Transcription
Hand Infections: Treatment Recommendationsfor Specific TypesReid A. Abrams, MD, and Michael J. Botte, MDAbstractHand infections can be associated with considerable morbidity. Expeditious treatment is needed to minimize permanent dysfunction, loss of work, and medical cost.Hand infections can affect the skin, subcutaneous tissues, fascia, subfascial andsynovial spaces, joints, and bone. Pathogens include a variety of bacteria, viruses,yeasts, fungi, and mycoplasmata. Management frequently involves rest, elevation, incision and drainage, and appropriate antibiotic therapy. The orthopaedicsurgeon must be knowledgeable about the pertinent anatomy and how this influences the behavior of specific types of infections, the role of immunocompromise,and the importance of early mobilization.J Am Acad Orthop Surg 1996;4:219-230Expeditious and appropriate treatment can minimize the morbidity associated with infections of the hand.The typical infections that occur inthe hand include subcutaneous abscesses, septic joints, and cellulitis.The complex anatomy of the handalso makes it susceptible to uniqueinfections. Optimal care requires theclinician to understand this anatomyand how it influences the behavior ofcertain infections, so that they can berecognized and treated appropriately. Management usually necessitates adequate incision and drainage,appropriate antibiotic therapy, elevation and edema control, and mobilization. The purpose of this reviewis to discuss the general principles oftreatment and to delineate morespecifically the management of infections typically unique to the hand.MicrobiologyThe most common bacteria involvedin infections of the hand are Staphy-Vol 4, No 4, July/August 1996lococcus aureus, Streptococcus, andGram-negative species. Staphylococcus is the principal organism in 50%to 80% of infections.1 Industrial andhome-acquired injuries usually involve a single Gram-positive organism, while infections due to intravenous (IV) drug use, bite wounds,and mutilating farm injuries andthose associated with diabetes mellitus often are polymicrobial, involving Gram-positive, Gram-negative,and anaerobic species. 1-7 α-Hemolytic Streptococcus and S aureusare the most commonly isolatedpathogens in human-bite infections.1-4 Eikenella corrodens is isolatedin approximately one third of human-bite wounds. 1,3,4 Pasteurellamultocida commonly infects animalbite and scratch wounds.8 Chronicindolent infections may suggestfungi or atypical mycobacteria.Knowledge of the likely pathogens is based on the history, nature,and course of infection and can direct culture and staining requests.Routine aerobic and anaerobic cultures and Gram stain should bedone. If atypical mycobacteria aresuspected, Ziehl-Neelsen stainingand cultures at 28 C to 32 C inLöwenstein-Jensen medium shouldbe performed. 9 Examination forfungi is accomplished with a potassium hydroxide preparation. 10 ATzanck smear can be useful in the diagnosis of herpes simplex virus infection by demonstrating typical giant cells.11Antibiotic TherapyTable 1 gives some recommendations for initial antibiotic therapybased on the type of infection. Antibiotics should be administered empirically after performing culturesDr. Abrams is Assistant Professor of OrthopedicSurgery, University of California, San Diego(UCSD), School of Medicine; Chief, Hand andMicrovascular Surgery Service, Department ofOrthopedic Surgery, UCSD Medical Center; andChief, Hand and Microvascular Surgery Service,Department of Rehabilitation Medicine, Veterans Administration Hospital, San Diego. Dr.Botte is Professor of Orthopaedics, UCSD Schoolof Medicine.Reprint requests: Dr. Abrams, Department ofOrthopedics, University of California, SanDiego, 200 West Arbor Street 8894, San Diego,CA 92103.Copyright 1996 by the American Academy ofOrthopaedic Surgeons.219
