Transcription
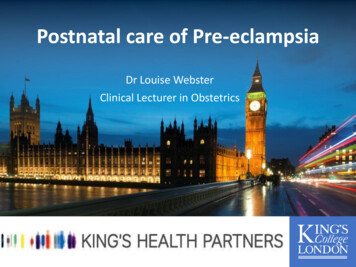
Contraceptive TechnologyUpdateSatellite Conference and Live WebcastWednesday, October 25, 20062:00 - 4:00 p.m. (Central Time)FacultyLeigh Beasley, MD, FAAFPEmory University Regional Training CenterAtlanta, GeorgiaProduced by the Alabama Department of Public HealthVideo Communications and Distance Learning DivisionProgram Objectives Describe current thinking oncontraceptive efficacy and the statusof experimental contraceptives. Describe the interrelationships ofmedical contraception methods withspecific drugs, reproductivedisorders and other health problems.Contraceptive Use in theUS: 2002 Report Percentage of men and women whoused contraception ranged from 67%(Guam) to 88% (Idaho). Women reported OC’s as thepredominant method in 49 areasfollowed by tubals, condoms andvasectomy. Men reported tubal, vasectomy, OC’s,and condoms. Note lack of “new methods” in the topfour.Program Objectives Describe the new World HealthOrganization's (WHO) medicaleligibility criteria; Intrauterine Device(IUD) and teens, IUD and PlevicInflammatory Disease (PID);spermicides; and knownthrombogenic mutations and oralcontraceptives. Discuss management of commoncontraceptive problems.Half of All Pregnancies in theUnited States Each Year riage9%Pregnancies(6.3 Million)1
The Oral Contraceptive Cycle Progestin prevents luteinizinghormone (LH) surge. Estrogen suppresses folliclestimulating hormone (FSH)and follicular development. Together, the hormones incombination OCs inhibitproliferative changes inuterus, leading to endometrialatrophy. When placebo pills are taken,a “pill period” results.OC Developments New Estrogen doses: 25mcg;Cyclessa, Ortho-Tricyclen Lo. Extended Cycle Use: Seasonale,Seasonique. Widening EC use. “Natural” estrogen pills andnonsteroidal progesterone agonist(tanaproget).Depo-Provera andBMD in Teens NIH-funded study (J. Adoles Health 2004)– 370 girls (mean age, 15).– 53 chose Depo, 165 chose OC’s (20 ugof estrogen) and 152 chose nohormonal contraception.– BMD values after 12 months. At lumber spine: -1.4%, 2.3% and 3.8%. At the hip: -2.2%, 0.3% and 2.3%.– Clinical relevance ?OC Developments New Progestin: Drospirenone;Yasmin. Berlex has obtained FDA approvalfor Yaz (20 mcg EE/3 mgdrospirenone) for BC and PMDD(unique dosing 24 days active pillsand 4 placebo pills).Depo-Provera November 17, 2004: the FDA issued a“black box” warning recommendingthat Depo-Provera be used long-term(i.e. more than two years) only if allother pharmacologic contraceptivesare not appropriate or tolerated dueto bone loss data in adult women.Effect of Contraception onBone Mineral Density Studied women ages 18-33 seekingcontraception. Injectable Depomedroxypgogesterone acetate150mg vs. 0.030 mg EE plus 0.15 mgdesogestrel vs. 0.035 mg EE plus 1.0mg norethindrone vs. controls (nohormonal contraception). Followed for 2 years.2
Effects of Contraception onBone Mineral Density Depo users-average loss from baselineof 5.7 % (in spinal BMD). Desogestrel OC-average loss formbaseline of 2.0 % (not statisticallysignificant). Norethindrone- no significant changein BMD. Controls-average gain of 2.6 % in BMD. Clinical relevance?Effect of Pregnancyand Lactation on BoneMineral Density Bone turnover is reduced in earlypregnancy, returned to normal duringthe third trimester and increased inpostpartum lactating women(Cole et al. 1987) No evidence that high parity isassociated with an increased incidenceof osteoporotic fractures in later life(Alffram, 1964; Walker et al. 1972).DMPA and Bone Health Complete recovery of BMD was notfound at all skeletal sites assessed(but would it have if followed for 2DMPA and Bone Health Three studies that indicate BMD iscomparable in former and neverusers following discontinuation ofDMPA.