Transcription
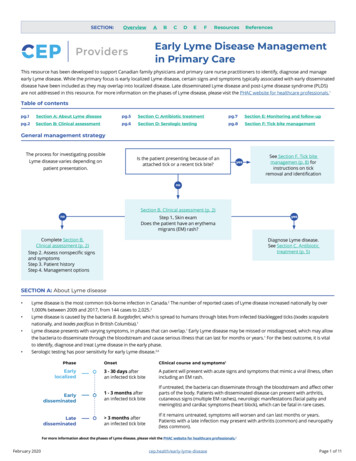
SECTION:OverviewABCDEFResourcesReferencesEarly Lyme Disease Managementin Primary CareThis resource has been developed to support Canadian family physicians and primary care nurse practitioners to identify, diagnose and manageearly Lyme disease. While the primary focus is early localized Lyme disease, certain signs and symptoms typically associated with early disseminateddisease have been included as they may overlap into localized disease. Late disseminated Lyme disease and post-Lyme disease syndrome (PLDS)are not addressed in this resource. For more information on the phases of Lyme disease, please visit the PHAC website for healthcare professionals.1Table of contentspg.1Section A: About Lyme diseasepg.5Section C: Antibiotic treatmentpg.7Section E: Monitoring and follow-uppg.2Section B: Clinical assessmentpg.6Section D: Serologic testingpg.8Section F: Tick bite managementGeneral management strategyThe process for investigating possibleLyme disease varies depending onpatient presentation.Is the patient presenting because of anattached tick or a recent tick bite?See Section F. Tick bitemanagemen (p. 8) forinstructions on tickremoval and identificationSection B. Clinical assessment (p. 2)Step 1. Skin examDoes the patient have an erythemamigrans (EM) rash?Complete Section B.Clinical assessment (p. 2)Step 2. Assess nonspecific signsand symptomsStep 3. Patient historyStep 4. Management optionsDiagnose Lyme disease.See Section C. Antibiotictreatment (p. 5)SECTION A: About Lyme disease Lyme disease is the most common tick-borne infection in Canada.2 The number of reported cases of Lyme disease increased nationally by over1,000% between 2009 and 2017, from 144 cases to 2,025.2Lyme disease is caused by the bacteria B. burgdorferi, which is spread to humans through bites from infected blacklegged ticks (Ixodes scapularisnationally, and Ixodes pacificus in British Columbia).1Lyme disease presents with varying symptoms, in phases that can overlap.1 Early Lyme disease may be missed or misdiagnosed, which may allowthe bacteria to disseminate through the bloodstream and cause serious illness that can last for months or years.1 For the best outcome, it is vitalto identify, diagnose and treat Lyme disease in the early phase.Serologic testing has poor sensitivity for early Lyme disease.3,4PhaseOnsetClinical course and symptoms1Earlylocalized3 - 30 days afteran infected tick biteA patient will present with acute signs and symptoms that mimic a viral illness, oftenincluding an EM rash.Earlydisseminated1 - 3 months afteran infected tick biteIf untreated, the bacteria can disseminate through the bloodstream and affect otherparts of the body. Patients with disseminated disease can present with arthritis,cutaneous signs (multiple EM rashes), neurologic manifestations (facial palsy andmeningitis) and cardiac symptoms (heart block), which can be fatal in rare cases.Latedisseminated 3 months afteran infected tick biteIf it remains untreated, symptoms will worsen and can last months or years.Patients with a late infection may present with arthritis (common) and neuropathy(less common).For more information about the phases of Lyme disease, please visit the PHAC website for healthcare professionals.1February 2020cep.health/early-lyme-diseasePage 1 of 11
Document 2Medical DocumentCardiogram 2X-raySECTION:BandageOverviewABCD ETubeSECTION B: cine 5Asset LibraryStep Pill1 : CapsulePerform a full-body skin exam to determineMedicineif the patienthas erythema migrans (EM) rash.6IconsEM is classically defined as a mainly flat, localized, expanding,Tooth Damageduniformly red rash (with or without central clearing) appearing at the siteof a tick bite.1,3,5,6 In the majority of cases, EM rash will not presentHospitalLabelIcons1,6with a bullseye appearance. While the majority of infected patients will develop an EM rash, aCardiogram3Tooth of patientssignificant number(at least 20%) will not.6 The darker the patient’s skin, the more difficult it may be toMedicineFirstaid 1,7kit2bagrecognize EMrash. See the PHAC website for healthcare