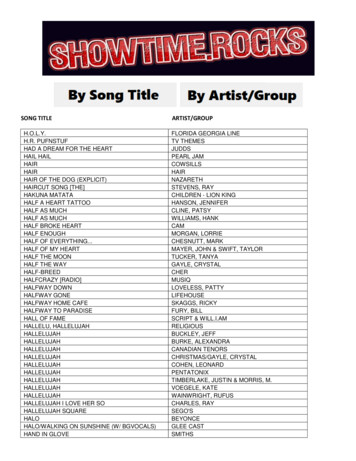
Hand InfectionsTable 1Empiric Antibiotic Recommendations for Hand Infections*InfectionPossible OrganismsAntibiotic DosageAlternative Antibiotic DosageFelon/paronychiaS aureus, oral anaerobesDicloxacillin, 250-500 mg PO q6h, orNafcillin, 1-2 g IV q4-6h, orClindamycin, 150-300 mg PO q6hCephalexin, 250-500 mg PO q6h, orCefazolin, 1 g IV q8h, orErythromycin, 250-500 mg PO q6hFlexor tenosynovitisS aureus, Streptococcus,Gram-negative rodsCefazolin, 1 g IV q8hNafcillin, 1-2 g IV q4-6h, orvancomycin, 1 g IV q12h, plusgentamicin,† orImipenem, 0.5-1.0 g IV q6hHerpetic whitlowHerpes simplex virusConsider acyclovir, 400 mg PO tidx10 daysSubcutaneous ordeep-space abscessS aureus, anaerobes, Gramnegative rodsCefazolin, 1 g IV q8h, orAmpicillin-sulbactam, 1.5 mg IV q6hNafcillin, 1-2 g IV q4-6h, plus gentamicin,† orImipenem, 0.5-1.0 g IV q6hCellulitis/lymphangitisStreptococcus, S aureusDicloxacillin, 250-500 mg PO q6h, orNafcillin, 1-2 g IV q4-6h, orCephalexin, 1 g IV q8hCephalexin, 250-500 mg PO q6h, orErythromycin, 250-500 mg PO q6hIV-drug-abuse–relatedGram-positive, Gram-nega- Nafcillin, 1-2 g IV q4-6h, plus gentamicin†tive, or mixed6 or methicillin-resistant S aureus1Vancomycin, 1 g IV q12h (for methicillin-resistant S aureus), plus gentamicin,† orImipenem, 0.5-1.0 g IV q6hHuman biteS aureus, E corrodens,Streptococcus, anaerobesCefazolin, 1 g IV q8h, plus penicillin,2-4 million U IV q4-6h, orClindamycin, 300 mg PO q6h, plusciprofloxacin, 250-500 mg PO q12h,or trimethoprim-sulfamethoxazole(Septra DS) PO q12hNafcillin, 1-2 g, plus penicillin, 2-4million U q4-6h, orAmoxicillin-clavulanate potassium,250-500 mg PO q8h, orAmpicillin-sulbactam, 1.5 g IV q6hAnimal bite‡Gram-positive cocci, anaerobes, P multocidaCefazolin, 1 g IV q8h, plus penicillin,2-4 million U IV q4-6hNafcillin, 1-2 g, plus penicillin, 2-4million U q4-6h, orAmoxicillin-clavulanate potassium,250-500 mg PO q8h, orAmpicillin-sulbactam, 1.5 g IV q6hDiabetes-relatedGram-positive cocci, Gramnegative rods5Cefazolin, 1 g IV q8h, plus gentamicin†Cefoxitin, 2 g IV q6h, orAmpicillin-sulbactam, 1.5 g IV q6hOsteomyelitisS aureus, Streptococcus,(rarely) Gram-negativerodsCefazolin, 1 g IV q8h, plus gentamicin†Nafcillin, 2 g IV q4h, orVancomycin, 1 g IV q12h, orClindamycin, 600-900 mg IV q8h, orDoxycycline, 100 mg PO q12hSeptic arthritisS aureus, Streptococcus(Neisseria gonorrhoeae)Cefazolin, 1 g IV q8h, orCeftriaxone, 1 g IV q24h (for N gonorrhoeae)Nafcillin, 2 g IV q4h, orVancomycin, 1 g IV q12h, orClindamycin, 600-900 mg IV q8h, orDoxycycline, 100 mg PO q12hTraumatic/contaminated wound§S aureus, Streptococcus,Imipenem, 0.5-1.0 g IV q6hanaerobes, Gram-negativerodsCefazolin, 1 g IV q8h plus gentamicin†* Abbreviations: PO, orally; q6h, every 6 hours; tid, three times a day.† Loading dose, 2 mg/kg of body weight; then follow serum levels.‡ Consider rabies prophylaxis.§ Consider tetanus prophylaxis.220Journal of the American Academy of Orthopaedic Surgeons
Reid A. Abrams, MD, and Michael J. Botte, MDand Gram stain. In general, initialantibiotic therapy should be aimedonly at suspected organisms, sinceexcessive coverage can select for resistant organisms, is costly, and unnecessarily exposes patients to sideeffects. Some hand surgeons feelempiric IV antibiotic coverage ofaerobic and anaerobic organisms isnecessary (e.g., cefazolin and penicillin G) for infections seriousenough to require incision anddrainage and hospitalization.12 If IVdrug abuse is involved or if the patient is diabetic, Gram-negative coverage is added (gentamicin) with theawareness that the adverse effects ofaminoglycosides include nephrotoxicity and ototoxicity.5,12,13In instances of methicillin-resistant