– Petitti DB et al (Obstet Gynecol2000;95:736-744).– Scholes D et al (Epidemiology2002; 13:581-587).– Scholes D et al (Arch PediatrAdolesc Med 2005; 159: 139-144).DMPA and Bone Health Data presented at the May 2005ACOG meeting (co-author AndrewKaunitz, MD). Loss of BMD of approximately 1%2% annually, with slower loss afterthat and substantial recoveryfollowing discontinuation (followedpatients for 2 years after DMPA wasdiscontinued).World Health OrganizationDMPA Statement July 2005: There should be norestriction on the use of DMPA,including no restriction on durationof use, among women ages 18-45years post DMPA?).who are otherwise eligible to use themethod.3
World Health OrganizationDMPA Statement Among adolescents (menarche toWorld Health OrganizationDMPA Statement Since the data are insufficient toless than 18) and women over 45, thedetermine if this is the case with longadvantages of using DMPA generallyterm use among this age group, theoutweigh the theoretical safetyoverall risks and benefits forconcerns regarding fracture risk.continuing use of the method shouldbe reconsidered over time with theindividual user.Lower Dose, SubcutaneousDepo-Provera Study compared LDSQ Depo(104mg/0.65ml) with IM Depo(150 mg/ml). Confirmed study participants wereovulatory. Received single injection andfollowed up until they ovulated(up to 12 months). 19 women who received IM and 39received SQ were evaluated.NuvaRing Non-biodegradable, flexible,transparent vaginal ring. Contains two active components:ethinyl estradiol and etonogestrel(an estrogen and a progestin). Releases 0.015 mg/day ofethinylestradiol and 0.120 mg/ day ofetonogestrel over a three weekperiod.Lower Dose, SubcutaneousDepo-Provera Ovulation was suppressed in allparticipants for at least 3 months. Median time to return to ovulationwas similar in the two groups (183days in the IM group and 212 days inthe SQ group). Dose and maximum serumconcentration are substantially lowerwith the SQ formulation so ? Lessside effects?NuvaRing : Metabolic andSafety Conclusions Minimal effect on lipid parameters. No clinically relevant effect oncarbohydrate metabolism. Minimal effect on hemostaticvariables, comparable with 30 EE/150LNG COC.4
NuvaRing : Metabolic andSafety Conclusions Low androgenic effects. No adverse effect on blood pressure. No unfavorable effects on the cervixand vagina.Nuva Ring Update Effectiveness not lower in very heavywomen (Westhoff-ACOG 2005). Continuous use can be based on a“calendar approach” since the NuvaRing is active for 35 days, not 21(Timmer et al Clin Pharmokin2000;39:233). Clinicians can obtain free fittingrings by going to www.nuvaring.comEmergency Contraception:The Nations Best-KeptSecretCalifornia Women’s HealthSurvey 6198 women (age 18-44) were asked“If a woman has unprotected sex, isthere anything she can do in the 3days after intercourse that willprevent pregnancy?”– Slightly more than said yes, 1/3rdsaid no and around 10% said theydidn’t know.California Women’s HealthSurvey– 19% of those who answered yeslisted incorrect responses to “whatcan she do?” (included RU 486 anddouche) and 7% gave ambiguousanswers (“seek medical help”).Why Everyone Should KnowAbout EC 43% of the decrease in abortions inthe US in the last 5 years has beenattributed to the use of EC. Up to 51,000 pregnancies areprevented annually by the use of EC. (Finer et al. Perspec on Sexualand Reprod health 2003) Works like LAM.5
