Transcription
NC MedicaidManaged Care
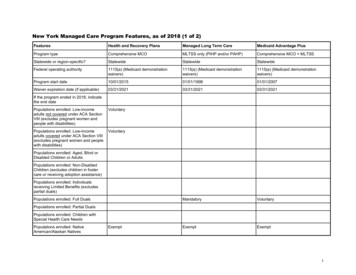
Webinar Summary Webinar Summaryo The NC Medicaid Managed Care transition and its impact on beneficiarieso The timeline for open enrollment and what to expect in terms of communication tobeneficiarieso And how you can partner with the Enrollment Broker to educate beneficiaries Webinar Speakerso Dave Richard, Deputy Secretary, Medicaido Sandy Terrell, Director Benefits and Services, Medicaido Eric Rubin, Division President for Health Services at MAXIMUSMedicaid Transformation page: rmationCounty playbook page: id-managed-careJune 25, 2019 / NC Medicaid Managed Care2
NC Medicaid Managed CareTransition
Vision for NC Medicaid Managed CareImproving the health and well-being of North Caroliniansthrough an innovative, whole-person centered and well-““coordinated system of care that addresses both medical andnon-medical drivers of health.June 25, 2019 / NC Medicaid Managed Care4
Common Terminology NC MEDICAID DIRECT: the current fee-for-service model where the Department of Health and HumanServices reimburses physicians and healthcare providers based on the number of services theyprovide, or the number of procedures they order. NC MEDICAID MANAGED CARE: State will contract with insurance companies, called Prepaid HealthPlans or PHPs (Health Plans). These insurance companies will be paid a pre-determined set rate perperson to provide all services, known as a capitated rate ELIGIBILITY: refers to whether a person qualifies for Medicaid or NC Health Choice (NCHC). Eligibleindividuals may need to enroll in a Health Plan. ENROLLMENT: the process of joining a Health Plan that is responsible for that person’s Medicaidhealth coverage. BENEFICIARY: a person who is eligible for Medicaid or NCHC. MEMBER: once a beneficiary enrolls in a Health Plan. STANDARD PLAN: integrated physical & behavioral health services under NC Medicaid ManagedCare. TAILORED PLANS: specialized plans for members with significant behavioral health needs andintellectual/developmental disabilities. Tailored plans will be coming in 2021.June 25, 2019 / NC Medicaid Managed Care5
What is Medicaid Transformation?Most people will get the same Medicaid services in a new way –through Health PlansWhat is NC Medicaid Managed Care?Under NC Medicaid Managed Care, the insurance companies assume all of the risk forthe individuals they cover, rather than the state. This also means that beneficiaries canchoose a Health Plan.Who is Impacted?Approximately 1.6 million of the current 2.1 million NC Medicaid beneficiaries willtransition to NC Medicaid Managed Care. These beneficiaries are referred to as the“crossover population.”June 25, 2019 / NC Medicaid Managed Care6
Medicaid Transformation FocusThe Department’s focus for Medicaid Transformation is that on Day 1: A person with a scheduled appointment will be seen by their providerA person’s prescription will be filled by the pharmacistA provider enrolled in Medicaid prior to Nov. 1, 2019 will still be enrolledA provider is paid for care delivered to membersJune 25, 2019 / NC Medicaid Managed Care7
Who is Enrolled in NC Medicaid Managed Care?NC Medicaid will determine which population beneficiaries fall into and if it is mandatory, exemptor excluded. This determination if beneficiaries must enroll in NC Medicaid Managed Care, shouldstay in NC Medicaid Direct or can choose.NC Medicaid will also be responsible for auto-assignment.ealth plan.MANDATORYEXEMPTEXCLUDEDA majority of beneficiaries will beconsidered mandatoryand must enroll inNC Medicaid Managed Care.Those who have the option toremain in NC Medicaid Direct ortransition to NC Managed Care.Some will remain in NCMedicaid Direct because of thetype of medical services theyneed. This small number will beexcluded from obtaining aHealth Plan through NCMedicaid Managed Care.June 25, 2019 / NC Medicaid Managed Care8
The Impact of Managed Care on BeneficiariesWhat’s new?Can choose aHealth PlanMost will be enrolled inNC Medicaid Managed CareWhat’s staying the same?Eligibility rulesJune 25, 2019 / NC Medicaid Managed CareServices coveredCo-pays (if any)Report changes tolocal DSS9
Health Plan BenefitsNetwork ofprovidersSee the doctor asoften as needed24-hournurse lineJune 25, 2019 / NC Medicaid Managed CareNo monthlypremiumsHelp withreferrals10
