Transcription
Your Guide ThroughChemotherapy
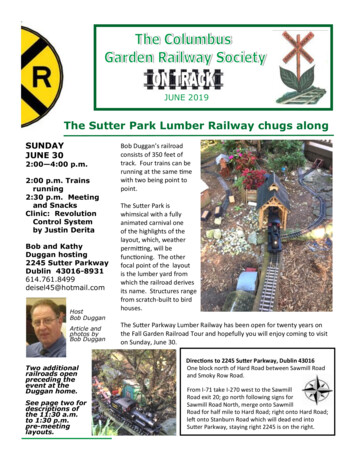
Dear Sutter Patient,Thank you for choosing the Sutter network to care for you during yourcancer journey. We understand that a cancer diagnosis can be veryfrightening and impact all areas of your life. Please know that you’resurrounded by caring and compassionate oncology clinicians and supportstaff throughout Northern California. We’ll work to make sure yourexperience is one where you feel listened to, safe and engaged in your care.This chemotherapy education notebook was created by a team of Sutternetwork oncology clinicians and is based on feedback from you, ourpatients. With your input, we’ve focused on what we believe is mostimportant for you to know about managing your chemotherapy treatmentand feeling your best throughout therapy. We hope to help you avoidside effects, but when that isn’t possible, we will help you manage yoursymptoms to feel well. Here we offer you education, tips and ideas tomaintain your energy and even grow stronger during treatment. If you haveadditional questions after reading through this booklet, your care team isalways here to answer them.We wish you the very best experience on your cancer journey and will becheering you every step of the way.Kindest Regards,Your Oncology Team
Table of ContentsWelcome to Sutter Infusion. 2Chemotherapy and Immunotherapy. 5Understanding Your Blood Counts.10Infection.12Fatigue.16Nausea and Vomiting .18Constipation .20Diarrhea .22Hair, Skin and Nail Changes .24Peripheral Neuropathy.27Cancer Pain .28Sexuality, Fertility and Chemotherapy .31Mind, Body and Spirit .32Additional Resources.33
Welcome toSutter InfusionAcross Northern California, we have multiple locations wherepatients can receive their treatment. No matter which you choose,your highly skilled team of clinicians and supportive staff will takewonderful care of you.Alta Bates SummitMedical Center Infusion2001 Dwight WayBerkeley, CA 94704510-204-1591Memorial Medical CenterInfusion Center1700 Coffee RoadModesto, CA 95355209-530-3673California Pacific MedicalCenterPacific Heights CampusBryan Hemming CancerCare Infusion Center2351 Clay St., Suite 134San Francisco, CA 94115415-600-3073Mills-Peninsula MedicalCenterDorothy Schneider CancerCenter100 S. San Mateo DriveSan Mateo, CA 94401650-696-4509Eden Medical CenterUniversal Care UnitAmbulatory Infusion20103 Lake Chabot RoadCastro Valley, CA 94546510-727-32482PAMF Infusion Fremont3200 Kearney St.,Third FloorFremont, CA 94538510-498-2335PAMF Infusion MountainView701 E. El Camino Real,First FloorMountain View, CA 94040650-934-7600PAMF Infusion Palo Alto795 El Camino Real,Lee Building, Level APalo Alto, CA, 94301650-853-2905PAMF InfusionSanta Cruz2850 Commercial CrossingSanta Cruz, CA 95065831-460-7355PAMF Infusion Sunnyvale301 Old San Francisco Road,First FloorSunnyvale, CA 94807650-934-7600
Sutter Amador HospitalInfusion100 Mission Blvd.,Suite 2500Jackson, CA 95642209-257-7480Sutter Auburn FaithHospital Infusion11710 Education St.Auburn, CA 96602530-886-6760Sutter Coast HospitalInfusion Center780 E. Washington Blvd.,Building CCrescent City, CA 95531707-464-8998Sutter Davis HospitalInfusion2000 Sutter PlaceDavis, CA 95616530-757-5124Sutter Medical Center,Sacramento Infusion2800 L St., Suite 320Sacramento, CA 95816916-887-4977Sutter Roseville MedicalCenter Infusion8 Medical Plaza Drive,Suite 250Roseville, CA 95661916-878-4960Sutter Santa RosaRegional Hospital Infusion3883 Airway Drive,Suite 300Santa Rosa, CA 95403707-521-7750Sutter Solano CancerCenter100 Hospital DriveVallejo, CA 95489707-551-3400Sutter Tracy CommunityHospitalInfusion Room1420 N. Tracy Blvd.Tracy, CA 95376209-832-60993
problemEvery time you talk with a health care providerASK THESE 3 QUESTIONS123What ismy mainWhat doI needto do?Why is itimportantfor me todo this?AskGood Questionsfor Your Good HealthInstitute forHealthcareImprovement4Me3ihi.org/AskMe3Ask me is regestrated trademark scnded to the instubate foe healthcare improvement IHI aske me availablefor distribution Use of Ask me 3 materials does not mean that the distributing organization is affaied with distributed IHI