Emergency ContraceptionMechanism of Action Inhibition of ovulation. Decreases the probability offertilization after ovulation. Changes in the endometrium(decreasing the likelihood ofimplantation). Does NOT interfere with anestablished, post implantationpregnancy.EC’s Effects on OvulationEC’s Effects on Ovulation Studied 58 women with regularmenstrual cycles (either had tubalsor IUD). Treatment regimens: two 0.75 mgdoses of levonorgestrel (12 hoursapart), single 0.75 mg dose oflevonorgestrel plus placebo ordouble dose of placebo. Randomized to take meds whenleading follicle reached a diameter of12-14 mm (Group I), 15-17 mm(Group II) and 18 mm (Group III).EC’s Effects on Ovulation Within 5 days of treatment, there was Percentage of cycle either ovualtoryno ultrasound evidence of follicularrupture (i.e., no ovulation) in 44%,dysfunction or no follicular rupture50% and 36% of cycles with 2 levo.doses, 1 dose and placebo. Ovulatory dysfunction (disorderedsurges in LH and FSH) in 35%, 36%and 5%.EC’s Effects on Ovulation Caution in interpreting results: usedhormonal parameters and ultrasoundand did not test EC’s efficacy. 13% of women with dominant follicle(i.e. 18 mm) did not ovulate whentreated with placebo. Single dose used in this study wasnot the “single dose” used intreatment studies.– (Contraception 2004 Dec.)was similar in with 3 regimens inGroup 1, significantly higher withlevo than placebo in Group II andsignificantly higher with one doselevo than placebo in Group III.Emergency Contraception Most effective if taken within 72hours of unprotected intercourse(the sooner the better). New data suggests equaleffectiveness if both doses are takentogether and may be used up to 120hours after unprotected intercourse. EC treatment is indicated regardlessof the cycle day on whichunprotected intercourse occurred.6
Emergency Contraception No absolute contraindications. Initiate long term contraceptionimmediately following EC(emergency contraception does NOTcontinue to prevent pregnancyduring the rest of the cycle).Mirena – A LevonorgestrelReleasing System T-shaped frame, 32 mm in length,that holds a cylinder that containslevonorgestrel. Resumption of next menstrual cycle. Releases levonorgestrel into theuterine cavity at a rate of 20 mcg aday. Over the counter status. Approved for five years of use.Plasma concentrationsconcentrations (pg/mL)PlasmaPlasma Concentrations ofLevonorgestrelMirena – A LevonorgestrelReleasing System Safety:90008000– Ectopic pregnancy7000 One of 5 contraceptive failuresassociated with the Mirena is anectopic pregnancy, resulting inan annual ectopic pregnancyrate of 0.02%.6000500040003000200010000LNG IUSImplantMini-pillCombined OCsMirena – A LevonorgestrelReleasing SystemPercent Changes in bleeding pattern:– Initially there is an increase inbleeding days (menstrual days andintermenstrual spotting dayscombined).– Irregular spotting during the first 3-6months.– Bleeding may remain irregular insome women.– 20% will become amenorrheic withinthe first year of use.LNG IUS as Alternative ctomyLNG IUSMedical Therapies7
Paraguard Lasts 10 years. Highly effective. Has no systemic effects (e.g.headaches, acne). Most women have regular menses. Women may experience increasedduration of menses and increasedamount of bleeding.Perhaps the Copper IUD isPermanent, ReversibleContraception? WHO reported the copper IUD waseffective for 12 years (contraception1997;56:341). Brazilian study followed women upto 16 years of use.this study needscorroboration. Explusion (? causedby fibroids?) may be a concern(contraception 2005 Nov; 72:337-41).Ortho EvraContraceptive Patch Once-a-week combination hormonalpatch. Changed on the same day of the week,three times a month, with the fourthweek patch-free. Carrier for ethinyl estradiol andnorelgestromin.– EE – 20 µg released daily.– Norelgestromin - 150 µg released daily.Perhaps the Copper IUD isPermanent, ReversibleContraception? In 1984, the FDA approved thecopper IUD for 4 years of use. Eventually the FDA said it was “goodfor up to 10 years.”Paraguard Package Insert The new insert does not recommendthat this IUD be avoided by womenwho are:– Nulliparous.– Have a history of PID.“Seventeen Deaths in Usersof Ortho Evra Patches” In October 2004, AP found 17 deathsamong users of the Ortho Evra patch. We know NOTHING about thedenominator data and very little aboutthe numerator number. Two epidemiological studies mayreveal more about this rare butserious complication. Biologic plausibility.8