professionals1 website forFirstkit bag2Cardiogrammore photosof aidvariedpresentationsof EM rash.Firstaid kit bag 3DocumentReportIf the patient has a localized rash that has appearedTooth Decay within the last 48LabelIconshours but is still relatively Labelsmall( 5cm in diameter), consider tracing the outline of therash with a waterproof marker. Instruct theInformationpatientto return to the clinic if the rash expands past theoutline.Continued expansion is suggestive ofEM.Onlinebanking2CalendarCheck-squareX-rayBlood 2(B)Document3BookCallBoneCenter3Features generally not consistent with EM3,6,8Features consistent with 2BoneBandagePhotos of erythema migrans rash.1 Bone2Medicine Medicine4Pill CapsuleMedicalAppears 3-30 days after a tick Bloodbite 2 DocumentThese symptoms may indicate an irritant reactionto a tick bite.2Expands within 48 hours ofHospital2X-ray Appears within hours after a biteappearance, usually to 5 cm in Is itchy, painful, hot, vesicular, raised,diameterTube Implantgeneralized (i.e. not localized)May last for weeks if untreatedTooth Recedes within 48 hours of its appearanceOften found near skin folds8,9(underarm, groin, back of knee)Bandage25MedicineDevelopment of additional EMrashes (indicates disseminatedTooth2 6Medicinestage)MedicalTooth DamagedToothReport3HumanHospitalmindBabyTooth DecayExam reveals EM rash.Blood( ) 3CardiogramDiagnose Lyme disease and treat immediately usingBlood(A) 2MedicineSection C, Antibiotic treatment (p. 5). Do not completeSteps 2 and 3.Blood(AB)First aidkit bag 2Exam reveals no rash, or a rashinconsistent with EM.BandageX-ray 2 3orMedicine7Online banking2Continue through Steps 2 and 3 to assessnonspecific symptoms and exposure risk.WarningDocument 3Step 2 : Identify nonspecific signs and symptoms consistent with early localized Lyme disease.Blood(O)First aidkit bag 3CautionCall CenterMobile BankingHospital 2Infected patients will develop a collection of nonspecific signs and symptoms within 3-30 days, ranging from mild to severe.1,3,6 Nonspecific signsand symptoms may becaused3 by many other illnesses, such as seasonal influenza.MedicineBlood 2 Before moving on to Step 3, rule out other potential causes ofillness as per usual clinical practice. Unlike most self-limiting viral illnesses, early Lyme disease symptoms usually last for over 72 hours.8Signs and symptoms consistent with earlyBone disease1,3,6,8localized Lyme SubjectiveBone or2 objective feverGeneralized arthralgias and myalgiasFatigueMedicine 4HeadacheSwollen lymph nodesTooth ImplantBandage 2Tooth 2MedicalTooth 3Human mindBabySymptoms generally not associatedwith early localized Lyme disease8 NauseaSore throatCoughRunny noseGI symptomsContinue to Step 3. Use the patient’s symptoms, in combination with the patient’s history taken in Step 3, to discern the level ofBlood ( )Bandage 3Blood (A)Medicine 7suspicion of Lyme disease.February 2020Blood (AB)cep.health/early-lyme-diseaseWarningPage 2 of 11
SECTION:OverviewABCDEFResourcesReferencesStep 3 : Take a detailed patient history to determine if the patient could have been exposed to an infected tick.To contract Lyme disease, a patient must have been fed on by an infectedblacklegged tick. The patient must come into physical contact with the tick forit to attach and feed. Ticks do not fly or jump.9Asset LibraryIconsPatients can come into contact with ticks: Outdoors in areas such as parks, meadows, wooded yards,campgrounds, golf courses and soccer fields. Indoors if a ticktravelled inside on pets, Iconsclothing or outdoor gearLabel(e.g. tents or boots).ToothThe recollection of a tick bite is not a requirement todiagnose Lyme disease. Many people will not recall orbe aware of tick bites because ticks are small and theirbites are painless.1,3,9 If your patient remembers a tickbite, incorporate information from Section F. Tick bitemanagement (p.8) into the assessment.LabelIconsBlood (B)InformationCalendarCheck-squareIn the last 30 days, has the patient or the patient’s pet been in woody or grassyareas such as parks, meadows, wooded yards, campgrounds, golf courses, soccer fields, etc.?First aid kit