and prevent theby advancing research on the structures that shape healthnext pandemic. One of the things we need to learn from the currentinequities and applying that knowledge into practice. We will workCOVID-19 pandemic is that we have to invest in our public healthwith community partners to model the behaviors and values thatinfrastructure, in science, and in global surveillance so things like wewe must demand of our national leaders and those who serve inare experiencing right now will never happen again.law enforcement. We will continue to support the recruitment andThese are very difficult times, not just because of COVID-19, butbecause we are brutally confronted by the inequitable and unjustretention of a diverse group of faculty, students, and staff to achieveinclusive excellence.systems built into the structures of our society. The more we learnIn the end, achieving a more just world depends on more thanabout COVID-19, the more we note the disproportionate impact it hasstatements and slogans. As an academic public health community,on communities of color, which are also burdened by the economicwe recommit to our deeply held tenets of public health: human rights,pain caused by the pandemic and which lack the resources tosocial justice, and health equity. The Graduate Program in Publicabsorb the loss of jobs and income that is currently reverberatingHealth at the Icahn School of Medicine at Mount Sinai will never beacross the nation. We witness example after example of thesilent on racial injustices. We will use our platform to advance ouregregious discrimination that many of our fellow citizens face daily,mission of improved health for everyone, everywhere.most recently evidenced in the death of George Floyd at the handsof Minneapolis police officers. The origins of America’s unjust racialorder lie in the institution of enslavement, and for me it is difficult toI might not see most of you on campus for a while. Until then,remember to seek uplift. Be cognizant of those in need. Stay safe, stayin touch and know that I am thinking of you. We will get through this.55
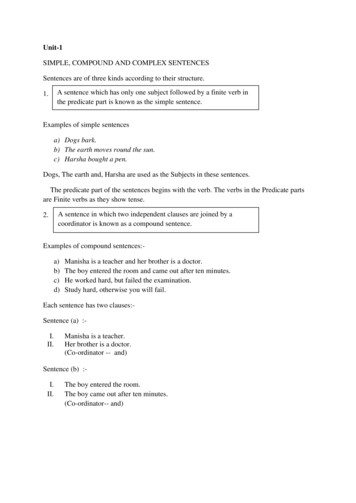
Applying Theory to PracticeMPH Students Share Their Applied Practice Experience Stories, April 2020The Applied Practice Experience is an essential component of thebe presented for the Bureau. I helped lead an outbreak investigationMPH degree, providing students with the opportunity to apply publicof a Cyclosporiasis infection associated with a restaurant inhealth theory to real-world projects. The APE provides the mentored,Manhattan, and my analyses were sent to FDA officials, ultimatelyhands-on training necessary to be successful in the workforce.leading to an ingredient traceback of a basil farm in Mexico.Team SalmonellaHow did the project or team work-style change with theRebecca Burns, MPH, Epidemiology TrackCOVID pandemic?How did you find your Applied Practice Experience (APE) andBeing in the Bureau of Communicable Disease during the start of awhat did you do?global pandemic was an extremely rare experience. When the firstI found an opportunity on the New York City Department of Healthtracing which involved calling people who may have had contact withand Mental Hygiene (NYCDOHMH) website to be a Disease Controlthe aforementioned case to ask them questions regarding exposureIntern in the Bureau of Communicable Disease. I was actually theand if they currently had any symptoms. As COVID-19 progressed,first ISMMS student to be a part of Team Salmonella, a uniquethe team started working remotely and developed electronicdisease control team.questionnaires that allowed us to continue Salmonella patientI conducted surveillance for food borne diseases such asSalmonella, Shigella, Campylobacter, and Shiga-toxin producinge. coli infections. This involved collecting patient data from healthcare providers and laboratory personnel, and interviewing patientsabout their illness and exposures. Team Salmonella also conductedcluster investigations, where we would track cluster-associatedcases and compare their exposure histories for commonalities. Ifcases were identified in New York City, I was tasked with contactinterviews from home. My experience within the NYCDOHMH atthis time also gave me the opportunity to interview for and accept aposition as a City Research Scientist, now working on the ongoingemergency response for the COVID-19 outbreak in New York City.Never Underestimate Your IdeasIsaiah Brown, MPH, Health Care Management Trackthe investigations were successful, we would work with CDC, stateTell us about your search foror city officials to create supplemental questionnaires and conductan APE.interviews regarding specific common exposures. Team SalmonellaFinding an APE didn’t comealso took on outbreak investigations when illnesses were linked witha restaurant or food supplier anywhere in the five boroughs of NewYork City. In these investigations, I was responsible for data entry,management, and analysis, and ultimately prepared final reports toeasy for me and took a