FDA “Bolded” Message“You will be exposed to 60% moreestrogen if you use Ortho Evra than ifyou use a typical birth control pillcontaining 35 mcg of estrogen. Ingeneral, increased estrogen exposuremay increase the risk of side effects.However, it is not known if there aredifferences in the risk of serious sideeffects based on the differencesbetween Ortho Evra and a birth controlpill containing 35 mcg of estrogen.”Weight and Riskof OC Failure NICHD-sponsored study. 618 OC users (2822 women-years OCuse).– 106 confirmed pregnancies. Women in highest body weightquartile ( 70.5 kg or 155 lbs) had 1.6x significantly increased OC failurecompared to women who weighed 155 lbs.Overweight Women Are atIncreased Risk for OC Failure Study in Seattle: 248 women becamepregnant while using OC’s and 533age-matched controls did not. Odds of becoming pregnant while onOC’s were 58% higher for womenwith BMI’s 27.3 and were highestfor women with BMI’s 32.2.–(Obstet Gynecol 2005 Jan.)Distribution of Pregnancies byBaseline Body Weight Deciles(n 3319 subjects)DecilePregnancies (N)1 (334)2 (285)3 (354)4 (256)5 (433)6 (346)7 (276)8 (379)9 (304)10 (352)WeightRange (kg)Total 5252 - 5555 - 5858 - 6060 - 6363 - 6666 - 6969 - 7474 - 80 80(80- 85)(85- 90) 90 (N 83)1200201027115Weight and Riskof OC Failure Risk in women with the highestbody weight and taking low- ( 50mcg EE 2.6x) and very low-dose ( 35 mcg EE 4.5x) OCs. Findings suggest that high bodyweight may compromise oralcontraceptive effectiveness.Contraceptive PatchPrecautions Body weight 198 lbs. (90 kg)– Results of clinical trials suggestthat the contraceptive patch maybe less effective in women withbody weight 198 lbs (90 kg) thanin women with lower body weights. No other changes. Consider body weight in OC usersalso.9
Single-Rod ImplantContraceptive: Description Single 40-mm 2-mm rod. Rod is made of ethylene vinyl acetatecopolymer. Contains 68 mg of etonogestrel (3keto-desogestrel), the activemetabolite of desogestrel, andcomes in disposable sterile inserter. Inhibits ovulation during the entiretreatment period. Effective for 3 years.Single-Rod ImplantContraceptive Efficacy No pregnancies during 1200 womanyears of exposure (Pearl Index, 0;95% CI 0.0-0.2). Effective contraception that lasts for3 years.FDA Approved July 2006 Implanon– Return to fertility – 94% of womenovulated within 3 weeks of removal.– Side effects. Changes in vaginal bleeding (30%discontinuation). Amenorrhea. Weight changes (1.5%discontinuation). Acne (1.0% discontinuation).ESSURE New procedure for non-incisionalpermanent birth control. Micro-inserts are placed in thefallopian tubes to prevent pregnancy. The system is introduced with astandard hysteroscopic approachwith tubal cannulation. Can be performed without generalanesthesia.Young Teenager withSevere DysmennorrheaContraceptive Case Studies 13 year old female, never sexuallyactive. Menses began at age 11 and painlessfor 6 months. Now periods are extremely painful,causing her to miss 1-2 days ofschool/month.10