S aureus infection, vancomycinis the drug of choice. Even when invitro sensitivity tests suggest sensitivity to cephalosporin, the organisms are still resistant; thus,cephalosporins have no role in theirtreatment.14 Only if there is a highsuspicion of methicillin resistance(e.g., recurrent infection and a history of previous methicillin-resistantS aureus infection) should vancomycin be used empirically, since it isnot as effective as the penicillinaseresistant penicillins (e.g., nafcillin)or the cephalosporins in this setting.Occasionally, methicillin-resistant Saureus is sensitive to trimethoprimsulfamethoxazole, rifampin, andciprofloxacin.Patient FactorsImmunosuppressive therapy, acquired immunodeficiency syndrome (AIDS), and diabetes mellituscan predispose patients to hand infections with typical and opportunistic pathogens. In series of handinfections in diabetic patients,5,13,15treatment was often delayed, resolution was slowed, repeated debridements often were necessary, Gram-Vol 4, No 4, July/August 1996negative organisms were common,and amputations were performedfrequently (rates of 20% to 63%), either to control infection or becauseof poor function. In diabetic patientswith renal transplants, morbiditywas particularly high.15In one series of hand infections inAIDS patients, the infections werenot opportunistic, but most hadatypical presentations and unusually virulent courses. Herpetic lesions were also more virulent anddid not resolve unless treated withantiviral agents.16Intravenous-drug abusers commonly present with dorsal hand abscesses, usually due to S aureus,which has a propensity for methicillin resistance (although this is notthe case at our institution [personalcommunication, Leland Rickman,MD, 1995]).1 Infections in IV-drugabusers and in diabetic patientshave a high incidence of Gram-negative organisms.1,6,12,15 Risk factorsfor necrotizing fasciitis include IVdrug or alcohol abuse and diabetesmellitus.17Incision and WoundManagementSuccessful management of hand infections predates the advent of antibiotic therapy. The mainstay oftreatment of deep hand infections isadequate incision and drainage. Ingeneral, straight incisions are preferred, as they cause less flap necrosis. Contaminated wounds shouldbe left open for later closure or allowed to heal by secondary intention. Certain special situations areamenable to wound closure over irrigation drainage.After initial incision and drainage, wounds are dressed with moistgauze and a bulky splint, usually immobilizing the digits in the intrinsicplus posture, maintaining the firstweb space. The wound is examinedat 24 to 48 hours, and daily wet-todry dressing changes are instituted,incorporating whirlpools or soaks toencourage continued drainage.Hand therapy is begun as early aspossible, after initial inflammationand swelling have begun to resolvebut usually before the wound hashealed.Specific Types of InfectionCellulitisCellulitis is a spreading, diffuseinflammation characterized by hyperemia, leukocytic infiltration, andedema (by definition, without abscess formation, although it may extend peripherally from an area ofsuppuration) and may be accompanied by acute lymphangitis. Although often initiated by skintrauma, ulceration, dermatitis, orlymphedema, in many instances nopredisposing condition exists. Cellulitis is most evident in the skin orsubcutaneous tissues but can involve deeper structures.Group A β-hemolytic Streptococcus is usually the causative organism. Occasionally, S aureus causesless extensive cellulitis.18The diagnosis of cellulitis is basedprimarily on clinical findings. Asubcutaneous abscess or septic jointor deep-space infection may lie beneath an apparent area of cellulitis,or there may be concern that apparent cellulitis actually representsnecrotizing fasciitis. Examinationshould concentrate on ruling outthese entities before initiating medical treatment. We have found noclinical usefulness in aspirating theleading edge of the area of cellulitisto identify an organism.An attempt to treat early cellulitiswith oral antibiotics is reasonable. Ifresolution is not apparent within 24to 48 hours, however, IV antibiotictreatment is indicated. Oral agentsof choice are penicillin V and221