Chemotherapy andImmunotherapyWhat is chemotherapy?Chemotherapy uses medicines to kill cancercells. It’s often called “chemo.” Chemo mayslow cancer growth, stop cancer fromspreading or help get rid of the cancer.Chemo can be given at different locations,such as a hospital, a doctor’s office or aclinic. Sometimes chemo treatments can bedone at home.You may get chemo in “cycles.” This meansthat you get a number of treatments overa set period of time. Then you take a breakbefore you start again.Chemo helps treat many kinds of cancer,but it can also affect healthy cells along withthe cancer cells. This is why some types ofchemo cause side effects, such as nausea,losing your hair or feeling tired.What is immunotherapy forcancer?Immunotherapy helps treat cancer bysupporting the body’s immune system.This type of treatment can restore, boost orredirect the immune system. Because of theway it works, it may also be called targetedtherapy or biotherapy.Immunotherapy for cancer includesmedicines (checkpoint inhibitors,monoclonal antibodies, interleukins),immune cell therapies (CAR T-cell therapy)and treatment vaccines.What are the goals of therapy?The goals of treatment with chemotherapyand immunotherapy include curing yourcancer, shrinking cancer prior to surgery andcontrolling the cancer or its symptoms.5
Self-Care DuringTreatmentHealthy Eating, Exercise,Mindfulness, Social SupportSome people want to learn more about howto care for their bodies and mental healthwhen learning of a cancer diagnosis orduring treatment. Below, we’ve suggesteda few ways to help you feel stronger in yourmind, body and spirit.Physical ActivityPhysical activity can help reduce pain andfatigue. It can also prevent muscle spasmsand stiffness in your joints. Stretching andrange-of-motion exercises can help you staystrong, flexible and mobile.Being physically active also can help withyour emotional and mental health. It may behard to be active when you don’t feel well,but if you can, going for a walk or a swimmay help you feel better, especially duringcancer treatment.Be sure to talk to your doctor before youincrease your level of physical activity.If you don’t know how to get started, pleasespeak with your team about a referral tophysical therapy. Therapists can work withyou to find exercise based on how you feelright now.CounselingCounseling can help you find ways to copewith your cancer and any discomfort fromcancer treatments. Sometimes counselingmay also be helpful for your family.Depending on the therapist you work with,they may be able to offer music therapy, pet6therapy, dance therapy or art therapy eitherin individual or group sessions.If this is something you would be interestedin, please talk with your care team foroptions close to home or work.Support GroupsAvailable either at your hospital, cancercenter or in your community, support groupsoffer you the chance to meet other peoplewho are going through similar experiences.Typically groups focus on a particular typeof cancer and are meant for either patientsor caregivers. Support groups are offeredin person and virtually. Please talk withyour treatment team about support groupsavailable to you.MeditationThis usually involves slow, regular breathingand sitting quietly for at least 15 to 20minutes. There are multiple options toparticipate in meditation, including podcasts,apps and different websites.AcupunctureVery thin needles are inserted into the skinat certain points on the body. Please talkwith your care team to see if this treatmentis available at your cancer center.BiofeedbackThis method uses the mind to help controla body function that the body normallycontrols on its own. These functions includemuscle tension and blood pressure.Before you try a complementary treatment,talk to your doctor. These treatments aren’tmeant to take the place of standard medicaltreatment.