Young Teenager withSevere Dysmennorrhea Tried heat, NSAIDS, aspirin,exercise nothing works. PE- normal B/P.Would You A. Prescribe a stronger prescriptionNSAID because OCP’s are notappropriate in this age group.B. Start her on Depo Provera todecrease her menstrual bleeding.C. Do a pap smear and give herwhatever method she wants.D. Defer the Pap and start her onOCP’s.Contraception andPap Smears Never sexually active women are atVERY low risk of HPV infection.What Factors Increase theRisk of Acquiring HPV? Number of sexual partners. Cervical cancer and HPV are linked. Recent new partner (5-8 months). Comfort of young teens with their Rate of new partners per month.bodies. New pap screening guidelines.What Factors Decrease theRisk of Acquiring HPV? Limited sexual exposure.– But HPV can be acquired withoutvaginal penetration.– 8% of virgins tested positive in 24month study.– Condoms are not protective. History of herpes.What Factors Decrease theRisk of Acquiring HPV? Various studies show different resultsfor use of oral contraceptives.– Winer: current oral contraceptivesadjusted HR 1.41.– Xi:1.6 (short duration use) to 5.4 (58 mon use)2.– Moscicki: current oralcontraceptives 0.543.11
What Is the Risk forDeveloping Cervical Cancer? Approximately 10,000 cases in theUnited States per year. Cervical cancer risk is higher indeveloping countries. Incidence of cervical cancer inadolescents is essentially zero.What Screening IsIndicated? Current recommendations:– Initiate Pap testing at age 21 or 3years after initiation of sexualactivity, whichever comes first. Recommendations after vaccination:– Yet to be determined.Would you .Will HPV Resolve? Median time to resolution:– Ho (1998) 8 months– Woodman (2001) 13.7 months– Richardson (2003) 13.2 months– Xi (2002) HPV16 17.2 months“Oh my gosh, I didn’t have aperiod, am I pregnant?!” 18 year old G1P1 on OCP’s for 2years with no problems. C/O no period this month. No symptoms of pregnancy. Can I start my new pack of pillsSunday?What About Family History?A. Tell her to call back on Monday andspeak to an APRN and come in for apregnancy test. 19 year old desires contraception,but doesn’t think she can rememberto take a pill every day.B. Tell her “sure, start yourpills” ”whatever”. Family history - father had MI at age48, 29 year old sister hashypertension.C. Inquire about missed pills duringthe past month.D. Tell her to stop her pills and startthinking of baby names. Patient is a college student, nonsmoker, gets lots of exercise, normalblood pressure.12
Would You Tell HerA. You are healthy, you can startwhatever method you like.B. The NuvaRing has the lowest doseof estrogen, you should consider itwith your family history.C. With that family history, your onlychoice is non-hormonalcontraception: a P-IUD or condoms.D. The patch might be the best choicefor you, if you can’t remember totake pills.Post Partum ContraceptionA. Any method is OK to use whilebreastfeeding.B. No need to worry aboutcontraception for at least 6 monthswhile you’re breastfeeding.C. Progestin-only methods (pills, MIUD or Depo) are the best for youwhile breastfeeding.D. You could use condoms and ECwhile breastfeeding.Post Partum Contraception 21 year old, 6 weeks post partum,“fully breastfeeding”. Married. Afraid of IUD’s. Normal B/P and pelvic exam.Nausea and Contraception 22 year old G1P1 (child is 9 monthsold). No longer breastfeeding. Wants another baby when this one is3 years old. Had hyperemesis gravidarum. Normal exam and B/P.Well .Acne and Weight LossA. The Nuva Ring, M-IUD and Implanonall have low doses of hormones andmay work for you.B. You should stick with progestin onlypills since they’re working for you.C. You don’t really want another baby in3 years Do you?!!D. The pills definitely won’t make younauseated after all that nausea ofpregnancy. 18 year old G0P0 wants “that new pillthat’s good for acne and causes youto lose weight”. History of heavy periods. Plays softball and takes Motrin “alot” for pain.13