Hand Infectionscephalexin. If the causative organism is not known, coverage for bothStaphylococcus (including penicillinase-producing organisms) andStreptococcus is necessary, withcephalexin being the most appropriate single drug. For patients withsevere penicillin allergies, erythromycin is an alternative.Reassessment, suspecting an underlying infection (such as a subcutaneous abscess, deep-space infection, or septic joint), is indicated ifthere is no improvement despite appropriate treatment. For extensivecellulitis, IV antibiotic therapy is indicated. Intravenous penicillin Gand cefazolin are the medications ofchoice, with cefazolin being preferred if the organism is unknown.If the patient is severely allergic topenicillin, vancomycin is an alternative.18 We prefer to observe patientsin the hospital while they are receiving IV antibiotic therapy, at least until early resolution. After discharge,IV antibiotics can be continued in thehome, if necessary. Oral agents canbe used if the causative organismsare sensitive.Subcutaneous AbscessA subcutaneous abscess usuallyresults from a puncture wound thatinoculates the subcutaneous layer.The most common organism is S aureus. Physical examination frequently demonstrates surroundingedema, cellulitis, and a central areaof fluctuation. A specimen for culture and Gram stain can be obtainedby aspiration through a large-boreneedle. Expeditious incision anddrainage before instituting antibiotictherapy can provide the necessaryspecimen while simultaneouslyachieving definitive treatment.Postoperatively, the wound is leftopen with a moist bulky dressingand subsequently managed as previously discussed. Initial empiric antibiotic treatment should be with afirst-generation cephalosporin. If222the infection originated from a farmyard or similar injury, penicillinshould be added for anaerobic coverage. If the patient is diabetic or theabscess originated from IV drugabuse, Gram-negative coverage(e.g., with gentamicin) is included.ParonychiaAcute paronychia refers to an infection beneath the eponychial fold19(Fig. 1). Disruption of the seal between the nail plate and the nail foldallows entry of bacteria into theeponychial space. The abscess thatforms can track around beneath theentire nail fold superficial to the nailplate (runaround abscess), or it cantrack proximally around and deep tothe nail plate between the nail andthe matrix.19 The infection is oftenseen after manicures, in personswith artificial nails, in nail biters,and in those with hangnails. Physical examination demonstratesswelling, erythema, and tendernessabout the nail fold. The offendingorganism is usually S aureus.Although early infections cansometimes be successfully treatedwith oral antibiotics, the safest approach is to provide drainage. Aftera metacarpal block and sterile preparation, a No. 15 scalpel, Freer elevator, or fine hemostat can be used tolift the nail fold off the nail plate toallow egress of the abscess. The nailfold is held open with a small pieceof gauze. If the abscess has spreadproximally underneath the nailplate, either a longitudinal portionor all of the nail is removed, depending on the extent of the spread. AFreer elevator or similar instrumentis placed between the nail plate andthe matrix (taking care not to damage the latter) on the involved side.The nail can then be cut longitudinally with scissors, and a portion ofthe nail can be removed, thereby decompressing the nail fold volar anddorsal to the nail plate. If necessary,the entire nail can be removed. APus beneatheponychial foldFig. 