lot ofpersistence. I went to ChristineCortalano, Manager for PublicHealth Practice, to help melearn how to search for an APEproject and she would evenemail me positions tailored tomy interests. I ultimately foundmy APE in the Friday Findsemail, applied, and was finallyaccepted into a position.What was your APE project?I assisted the Center for Health Equity and Community Wellness(CHECW) at NYCDOHMH with the construction of a biweekly eventcalendar and the production of CHECW video and photographyHistogram of reported cases by day for the Cyclosporiasis outbreak,provided by the Centers for Disease Control and Prevention (CDC).projects, cataloging consent, and tracking health topics on socialmedia. My APE work products included four months of socialmedia tracking data and my analysis and recommendations for thedivision’s outreach and future directions.6
What was a lesson you learned that you’ll use in your career?While working with Mount Sinai’s Health Education Department,Never underestimate your ideas! During my first division meeting,I helped create informational materials to support school-basedI was surprised by how my colleagues considered my suggestionsfor a project. Also, always make connections, no matter howsmall they may seem. You never know where those connections canhealth education programming for middle schoolers in the EastHarlem area. My primary project was creating a series of parentnewsletters to complement the department’s health educationlead you.curriculum. The newsletters contained actionable information toHealth Education with Actionable Informationrespectfully talking with their child about health, particularly sexualempower and support parents in productively, meaningfully, andand mental health.Allison Reichel, MPH Candidate, General Public Health fthefindingan APE that I could completealongside my professionalcommitments was initiallyOf all the skills I practiced during my APE, creating materials thatsupport positive health beliefs and behaviors and contain onlyrelevant, actionable information is one of the most valuable. Thehealth messaging being shared in response to the COVID-19pandemic has reinforced just how important this is, and I anticipateusing this skill often as I continue my work in public health.daunting. Christine Cortalanohelpedmeidentifysome great (and flexible!)opportunities and ultimatelyconnected me with t alth to learn more about howMaster of Public Health students complete theApplied Practice Experiencecompleted my APE.Discussing Job Seeking and Internship Hunting in Uncertain TimesOn April 9, 2020 Kelly Gentry, MA, LPC,My main takeaway from the webinar withProgram Manager, Public Health CareerKelly and Christine is to think ahead toServices and Alumni Relations, and Christinepost-pandemic needs. Focusing on publicCortalano, Program Manager, Public Healthhealth areas and populations that arePractice, hosted a webinar regarding thebeing impacted the most will be beneficialhow, when, and why (or why not) to searchwhen applying to future job and internshipfor new opportunities during a pandemic.opportunities.In our discussion, I learned that the public– Stacey Pinto, MPHhealth job and training opportunities are vastduring the current pandemic and potentiallywill continue to be after the pandemic.For some, this may actually a great timeto seek new opportunities. The webinarconversation also led me to think about ifstability in my current job is important to meright now, and consider if jumping to a newCurrent students and alumnican visit alth/career-servicesto engage in career servicesactivities.position is a good fit right now.- Katie Maguire, MPH Candidate7
Reflections on the First VirtualPublic Health Career FairANNOUNCEMENTSCongratulations to all June 2020 MPHgraduates! A number of graduates wereselected for awards related to the rigor oftheir research and writing, the excellencethey demonstrated in their Applied PracticeExperience, and their outstanding leadershipin the School community and larger New YorkCity community.Outstanding Public Health CulminatingExperience AwardVibhor MahajanAnne Impellizeri HahnSofia Viviana BengoaExcellence In Public Health Practice AwardStacey Heather PintoExcellence In Public Health LeadershipAnd Service AwardAcacia Lynn SmashGavriella L.Y. HechtInterested in having your writing or photospublished in The Scoop? Be a part of ournext issue! Contact one of our editors toget involved.The career fair gave me the time to touch base with dozens of potential employers andmake new connections.– Majdi Alghader, MPH CandidateIt was a great chance to keep my interview skills sharp in this period of increased virtualconnection. It was also helpful to learn how each of the org
ADUATE POAM IN PULIC HEALTH SPINSUMME Issue I hope this issue of the Scoop finds you healthy and safe. These are historic times for Public Health. New York City and Mount Sinai has been right in the epicenter. I have never been more proud of our students, faculty and staff than in their response to the COVID-19 pandemic. Whether through