Nutrition Guidelines forChemotherapyEating and drinking correctly is importantafter chemotherapy to prevent unwantedside effects and to help support the body forrecovery.EatingHere are some general guidelines forchemotherapy treatment. Ask your dietitianfor your specific guidelines. Most willrecommend a whole-foods diet, limitingthe amount of processed sugars and friedfoods.Eat a regular meal or snack prior to goingto chemotherapy, avoiding spicy or greasyfoods. Be sure to ask how long yourtreatment will take as you may want to packsnacks or a meal.Some examples are: A salad with protein like turkey or chicken Cereal, fruit and milk Eggs and toast Fresh fruit and cottage cheese or yogurt Soup and sandwichDuring your chemotherapy treatment, youmay want to snack on crackers and low-acidjuices (apple, grape or fruit nectars) as wellas broth-based soups (not cream-based).You might enjoy hard candy like lemondrops or mints to mask unpleasant tastes.Be gentle with your stomach afterchemotherapy. What you put in may helpminimize issues with nausea and vomiting.Here are some simple guidelines of what toeat, drink and avoid:Eat Baked or broiled meats, chicken orfish. Cool foods with less odor. Small meals frequently. Whole-food diet. Try to stay awayfrom pre-packaged, highly processedfoods.Drink A variety of fluids, not just water. Fluids in between meals. Gatorade has dyes and lesselectrolytes than we recommend.Use Pedialyte instead. Low-acid, non-citric juices, such asapple or grape juice. Small amounts frequently.Try Not to Eat/Drink Acidic foods (tomatoes, orange juice). Fried foods. Raw foods (eggs, fish, meat, dairy). Spicy foods.Some patients have other dietaryconsiderations prior to being diagnosedwith cancer, such as with diabetes, Crohn’sdisease and heart disease. Some cancersare also more irritating to the stomachbecause of where the cancer is along thegut or sometimes because of treatment. It’simportant for you to talk with your doctorabout your concerns and to ask for a referralto a dietitian. They’re here and available tosupport you on your journey to healing.7
DrinkingDrinking fluids will help you to stay hydratedand feeling good. It may also help youreduce feelings of tiredness and pain.SavoryJuices BrothApple juiceMilk Chicken noodle soupApricot nectarPeach nectar Chicken rice soupCoconut waterWatermelon Miso soup Other broth-based soups only, nocreamed-based soupsWater-Based Teas, such as herbal, black,green or ginger tea Water8Try to drink at least 8-10 glasses of fluidevery day. The following chart will give youoptions and ideas:Grape juiceOther IdeasGinger alePopsiclesJell-OSherbetPedialyte
Taste ChangesChanges in taste are common with cancerand cancer treatment, especially if you’rereceiving radiation therapy to the neck andmouth area. Taste changes are usually atemporary condition, and your team will alertyou if this is something you may experienceduring treatment. Common complaints areof food having no taste or tasting too sweet,too bitter or metallic. Losing your taste maymake it harder to eat, which can causeweight loss. With time and healing, tasteoften returns to normal.What you can do if foods taste toobitter: Add honey or sweetener to foods anddrinks. Add sweet fruits to meals. Alternate protein sources might beblandly prepared chicken and fish, mildcheeses, eggs, dairy products or tofu. If meat tastes too bitter, eat it cold or atroom temperature.What you can do if foods taste toosweet: Avoid fruit juice and other sweet drinks, ordilute drinks with half water or ice. Avoid sweet fruits. Vegetables may bemore appealing. Consider a squeeze of Meyer lemon onyour foods to disguise the strong sweetflavor.What you can do if foods taste off: Add plain yogurt or sour cream to soupsand sauces to disguise off tastes. Choose bland foods. Eggs, cheeses(including cottage cheese), hot cereals,puddings, custards, tapioca, toast,potatoes, rice and peanut butter are lesslikely to taste strange than foods withmore distinctive flavors. Drinking water, tea, ginger ale and fruitjuices mixed with club soda may removesome of the strange tastes in yourmouth. It might also help to suck on hardcandies, such as sugar-free mints. Marinating foods may make themtaste better. Marinate meats or fish inpineapple juice, wine, Italian dressing,lemon juice, soy sauce or sweet-and-soursauces.9