bagUnlikely to haveCardiogrambeen exposed to blacklegged ticks.Ticks must come into physical contact in order toDocumentattach and feed.Consider an alternative diagnosis.BookDuring outdoor activity, did the patient or thepatient’s pet come into contact with grass, underbrush,trees or leaf litter?Bone 3Document 2Medical DocumentUse this table to assess whether the patient visited an area with elevated risk.Click on a province abbreviation to see detailed risk information for thatCardiogram 2X-rayprovince. While cases of Lyme disease have been reported in every province, theoverall risk of Lyme disease varies considerably from province to province and withinBandageTube2individual provinces.It is possible for patients to contract Lyme disease in lowand2moderate risk areas as ticks are spreading due to climate change.Medicine 1 case / 100,000Lowest riskProvince /territory1-19 cases / 100,000PillModerateCapsuleriskWhere did this outdooractivity take place?Medicine 520-49 cases / 100,000Higher risk(highest in Canada)Tooth DamagedOverall provincial risk(based on incidence rate)2HospitalLowest riskBC10AB11Cardiogram 3Lowest risk 50 cases / 100,000Very high riskMedicine 6ReportRisk (basedon incidencerate)Moderate or higher riskareas within province?yesnoTooth DecayUnitedStates20X-ray 2Medicine 2noOnline banking 2MBFirst aid kit bag 2yesDocument 3ON14First aidModeratekit bag 3 riskSK1213Lowest riskModerate BankingyesNL17NS18PEI19NT/YT/NU2Lowest risknoHigher riskyes - including very high risk areasModerate riskyesBoneBone 2Europe21Tooth ImplantBandage 2Medicine 4Tooth 2MedicalTooth 3Human mindBabyBlood ( )Bandage 3orThere have been no reported cases of Lyme disease in the territoriessince the Public Health Agency of Canada began tracking cases in 2009.Steps 2 and 3 reveal symptoms suggestive of early Lyme diseaseand high probability of exposure to infected ticks.Continue to Step 4 to consider options based on clinical suspicion.Blood (A)February 2020Blood 2Hospital 2Blood (AB)ModerateriskHigherriskrisk areasyes - including very high CallCenter15QCLabelPlease notethat this is notan exhaustivelist. For moreinformationon risk areasin Europe, seethe Resourcespage.JurisdictionIllinois, Indiana, Iowa, Maryland,Michigan, Massachusetts, NewYork, North Dakota, Ohio,Virginia, Washington D.C.Connecticut, Delaware,Minnesota, New Jersey,West Virginia, WisconsinVeryhigh riskMaine, New Hampshire,Pennsylvania, Rhode Island,VermontModerateriskBelarus, Belgium, Bulgaria,Croatia, Finland, Hungary,Norway, Poland, the RussianFederation, Serbia, SlovakiaHigherriskthe Czech Republic, Estonia,LithuaniaVeryhigh riskSloveniaSteps 2 and 3 reveal symptoms inconsistent with early Lymedisease and/or low probability of exposure to infected ticks.Unlikely to be Lyme disease. Consider an alternative diagnosis.Medicine 7cep.health/early-lyme-diseaseWarningPage 3 of 11
ToothBlood (B)InformationFirst aid kit BCDBookEFResourcesReferencesDocument3Step4 : Choose a management option based onBoneclinicalsuspicion and patient preference.Document 2Medical DocumentExtra care should be taken to promptly diagnose andtreat early Lyme disease in pregnant women.8,9,23However, evidence for adverse effects on the fetus is weakTubeand has been limited to retrospective case reports.9,23,24Reassure pregnant patients that:Medicine No5negative effects on the fetus have been found whenmothers receive appropriate antibiotic treatment.9,24Medicine6 Currentevidence does not support the transmission ofB. burgdorferi through breastfeeding.9,24Clinical diagnosisof earlyCardiogram2 Lyme disease in patientswithout EM rash can be difficult.8X-rayIf symptomsBandageand exposure history raise clinicalsuspicion of early Lyme disease, there are twooptions for management.While neither option hasMedicinebeen validated, both are reasonable.8 Use the tablebelow to make an informed decision in collaborationPill Capsulewith your patient.22Tooth DamagedReportHospitalCardiogram 3Tooth DecayX-ray 2Management options for patients without EM rash82Option A: TreatMedicineempirically.Based on a high degree ofclinical suspicion, treat empirically