The Impact of Managed Care onBeneficiaries with Behavioral Health NeedsIndividuals will receive fully integrated whole person care in both standard and tailored plans.Both plans will: Cover physical, behavioral health and pharmacy services Contract with behavioral health providers Have behavioral health crisis lines Standard plans Most Medicaid population including individuals with mild to moderate behavioral healthneeds Tailored plans Targeted to populations with significant behavioral heath conditions Additional services available and only plan to offer current 1915(b)(3), 1915(c) Innovationsand traumatic brain injury (TBI) waiver and state-funded services Health home care management model LME-MCOs will continue to exist until becoming tailored plans in 2021 June 25, 2019 / NC Medicaid Managed Care11
Roles and Responsibilities43152DSSNC MEDICAIDDetermineEligibilityDefine Population asMandatory, Exemptor ROKERMails Notice andEnrollment Packetto BeneficiariesChoice Counselingand EnrollmentHEALTH PLANSends MembersHealth PlanInformationAnswers plan andbenefits questionsOutreach12
Key Partners and Their Roles Beneficiaries are at the center of this process. Partners need to work together to supportbeneficiaries through this transformation and ongoing.NC Medicaid: provide Medicaid supervision, oversight of Health Plans and other partnersLocal DSS: determine Medicaid eligibility, update beneficiary information, Medicaid casemanagementNC FAST & NCTracks: these systems will continue to transmit beneficiary information; NCFAST will remain the system of record.Providers: will contract with the Health Plans; must continue to enroll as an NC Medicaid orNC Health Choice providerOmbudsman: (*this program is pending) group that provides information and education forbeneficiaries; assist with issue resolution and referralsEnrollment Broker: unbiased, third party entity to provide enrollment assistance and helpchoosing a Health Plan; outreach & education to beneficiaries.Community-based Agencies: disseminate information to help educate the public on changesto Medicaid; provide feedback to DHHS from clients they serveHealth Plans: provide health care and related services to their membersJune 25, 2019 / NC Medicaid Managed Care13
Health Plan ResponsibilitiesHealth Plans will: Ensure their Members receive the same services as they did under NCMedicaid Direct Provide Non-Emergent Medical Transportation (NEMT) Services forManaged Care Members Assist Members with primary care provider (PCP) information andcomplete PCP Auto-Assignment if no PCP is selected Supply NC Medicaid Managed Care Medicaid Card/ReplacementCards Conduct Care Needs Screening for Members Operate a Call Center/Member Service Lines Facilitate Appeals and Grievances Provide Health Plan Welcome Packets, including Welcome Letter,Medicaid Card and Member HandbookJune 25, 2019 / NC Medicaid Managed Care14
NC Medicaid Managed CareTimeline15
Phase 1 CountiesRegion 2Region ngePersonVanceWakeWarrenWilsonJune 25, 2019 / NC Medicaid Managed CareREGION 2REGION 4REGION 6REGION 1REGION 3REGION 516
Phase 1 Timing – Regions 2 and 4NOV. 1, 2019AUG. 13, 2019JUNE 28, 2019Health PlanCoverageStartsReminderPostcardMailings StartJULY 15 –SEPT. 13, 2019OpenEnrollmentJune 25, 2019 / NC Medicaid Managed CareSEPT. 16, 2019Auto-AssignmentFEB. 1, 202090Lock-in PeriodStartsNOV. 1, 2019– JAN. 31, 202090 DayChoice Period17
Phase 2 CountiesRegion 1Region 3Region 5Region dHarnettHokeLeeMontgomeryMooreNew nsPittTyrrellWashingtonWayneJune 25, 2019 / NC Medicaid Managed CareREGION 2REGION 4REGION 6REGION 1REGION 3REGION 518
Phase 2 Timing: Regions 1, 3, 5 and 6FEB. 1, 2020Health PlanCoverageStartsNOV. 13, 2019SEPT. 2, 2019ReminderPostcardMailings StartOCT. 14 –DEC. 13, 2019OpenEnrollmentJune 25, 2019 / NC Medicaid Managed CareDEC. 16, 2019Auto-AssignmentMAY 1, 202090Lock-in PeriodStartsFEB. 1, 2020– APRIL 30, 202090 DayChoice Period19
Working with theEnrollment Broker
About the Enrollment BrokerThe Enrollment Broker is responsible for choice counseling for Health Plan and PCPselection; as part of this, the Enrollment Broker is also responsible for mailing all noticesand handling enrollment.““An Enrollment Broker is an entity that performs choicecounseling or enrollment activities, or both. Eligibilityservices are completed by NC Medicaid, not by theEnrollment Broker. Enrollment Brokers and subcontractorsmust not have direct or indirect financial ties to any HealthPlan or healthcare provider that furnishes services in thesame state where the Enrollment Broker work is performed.Source: The Centers for Medicare & Medicaid Services (CMS) Code of Federal Regulations 42 CFR § 438.810 - Expenditures for enrollment broker servicesJune 25, 2019 / NC Medicaid Managed Care21