UnderstandingYour Blood CountsHow does your treatment affectyour blood cells?Cancer occurs when cells in the bodydivide and grow at an abnormally fast rate.Chemotherapy is a common treatmentfor many of these cancers. Chemotherapyworks by stopping or killing these cells thatdivide more frequently. However, it doesn’thave the ability to select only cancer cells fordestruction. There are some healthy cellsin the body that also rapidly divide and aredestroyed by chemotherapy. These includethe body’s bone marrow (blood cell factory),gut, skin and hair cells.How is a low blood count treated?All parts of the blood are produced by yourbone marrow inside your bones. There aremedications that can stimulate your bonemarrow to produce more blood cells. Yourdoctor may also consider a blood or platelettransfusion. Your doctor will discuss thesetreatment options with you depending onyour individual condition.Understanding YourChemistry TestThis test measures chemicals in the bodyand gives your doctor information on howyour kidneys, liver and other organs areworking. Tests may include: Alanine aminotransferase (ALT) –Liver function Albumin – Liver function Alkaline phosphatase – Liver functionand others Aspartate aminotransferase (AST) –Liver function BUN – Kidney function Calcium – Bones and muscles (includingheart) CO2 (carbon dioxide) – Several organs Creatinine – Kidney function Serum chloride – Kidney function andothers Serum potassium – Heart and muscles Serum sodium – Kidney function andothers Total bilirubin – Liver function10
What is being monitored by acomplete blood count (CBC)?A CBC is ordered by your doctor to monitorthe effects of chemotherapy on your bloodcell counts. There are three main parts ofthe blood that are monitored – red bloodcells, white blood cells and platelets. Eachpart has a different function:Red Blood Cells (RBCs)The RBCs consist of hemoglobin andhematocrit (H/H), which carry and deliveroxygen from your lungs to the entire body. Alow H/H is called anemia. The symptoms ofanemia may include: Being tired or weak Chest pain Dizziness Light headedness Pale-colored skin Shortness of breathWhat should you do if you’reanemic? Get plenty of rest. Move slowly to avoid getting dizzy. Report increasing fatigue and shortnessof breath to your nurse or doctor. Schedule short periods of activity andrest between activities.PlateletsThe function of platelets is to form clotsand to prevent uncontrolled bleeding. A lowplatelet count is called thrombocytopenia.Symptoms of a low platelet count mayinclude: Bleeding gums. Dark/black colored bowel movements. Easy bruising. Nose bleeds. Red/purple spots on your skin or in yourmouth.What should you do if your plateletcount is low? Avoid contact sports. Check with your doctor before seeing thedentist. Clean your nose by gently blowing. Don’t use aspirin or aspirin-likemedications. Shave with an electric razor. Use a soft toothbrush. Use caution with nasal swabbing (Flu/COVID screening).White Blood Cells (WBC)The function of WBCs is to fight offinfection. The neutrophil is the mostimportant part of the WBC, that helpsyour body to fight infection. The absoluteneutrophil count (ANC) is monitored by yourdoctor to determine how well you’ll be ableto fight off infection. A low neutrophil countis called neutropenia. The lower your ANC,the higher your risk of infection.11
InfectionInfection can be prevented for manypatients. Throughout treatment, our goal isto avoid infection in any part of your body.We can prevent and minimize the problemsassociated with infection by making youmore aware of how to prevent it.Why does infection happen withcancer treatment? Chemotherapy affects the productionof new white blood cells in your bonemarrow. Your white blood cells (WBC) are yourbody’s defense against infection. When your white blood count is low,you’re more likely to get an infection. Central lines and urinary catheters aremore likely to become infected if yourwhite blood cell count is low. Your doctor or nurse will tell you whenyour white count is low.Signs of Infection Fever with a temperature 100.4 F orabove Areas of redness or tenderness Chills or