during acute infection.ConsiderDocument3 ordering serologic testing, and treat if serology ispositive.Enables early treatment, potentially relieving a patient’sFirst aid kit bag 3suffering sooner and halting disease progression beforeit reaches the disseminated stageCons persistence or worsening, or development of new symptoms.First aid kit bag 2Pros Onlinebanking2OptionB: Waitand watch. Monitor patient for symptomCall CenterPros Medicine 3May expose a patient to unnecessary antibiotics if initialMobile Bankingdiagnosis of Lyme proves incorrect. The harms of this caninclude:Bone An increased risk of antibiotic-associated adverseevents/complicationsBone 2 Risk of developing resistance to antibiotics Delayed identification of true cause of symptomsCons2Hospital MedicalTooth 3Human mindBabyBlood If( )selecting option A,see Section C. Antibiotic treatment (p. 5).Bandage 3 Medicine 7Blood (A)February 2020Increased risk of Lyme-associated morbidity (neurologic,Bandage cardiac2and rheumatologic)Tooth 2Blood (O)May prolong patient’s suffering due to potentially signifi-cant delays in reporting test resultsTooth ImplantMedicine 4Blood (AB)Resistance is a global health problem and preserving theBlood 2 efficacy of our current antibiotics is essentialorWarningCaution cep.health/early-lyme-diseaseIf selecting option B:Treat symptoms as per usual clinical practiceConsider ordering serologic testing. See Section D.Serologic testing (p. 6)Instruct the patient to return to the clinic if: Symptoms persist or worsen after 1 week Suspected EM rash continues to expandProvide a copy of the patient tool to help informthe patient about symptoms and prevention ofLyme diseasePage 4 of 11
First aid kit okDECheck-squareFResourcesBone 3SECTION C: Antibiotic treatmentDocument 2Medical DocumentCardiogramto2Table 1. Doxycycline is the recommended first-lineX-rayPrescribe antibiotics according1,3,5,25antibiotic for Lyme disease.It is the most effective at preventing severe complications if3BandageTubestarted in the early phase.Medicine duration for early Lyme disease is 21 days.3 WhileMedicineThe recommended treatmentsome5providers may be tempted to prescribe shorter courses, due to the acute nature of theinfection as well as recommendationsfrom other sources,1,5,25 this practice shouldbe 6Pill CapsuleMedicineavoided. There is some evidence suggesting that shorter courses may result in lower curerates while not significantlyreducing the number of adverse events.3Tooth DamagedReportHospitalAdultsTable 1. Antibiotic treatment of early localized Lyme disease1,3,25-28X-ray 2LineDrugDosage1stDoxycycline100 mg orallyMedicine 2First aid kit bag 22ndCefuroxime axetilFirst aid kit bag 3Children( 18 years)Medicine31st500 mg orallyFrequencyMaximumDurationTwice/dayN/A21 daysN/A21 daysN/A21 daysOnline banking 2Document 3Twice/dayCall CenterAmoxicillin500 mg orallyDoxycycline4 mg/kg orallyBlood2 2 divided dosesDaily,100 mg per dose21 days50 mg/kg orallyDaily,Hospital2 3 divided doses500 mg per dose21 days30 mg/kg orally2 divided dosesToothDaily,Implant500 mg per dose21 days2nd Banking AmoxicillinMobileBoneBoth laboratory and clinically-diagnosedcases of Lyme disease are nationallynotifiable.26 See PHAC’s National CaseDefinition for Lyme disease to determine if apatient’s case is reportable.Tooth DecayCardiogram 3AgeReferencesCefuroxime axetilThree times/dayBandage 2Special populations:Bone 2 Pregnant women: Doxycycline is contraindicated during pregnancy, and should not be used for the treatment of early Lyme disease inMedicine4 women should be treated using appropriateTooth2pregnant women.Pregnantantibioticsfor their stage of pregnancy.1,3,25 Children: A growing consensus accepts the safety of doxycycline use with children 8 years old, for 21 days or less.27 Historicallydoxycycline has Medicalbeen contraindicated in children 8 years old due to itsToothpotentialto cause teeth staining.3Human mindBabyFor all patients, refer to post-treatment follow-up recommendations in Section E (p. 7).February 2020Blood ( )Bandage 3Blood (A)Medicine 7Blood (AB)WarningBlood (O)Cautioncep.health/early-lyme-diseasePage 5 of 11