YasminYasmin 30ug EE/3 mg drospirenone Drospirenone– Spironolactone analog withantimineralocortocoid andantiandrogenic activity.whichmeans it’s also a diurectic.– Limited data in use in women 30.– Good for acne and hirsutism maybenefit patients who experience“fluid retention and bloating”during their cycles. Restricted labeling for drospirenone.– Contraindicated in women with renalinsufficiency, hepatic insufficiencyand adrenal insufficiency (patients atrisk for hyperkalemia).– Warning for patients on chronicmeds. NSAID’s (long term use). Potassium supplements. K sparing diurectics, ACE’s,ARB’s, heparin (check K level in1st month for pts on these meds).Drospirenone andWeight LossHypertension andContraception Same side effect profile. Same effectiveness. 1 open label trial.– Small amount of temporary weightloss in first 6 months, at 1 year,weight returned to baseline orslightly above. (Contraception 2000, Eur. JContra Reprod Health Care 2000)Low Dose OCP’s and CV RiskNumber of Excess Cases of MI andStroke Attributable to Smokers1220Hypertension4729Number of PregnancyRelated Deaths (per100,000 live births)101245 40 year old G3P3 on OCP’s for 5years. Annual exam.B/P is 150/98. B/P last year 120/80.Contraception and“Migraine” Headaches 19 year old nulliparous patient. c/o “migraine headaches”. B/P normal. Exam and FH unremarkable.14
OCP’s and MigraineHeadaches Increased risk of stroke in women 45years with migraines. Migraine with aura is associated withgreater risk than migraine withoutaura. WHO states prescribing OCP’s towomen 35 years with migrainewithout aura is safe. “Menstrual migraines” may improveon OCP’s.Age and ContraceptionSmoking and Contraception 34 year old G2P2 on OCP’s for 8years. Smokes -1 pack of cigarettes/day. Likes that her periods are regular onthe pill. Doesn’t want a tubal. Turns 35 years old next month.Contraception and CAM 42 year old G3P3 on OCP’s for 12years. 38 year old G2P2 with history ofhypothyroidism and irregular mensesand “perimenopausal” symptoms. Non-smoker. On Progesterone cream and “naturalthyroid replacement”. B/P normal (120/70). Worried that “condoms aren’tenough”. Doesn’t want an IUD or tubal. Partner doesn’t like condoms.Complicated Patient 30 year old G3P3 (living children 1). Had 2nd trimester fetal demise, 3rdchild born with congenital cardiacdefect. History of DVT between 2nd and 3rdpregnancy. Diagnosed with AnticardiolupinAntibody, Factor 5 Leiden. Doesn’t want “more hormones” nowthat she’s “getting better with naturalmeds”.OCP’s and InheritedHypercoagulable States In OCP user:– Risk of VTE increases 35-99 fold incarriers of Factor V Leiden.– Risk of VTE in carriers of Protein Cand antithrombin deficiency increased2 fold and 9 fold respectively.– Safety of progestin onlycontraceptives in hypercoagulablestates in unknown.15
Complicated PatientNon-Contraceptive Benefits 41 year old G7P0. 39 year old G2P2. Non-smoker. S/P BTL after last child (age 6). Regular menses. Married/monogamous relationship. Non-smoker. Heavy, irregular menses. History of OCD.What Now? 24 year old G3P2. Non-smoker. Conceived first child while on OCP’s,conceived second child while usingthe patch, got pregnant with thirdchild with P-IUD in place. Doesn’t want sterilization.Any Suggestions? 18 year old G3P2 (currently 24 weekspregnant). 2 prior C-sections, Wants a tubal thistime. Can’t remember to take pills, weighs240 pounds, doesn’t want an IUD,tried the ring and didn’t like it,doesn’t like Depo, partner won’t usecondoms.Upcoming ProgramsEnsuring Quality in the CollaborativePractice AgreementThursday, October 26, 200610:00 a.m. - 12:00 Noon (Central Time)Infection Control UpdateWednesday, November 1, 20062:00 - 4:00 p.m. (Central Time)For complete list of upcomingprograms visit: www.adph.org/alphtn16
Depo-Provera Study compared LDSQ Depo (104mg/0.65ml) with IM Depo (150 mg/ml). Confirmed study participants were ovulatory. Received single injection and followed up until they ovulated (up to 12 months). 19 women who received IM and 39 received SQ were evaluated. Lower Dose, Subcutaneous Depo-Provera Ovulation was suppressed in all