shakes Sore throat Mouth sores Productive cough with yellow or greensputum12 Pain/burning or frequent urge to urinate Change in mental state or confusionIt’s important to call your doctor for thefollowing problems: Temperature above 100.4 F Sore throat, cough, congestion, chills,shaking (signs of infection) Shortness of breath that is new Mouth sores or pain when swallowing A cut in your skin has become reddened,swollen or is draining pus More than three loose, watery stools in24 hours Burning or pain with urination or you haveto urinate often or urgently Pain or soreness at injection or IV siteMonitor for Fever By monitoring your temperature daily, notonly will you know right away if you beginto have a fever, but you’ll also learn what anormal temperature is for you. Although a normal oral temperature isrecognized as 98.6 F, an individual’stemperature may be slightly higher orlower. Check your temperature any time yoususpect you may have a fever, such asif you feel ill, feverish, chilled or you’rehaving cold sweats. Keep a record ofthese temperatures to share to your team.
Food Safety Don’t eat or drink items that are past thefreshness/sell by date. Don’t eat foodsthat have moldy spots, even if you cutthem out. Hand Sanitizers may be used unlesshands are visibly soiled or if your skin isdry and cracked. Keep your body clean by showering orbathing daily. Don’t eat raw or undercooked eggs, meatand seafood, including sushi. Avoid people who are sick (colds, flu,chicken pox, shingles or other illness). Wash your unpeeled fruits and vegetableswith soap and water to eliminate germs. Be gentle and “dab” rather than wipeyourself after a bowel movement. Avoid crowded places or large gatheringswhere you can be exposed to germs frompeople coughing and sneezing near you.If you can’t avoid crowded places, wear amask. Plan activities during non-crowdedtimes (early morning). Instead of toilet paper, use a baby wipeor squirt of water from a spray bottle toclean yourself. You also need to stay away from adults orchildren who just had a “live virus” vaccinefor chicken pox or polio for 14 days. Tell your doctor/nurse if your bottom issore, bleeds or if you have hemorrhoids. Avoid contact with animal waste,including litter boxes, birdcages and fishtanks.Toileting Safety Women should wipe from front to back.To Prevent Infection, ProtectYourself The single most important thing you, yourfamily and friends can do is to wash yourhands frequently. Use soap and warm water, lather well andrub all portions of the hand thoroughly for20 seconds (sing "Happy Birthday" or the"ABCs" song twice). Insist on frequent, thorough handwashing for every member of the family:- After using the toilet, blowing yournoseFlu Vaccine Discuss timing of your vaccine with youroncologist. Flu vaccines are recommended forcancer patients and their families.COVID-19The COVID-19 pandemic created a rapidlychanging public health issue. Talk to yourdoctor about the current COVID-19 situationin your community and what the latestguidance is for patients like you.- After handshaking or touchinganimals- After changing a diaper- Before eating or preparing food toeat13
How to Handrub?RUB HANDS FOR HAND HYGIENE! WASH HANDS WHEN VISIBLY SOILEDDuration of the entire procedure: 20-30 secondsWorld HealthOrganization14Patient SafetySAVE LIVESA World Alliance for safety health careClean Your Hands
How to Handwash?WASH HANDS WHEN VISIBLY SOILED! OTHERWISE, USE HANDRUBDuration of the entire procedure: 40-60 secondsWorld HealthOrganizationPatient SafetySAVE LIVESA world alliance for safety health careClean Your Hands15
FatigueFatigue is commonly felt by people withcancer. It can be caused by many things,such as the cancer, the effects of treatment,emotions, stress, poor nutrition and sleepdisturbances. Being aware of the signalsyour body provides is important in theprevention and management of fatigue.Many people describe fatigue as feelingweak, weary, worn out, heavy or slow.Resting doesn’t always help. People feelfatigue in different ways. You may feel more/less fatigue than someone else who has thesame type of chemotherapy.Think of your body as an energy bank. Youneed to deposit rest and nutrition at thesame time you withdraw energy for dailyactivities. Your