SECTION:OverviewABCDEFResourcesReferencesSECTION D: Serologic testingProviders should only consider serologic testing to assist with diagnosis if: 1) they understand the appropriate use of the testing algorithm; and,2) they are uncertain about clinically diagnosing a patient who is only exhibiting nonspecific symptoms.1,3 Antibiotic treatment for early Lyme diseasemay inhibit seroconversion and impact the validity of serologic tests.3,8Cautions1,3,8Choosing to Test: DO NOT test asymptomatic patientsDO NOT test patients who have EMrash. They can be diagnosed andtreated without serologic testing.Testing and Diagnosis: Interpreting Test Results:DO NOT rely on test results alone to makea diagnosisDO NOT rule out early Lyme disease inpatients with negative resultsDO NOT use either tier as a stand-alone test DO NOT use as a test of cureDO NOT use 2-tiered test tomeasure treatment responseStandard two-tiered testing (STTT) algorithm1,3,29,30This information is for general guidance. Laboratory testing procedures may vary by province/territory.In Canada, laboratory testing for Lyme disease traditionally involves a sequential, two-tiered testing algorithm. The first tier is an enzymeimmunoassay, followed by the second tier (western blot) in the event that the first tier is positive or equivocal.The first tier is ordered from your provincial lab. For all provinces, except Ontario and British Columbia, positive/equivocal samples are automaticallysent to the National Microbiology Laboratory (NML) for confirmatory testing using the second tier. For Ontario and British Columbia, second-tiertesting is only sent to the NML if European exposure is suspected. Otherwise, second-tier tests are conducted in-province.29,30Required information for lab requisitions may vary by province/region. Providers should indicate if the potential exposure to a tick occurred inEurope, as different tests are required to detect European species of Borrelia. The duration of symptoms should also be indicated, as testingfor IgM antibodies should be avoided in patients who have been ill for 1 month (in these patients, IgG antibodies must be positive in order todiagnose Lyme disease).1st Tier: Enzyme immunoassay (EIA/ELISA)Turnaround time: 1 week2nd Tier: Western blotTurnaround time: 3 weeks from receipt at NMLPurpose: Screens for Lyme disease antibodies (IgG andIgM). Has poor sensitivity during early Lyme disease, whichmay lead to a high number of false negatives.3,4If Positive or Equivocal: Purpose: Confirmatory test used after positive/equivocal1st tier test. European genospecies require differentwestern blots. If symptoms have lasted 1 month, only IgGantibodies should be tested.Serum referred for 2nd tier.If Positive or Equivocal: If Negative: Consider alternative diagnoses, but do not rule outLyme disease.3If the test has been done within the first 30 days ofonset, repeat the 1st tier 4-6 weeks after the initial test.3If negative again, do not order a third 1st tier test.3,8 Diagnose Lyme disease and prescribe antibiotictreatment.1,3 See Section C. Antibiotic treatment (p. 5)If symptoms have lasted 1 month, IgG must bepositive in order to diagnose. Do not diagnose basedon positive IgM after 1 month.1If Negative: Consider an alternative diagnosis, includingnon-infectious diseases3,5,8Consider consulting with or referring to an appropriatespecialist3,8Modified two-tiered testing (MTTT) algorithm31In 2019, the U.S. FDA approved a modified two-tiered test (MTTT) as an alternative to the standard two-tiered test (STTT) based on evidence thatshowed MTTT performance to be equivalent or better than the STTT.31 In the MTTT, the second tier is an additional EIA/ELISA (instead of a westernblot) which can be performed concurrently with the first-tier EIA/ELISA. Access: All Canadian labs will use the STTT but may not use the new MTTT (at time of this resource’s publication).1,8 Turnaround time: EIA test results are returned more quickly than western blots. Faster results ( 1 week) may support more timely treatmentdecisions.8,31February 2020cep.health/early-lyme-diseasePage 6 of 11