The Largest Medicaid AdministrativeServices Provider70%market share ofMedicaid managed careNC2019June 25, 2019 / NC Medicaid Managed Care22
Enrollment Broker Servicesin North CarolinaCommunications hubOutreach and educationWebsite and mobile appPartnering with DSSand local organizationsChoice counselingEnrollmentJune 25, 2019 / NC Medicaid Managed Care23
Choice CounselingDelivering information and assistance effectively to consumers Provide unbiased, culturally competent choice counseling services to beneficiaries Simplify the application and enrollment process so it’s easy for consumers tounderstand, and satisfy program requirements Achieve improved voluntary choice rates for better health outcomesTrained customerservice teamJune 25, 2019 / NC Medicaid Managed CareResponsive andempathetic6th grade levelof health literacy24
Enrollment AssistanceStreamlining the decision making and enrollment process Communicate with consumers on their preferred channels – whether by web,phone, email, text and mobile app Proactively engage beneficiaries at critical points to ensure they enroll as necessaryMultichannelincluding mobileJune 25, 2019 / NC Medicaid Managed CareSelf-service60% of consumersdon’t understandtheir benefits25
Options forBeneficiariesCHANNELS FOR ENROLLMENT1. Direct them to ncmedicaidplans.gov tolearn more2. Direct them to ncmedicaidplans.gov tochat with an Enrollment Specialist3. Direct them to download and use the NCMedicaid Managed Care mobile appEnrollmentServicesWebsiteWeb Chat4. Tell them to call 1-833-870-5500 to speakwith an Enrollment Specialist. The call isfree.5. Individuals with hearing impairments maycontact an Enrollment Specialist via theTTY line 1-833-870-5588.6. Beneficiaries can also enroll by mailing orfaxing their completed enrollment formMobile AppEnrollmentSpecialistMail/FaxTTY26
Website: ncmedicaidplans.govThe NC Medicaid Managed Care website provides anintegrated experience for beneficiaries to manage theirenrollment needs. This is a great resource to directbeneficiaries to for questions about enrollment. Thewebsite includes the following tools and information: Health plan comparison charts and lists of benefits Provider network search capability Program information, brochures and enrollment forms(as downloadable PDFs) Questions and answers List of events in their countyAvailable in English and Spanish, it can be accessed atncmedicaidplans.gov.Enrollment Specialists are available via a chat tool toanswer questions.June 25, 2019 / NC Medicaid Managed Care27
Web Chat Web chat service is available via asecure web portal Web chat adds an online alternativefor real-time assistance for users Members can begin a web chatconversation from any page on thewebsite via the “Chat with Us!”button Web chat is also compatible withiOS and Android operating systemsfor mobile users Enrollment Specialists will providechat assistance, answeringquestions and directing members toappropriate pages of the website tolearn moreJune 25, 2019 / NC Medicaid Managed Care28
NCMedicaidManagedCareMobileAppJune 25, 2019 / NC Medicaid Managed Care29
App Features The mobile app allows for seamlessconnection and interaction withbeneficiaries With the app, the Head of Householdcan: View all case contact information Alter some case contact information View all member enrollment information Alter all member enrollment information30
Enrollment Call CenterEnrollment Specialists are available at the call center forsupport. Beneficiaries can call toll free: 1-833-870-5500.EXTENDED HOURSDURING OPENENROLLMENT:7 a.m. – 8 p.m.7 days a weekWe are available to: Provide choice counseling Support search for preferred PCP Compare Health Plan services Enroll members in selected Health Plan Assist with some demographic changes Disenroll members as needed Process Enrollment Broker complaints and grievances Facilitate appeals processALL OTHER TIMES:Monday – Saturday,7 a.m. – 5 p.m. Receive warm transfers Provide support for the website and mobile app Provide assistance for deaf, blind and non-Englishspeaking beneficiaries31