body is working hard torecover as you receive treatment and forsome time after treatment stops.Be aware of what is most importantevery day. You probably won’t be able toaccomplish everything you usually do. Dowhat you must do and then ask others forhelp.16Preventing FatigueEven if you can’t exercise like you used to,getting up and moving around every daycan make a big difference. A short 5- or10-minute walk can help! Many peoplewith cancer who participate in an exerciseprogram say they feel better and have moreenergy. They also report fewer side effectsfrom their treatment.Remember, even small amounts of activitycan help put energy into the bank.General Exercise GuidelinesTypes of exercise: Walking, yoga, bikeriding, swimming, active housecleaning andgardening count toward exercise.Frequency of exercise: Ideally, you shouldtry to exercise at least three to four times perweek. You don’t need to be in a structuredprogram. Simply walking a few times a weekis good exercise.Length of exercise: You may need to startout with only 5 minutes at a time and slowlywork your way up to a comfortable exerciselevel for you. Use your own judgment andhow you’re feeling to guide you.
Precautions To TakeTips To Reduce Fatigue Avoid exercising outdoors in very cold orvery warm weather.Relax. You might want to try meditation,prayer, yoga, guided imagery, visualization orother ways to relax and decrease stress. Forideas on relaxation exercises, see “Learningto Relax” at . Don’t exercise without permission fromyour doctor if your platelet count is below50,000. If you have an infection or a fever, waituntil you feel better. Begin slowly. Take it easy the day of yourchemotherapy. Postpone exercising untilanother day. You should never feel faint, dizzy,exhausted or short of breath whenexercising. If this happens, you’re workingtoo hard and should slow down.Benefits of Exercise Helps with sleep Improves appetite Improves your mood Increases energy Increases strength and endurance Strengthens muscles and bones Strengthens your heartIf you’re having trouble getting started, askfor a physical therapy referral.Plan time to rest. You may feel better whenyou rest or take a short nap during the day. Ifyou nap, try to sleep for less than one hour.Keeping naps short will help you sleep betterat night.Sleep at least eight hours each night. Thismay be more sleep than you needed beforechemotherapy. You’re likely to sleep better atnight when you’re active during the day. Youmay also find it helpful to relax before goingto bed.Let others help. Ask family membersand friends to help when you feel fatigue.Accept their help. Often, your friends andfamily are looking for ways to support you.Learn from others who have cancer.People who have cancer can help by sharingways that they manage fatigue. One wayto meet others is by joining an in-person oronline support group.Talk with your doctor or nurse. Your doctormay prescribe medication that can helpdecrease fatigue, give you a sense of wellbeing and increase your appetite. Theymay also suggest treatment if your fatigueis from anemia, and can help you findresources like support groups.17
Nausea andVomitingNausea and vomiting can be predicted andprevented for many patients. Our goal is foryou to have no nausea or vomiting. It can beprevented and controlled with medicationsand other non-medical interventions. Fill all medications prescribed for you.TermsDuring Treatment Dry heaves – Your body is trying to vomiteven though your stomach is empty.If your treatment is likely to cause nauseaand vomiting, you’ll receive medications withyour treatment to prevent these side effects.The infusion nurse will either give you pills ormedication through your IV. Nausea – Feeling sick to your stomach,like you’re going to throw up. Vomiting – Throwing up.Many things can cause nausea andvomiting, such as chemotherapy, painmedicine (opioids like Vicodin andmorphine), anesthesia from surgery,movement (motion sickness), indigestion,being nervous (feeling like butterflies in yourstomach), constipation and radiation to thestomach area or brain.Prevention and ManagementBefore Treatment Begin eating simple, plain foods (avoidgreasy, spicy, high-fat foods) before andon the day of your chemotherapy. Seenutrition guidelines on page 6.18 Stock your home with foods and fluidsthat are easy to digest. Talk to your doctor about alcohol useduring and after treatment.After TreatmentIt’s very important that you take themedications your oncologist has prescribedto prevent nausea and vomiting. These mayinclude: Aprepitant (Emend) Ativan (Lorazepam) – This may causedrowsiness. Don’t drive while taking thisdrug. Compazine (Prochlorperazine) Decadron (Dexamthasone) Zofran (Ondansetron)