HospitalTooth DecayCardiogram 3X-ray 2Medicine 2SECTION:OverviewFirst aid kitbagfollow-up2SECTION E: MonitoringandABCDEFResourcesOnline banking 2ReferencesDocument 3The majority of patientsreceiveduration are cured once therapy is finished, and show a resolutionFirstwhoaid kitbag 3 an appropriate antibiotic for an appropriateCall Centerof all signs and symptoms.1,3,5 However, some patients may have symptoms that persist after therapy.1,3,5 Immediately following the completion8of antibiotic treatment,assess3the patient for evidence of disease persistenceBloodor progression.Include the patient in your decision-making as youMedicine2consider the next steps.22Mobile BankingHospital 2It is possible for patients to become infected with more than one tick-borne pathogen.5 In Canada, the most common tick-borneBoneTooth Implantinfections other than Lyme disease are anaplasmosis (caused by Anaplasma phagocytophilum), babesiosis (caused by species of Babesia)and Powassan virus disease.32 Potential co-infection should be suspected in patients who present with symptoms that are moreBone 2Bandage 2severe than commonly observed in cases of early Lyme disease alone, especially those with:5 High-grade fever for 48 hours, despite receiving appropriate antibiotic treatment for Lyme diseaseMedicine4 thrombocytopenia or anemiaTooth 2 Unexplainedleukopenia, No improvement (or worsening) of nonspecific symptoms despite resolution of EM rashMedicalTooth 3Human mindBabyBlood ( )Bandage 3Blood (A)Medicine 7Satisfied with symptom resolution Have the patient monitor anyBlood(AB)remainingsymptomsfor continuingresolution.BloodEncouragethe(O)patient to returnto the clinic if remaining symptomspersist. Schedule subsequentassessments as requested bythe patient.22Share the patient tool and highlightmethods of prevention to avoidfuture infection.Not satisfied with symptom resolutionorAdults: Treat symptoms as per regular clinical practice, and consider thefollowing Warningas appropriate:3,8 Second round of treatment with an alternative antibiotic.3,5 See SectionCautionTreatment (p. 5).C. Antibiotic Alternative diagnosis. Referral to infectious disease specialist. Possibility of co-infection. See below for further information.Children: If symptoms persist after a complete course of antibiotics, treatsymptoms as per regular clinical practice, and refer the patient to aninfectious disease specialist.3,8If you are suspicious of co-infection: Consider a referral to an infectious disease specialist.8 Doxycycline is effective at treating anaplasmosis. The treatment regime for Lyme disease should also resolve anaplasmosis.5,33 Doxycycline alone is not effective for treating babesiosis or Powassan virus disease.5Visit the U.S. Centers for Disease Control and Prevention websites for more information on babesiosis34 and anaplasmosis33, or thePublic Health Agency of Canada website for more information on Powassan virus disease.35February 2020cep.health/early-lyme-diseasePage 7 of 11
SECTION:OverviewABCDEFResourcesReferencesSECTION F: Tick bite managementTo transmit Lyme disease, a blacklegged tick infected with B. burgdorferi must attach toa person and feed for an extended period of time (most evidence suggests aminimum of 24 hours).1,5,9 The likelihood of disease transmission increases withattachment time.9 If a tick has been feeding, it will become engorged, but this level ofengorgement is often difficult to determine in practice.The images to the right may help to identify blacklegged ticks and determine if arecently-discovered tick was attached long enough to transmit disease. It may be verydifficult for patients and healthcare professionals to identify tick species and estimateattachment time, especially if a tick has been damaged during removal.8Unfed blacklegged ticks(deer ticks)36Unfed American dog ticks(wood ticks)36Levels of engorgement in adultblacklegged ticks as a result offeeding on blood36Is the tick still attached?If the patient recalls removing a tick fromtheir skin within the last 30 days: Use Section B. Clinical assessment (p. 2)to check for signs and symptoms of earlyLyme