Outreach and EducationEnsuring a seamless and streamlined beneficiary experience, the Enrollment Broker will: Partner with North Carolina’s county DSS offices and community organizations to providemanaged care training Provide member materials that are understandable and accessible Conduct outreach services that meet consumer’s cultural and behavioral expectationsIn-person services,group presentations,enrollment eventsand health fairsJune 25, 2019 / NC Medicaid Managed CareDistribution ofinformation andeducational materialsTraining32
Outreach Events: Home PageJune 25, 2019 / NC Medicaid Managed Care33
Partner Engagement & Member OutreachPartner Engagement EventsTypes of Events: Onboarding sessionsCross-functional trainingsMonthly webinarsReadinessTypes of Materials: Managed care toolkitPresentationsRecordingsSystems trainingJune 25, 2019 / NC Medicaid Managed CareMember Outreach EventsTypes of Events: Member education: Enrollment events Community events Meet & greet Informational boothTypes of Materials: Media campaigns Marketing materials Flyers, fact sheets, etc.34
Outreach MaterialsPOSTERFACT SHEETQ&APALM CARDFLYERDownload at: ed-careJune 25, 2019 / NC Medicaid Managed Care35
Introductory VideoThe NC Medicaid Managed CareIntroductory Video addresses: What is a primary care provider (PCP) What is a Health Plan The Health Plans available What beneficiaries need to do What happens after beneficiaries enroll The phases for enrollment and key dates How to get answers to additional questionsJune 25, 2019 / NC Medicaid Managed Care36
Enrollment Packet: Sample Transition NoticeDownload at: ed-careJune 25, 2019 / NC Medicaid Managed Care37
Sample Mandatory NoticeDownload at: ed-careJune 25, 2019 / NC Medicaid Managed Care38
Sample Excluded NoticeDownload at: ed-careJune 25, 2019 / NC Medicaid Managed Care39
Sample Exempt NoticeDownload at: ed-careJune 25, 2019 / NC Medicaid Managed Care40
Enrollment Packet: Informational FlyerDownload at: ed-careJune 25, 2019 / NC Medicaid Managed Care41
Enrollment Packet: Enrollment FormDownload at: ed-careJune 25, 2019 / NC Medicaid Managed Care42
Enrollment Packet: Comparison ChartDownload at: ed-careJune 25, 2019 / NC Medicaid Managed Care43
Enrollment Packet: Comparison ChartDownload at: ed-careJune 25, 2019 / NC Medicaid Managed Care44
Enrollment Packet: Additional InformationJune 25, 2019 / NC Medicaid Managed Care45
Reminder PostcardJune 25, 2019 / NC Medicaid Managed Care46
Key Takeaways47
How Members EnrollThere are several ways that members can enroll. Online and mobile app arerecommended.ONLINEMOBILE APPCALLMAILEnroll using a computerby going toncmedicaidplans.gov,where they can alsochat with an EnrollmentSpecialistAvailable on Android oriPhoneEnroll by speaking withan Enrollment Specialistvia phone at1-833-870-5500(the call is free)Language lines areavailable.TTY 1-833-870-5588Mail completed form toNC MedicaidEnrollment BrokerP.O. Box 613Morrisville, NC 27560Or fax the completedform to 1-833-898-9655June 25, 2019 / NC Medicaid Managed CareTo get the free app,members should searchfor NC MedicaidManaged Care in GooglePlay or the App Store48
For More InformationABOUTELIGIBILITYContact their local DSSFind contact informationat ncdhhs.gov/localdssABOUT NCMEDICAID DIRECTBENEFITSAND CLAIMSCall the Medicaid ContactCenter toll free:1-888-245-0179ABOUT CHOOSINGA PLAN OR PCPAND ENROLLINGGo toncmedicaidplans.gov(chat available)Use the NC MedicaidManaged Caremobile appCall 1-833-870-5500(the call is free)(TTY: 1-833-870-5588)ABOUT NCMEDICAIDMANAGED CAREPLAN ORBENEFITSCall their Health Plan49
Health Plan Contact InformationHealth TTY: (TTY: 711)www.HealthyBlueNC.com1-844-594-5070(TTY: : -552-3876(TTY: 711 or 1-833-552-2962)Carolina Complete Health will be available in Phase 2 starting on October 14, 2019. It will only be offered to people who live in these counties: Alexander,Anson, Bladen, Brunswick, Cabarrus, Catawba, Cleveland, Columbus, Cumberland, Gaston, Harnett, Hoke, Iredell, Lee, Lincoln, Mecklenburg, Montgomery,Moore, New Hanover, Pender, Richmond, Robeson, Rowan, Sampson, Scotland, Stanly, UnionJune 25, 2019 / NC Medicaid Managed Care50
Questions?
Thank you!
Thank youThank you for attending today’s webinar.As a reminder, we will email a link to the webinar slides and recording to all attendees.You can also find the webinar posted online on the Medicaid Transformation ansformation
An Enrollment Broker is an entity that performs choice counseling or enrollment activities, or both. Eligibility services are completed by NC Medicaid, not by the Enrollment Broker. Enrollment Brokers and subcontractors must not have direct or indirect financial ties to any Health Plan or healthcare provider that furnishes services in the