Because nausea and vomiting duringtreatment for cancer can be caused bymany things, you may need more than oneof these medications to feel better. Pleasetake these as directed by your medical team. Distraction – Try reading, watching aTV show you love. Say “yes” to bingewatching!Some patients use complementarytherapies, such as medical cannabis(marijuana) for easing nausea and vomiting.In many cases, this is OK. Please speak withyour doctor before starting; your doctor mayhave a recommendation. Ice chips or popsicles.After You Go Home Don’t lie down for one hour after eating. Don’t skip a meal or snack, eat somecrackers at least every one to two hours. Drink eight to 10 eight-ounce glasses offluids to help flush the chemotherapy outof your system. Drink and eat foods at room temperature(not hot and not cold). Eat five to six snacks each day ratherthan three big meals. Eat simple, plain foods for the next two tothree days, allowing your stomach to restand recover. Keep saltines nearby and eat two to threecrackers before getting out of bed in themorning.Things To Try Acupuncture – Your doctor may be ableto refer you to someone who specializesin cancer treatment. Aromatherapy with ginger, peppermint,lavender, fennel seed or lemon oil. Ginger (ginger candy, ginger tea, gingerale, ginger lozenges). Keep a fan blowing cool air to your face/upper body. Listen to your favorite music. Meditation. Motion sickness wrist bands(accupressure). Peppermint tea or other peppermintproducts (gum, mints).Eating and drinking correctly is importantafter chemotherapy to prevent unwantedside effects and to help support the bodyduring recovery.You should be able to drink plenty of fluidsand eat small amounts of food withoutnausea or vomiting.If you’re still having problems despiteprevention, call your doctor or nurse. We’rehere to help you.Indigestion/HeartburnYou may experience heartburn or indigestionat times for several weeks during treatment.This is often a result of the medications wegive you to stop the nausea. We suggestkeeping Mylanta , Tums or Rolaids in the house. If heartburn or indigestioncontinues, please tell us so we can give youa prescription for something stronger. Deep-breathing exercises.19
ConstipationConstipation is a common problem forpatients undergoing chemotherapy.Treatment can alter one’s appetite, the wayfood moves through the body and how thebody eliminates waste. Signs and symptomsof constipation include: Bowel movements that are small andmarble-like. Hard bowel movements that are difficultto pass out of the body. Infrequent to almost no bowelmovements. Pain/pressure in the stomach thatmay move down lower to your bottom(rectum). Straining for a bowel movement.Causes of constipation include differentmedications and medical conditions. If leftuntreated, constipation may get worse andcause a blockage that may need medicaltreatment. It’s very important to be sureyou’re having normal bowel movements forby your own standards. Just remember it’sbest to have soft, formed stool that’s easy topass out of your body at least every two tothree days.Dietary and LifestyleManagement Increase fluids. Drink eight to 10 eightounce cups of liquid each day. Increase caffeine intake to stimulateintestinal muscles.20 Increase your fiber intake. Include fruitsand vegetables, whole-grain breads,cereals and pastas, legumes, nuts andseeds in the foods you eat every day. Exercise daily. At least
Sutter Coast Hospital Infusion Center 780 E. Washington Blvd., Building C . Crescent City, CA 95531 . 8 Medical Plaza Drive, Suite 250 . Roseville, CA 95661 . 916-878-4960 Sutter Tracy Community Hospital . Infusion Room . 1420 N. Tracy Blvd. Tracy, CA 95376 . 209-832-6099 . 3 . problem Every time you talk with a health care provider .