disease. Note that signs andsymptoms of early Lyme disease maytake up to 30 days to appear afterinfection. Provide a copy of the patient tool, whichwill provide more information on course,treatment and prevention of Lymedisease. Advise the patient to monitor forsymptom development over the nextfew weeks. If the tick was removed within the last72 hours, and all other criteria are met,consider offering post-exposureprophylaxis.5 See below for moreinformation.Remove tick:37,38 Do not use sharp forceps. Use blunt, mediumtipped, angled forceps to grasp the head of thetick as close to the skin as possible. Do not use a twisting or jerking motion toremove the tick. Use perpendicular traction,taking care not to twist or crush the tick. If themouthparts break off and remain in the skin, remove them with forceps. Clean the area with an antiseptic solution. Record the date in the patient’s record. Instruct the patient to monitor for signs and symptoms for the next 30days. Provide a copy of the patient tool, which will provide more information oncourse, treatment and prevention of Lyme disease. Dispose of the tick. Do not submit ticks for testing to seek confirmation ofLyme disease. See the PHAC website38 for information on submitting ticksfor surveillance purposes only. If the patient meets all of the criteria, consider post-exposure prophylaxis(below).5Post-exposure prophylaxis5Post-exposure prophylaxis is not generally recommended. Providers may consider prophylactic treatment in asymptomatic patients if all thefollowing criteria are met: Attached tick can be positively identified as a blacklegged tick (see images above) Tick was engorged and estimated to have been attached for 24 hours Prophylaxis can be started within 72 hours of tick removal Tick was acquired in an area where the infectivity rate of the tick population with B. burgdorferi is 20% . [Note: Infectivity rate is notuniformly collected in Canada. However, recent reports have shown that areas of Ontario, Manitoba and Nova Scotia have infection rates 20%.39,40,41 Many provinces and U.S. states instead estimate incidence rate by confirmed and probable cases.] Doxycycline is not contraindicatedIf all of the above criteria are met: A single prophylactic dose of doxycycline may be given to adults (200mg) and children (for children under 45kg, 4 mg/kg to a maximum dose of200 mg). Recent research suggests a single dose of doxycycline is safe for pregnant women.42,43 If doxycycline is contraindicated, do not offer an alternative antibiotic. Antibiotics other than doxycycline have not been proven effective.1,5As post-exposure prophylaxis is not 100% effective, patients should be monitored for the development of signs and symptoms for 30 days.5,44February 2020cep.health/early-lyme-diseasePage 8 of 11
SECTION:OverviewABCDEFResourcesReferencesRisk area resources: Canada, U.S. and EuropeCanadaNational BC AB Government of Canada surveillance website: Most recent data/report (2017): se-canada-2009-2015.htmlSurveillance website: emiologyInteractive map: rts/reportable-diseases-data-dashboardSurveillance website: nce.aspxMost recent data/report: (2018): mary-report.pdfInteractive map: /vizhome/Ticks AB/AlbertaTicks Surveillance website: anMost recent data/report: (2019) ts/100547/formats/111004/downloadMB Surveillance website: borne/surveillance.htmlMost recent data/report: (2017) borne/docs/tbd report2017.pdfON Surveillance website: tic-diseases/lyme-diseaseMost recent data/report: (2018) nually#/34SK QC Surveillance website: s/maladie-lyme/surveillance-de-la-maladie/Most recent data/report: (French – 2017): https://www.inspq.qc.ca/en/node/14523(English – 2016): https://www.inspq.qc.ca/en/publications/2417NB Surveillance: https://www2.gnb.ca/content/gnb/en/departments/o
Mobile Banking Hospital 2 Document 2 Medical Document Medicine 2 Online banking 2 Medical Tooth 3 Cardiogram Book Hospital Tooth Decay Bone 2 Bandage 2 Bandage Tube First aid kit bag 3 Call Center Blood ( ) Bandage 3 Blood (AB) Warning First aid kit bag Calendar Tooth Damaged Report Bone Tooth Implant Cardiogram 2 X-ray First aid kit bag 2 .