1Sagittal section of the digital tipdemonstrates the space beneath the eponychial fold under which an abscess (paronychia) can develop.small piece of gauze can maintaindrainage. An eponychial fold incision should be avoided, if possible,because an unsightly deformity ofthe nail fold can result. Within 24 to48 hours, the dressing should be removed with the aid of a warm soak.The dressing should be changeddaily thereafter, again with the useof soaks.Chronic paronychia is characterized by intermittent periods of inflammation about the eponychium.It is usually seen in patients exposedto constant moisture. Eventuallythere is separation of the nail foldfrom the underlying nail plate.There may be a cheeselike drainagefrom beneath the eponychium.Fungi (particularly, Candida albicans), atypical mycobacteria, andGram-negative bacteria have allbeen implicated.1,19 Treatment canbe frustrating, with the most successful interventions being marsupialization and total nail removal.19Application of a topical corticosteroid-antifungal ointment (3% clioquinol in a triamcinolone-nystatinmixture [Mycolog]) has been recommended as an adjunct.19FelonThe digital pad is a closed, poorlycompliant compartment containingJournal of the American Academy of Orthopaedic Surgeons
Reid A. Abrams, MD, and Michael J. Botte, MDa latticework of fascial septa extending from the distal phalanx to theskin.19 Distal phalangeal vascularitycan be compromised by distentionwithin this compartment.19 Felonsare closed-space infections of thedigital pulp. Symptoms include intense throbbing pain and swelling ofthe entire pulp, usually after penetrating trauma. The most commonorganism is S aureus.19In the cellulitic stage, elevation,soaks, and antibiotics are often adequate treatment. Once abscess formation has occurred, drainage is necessary. If inadequately treated, necrosisof the digital pad, osteomyelitis of thedistal phalanx, and extension to theflexor sheath can occur.Incisions for drainage of felonshave been controversial. Fishmouth incisions have been condemned because of resultant vascular compromise of the digital pad.19Midvolar and high lateral incisionsare preferred, with the point of maximal tenderness guiding placement19(Fig. 2). Proximal probing should beavoided because of the risk of inoculation of the flexor sheath.Postoperatively, loose-gauzepacking facilitates drainage. Removal of the dressing and reexamination are recommended in 24 to 48hours. Empiric Staphylococcus coverage should be provided until definitive cultures are available to guidetreatment. Warm soaks and dress-ABFig. 2 Recommended incisions for drainageof felons. A, Midvolar. B, High lateral.Vol 4, No 4, July/August 1996ing changes will facilitate furtherdrainage. The wound should thenbe allowed to close by secondary intention.Herpetic WhitlowThe term “whitlow” (synonymous with felon) has continued to beused when describing herpesvirushand infections. In fact, these infections are not felons, although theyare often clinically confused withthem and with paronychias. Mostoccur on the digital tip, but infections of the more proximal hand andforearm have been reported.11The causative agents are the clinically indistinguishable herpes simplex virus types 1 and 2. Infection isan occupational hazard of those exposed to orotracheal secretions, butcan also occur through autoinoculation from genital or oral lesions. Apainful cytolytic infection occurs 2 to14 days after exposure. It maturesover the subsequent 14 days, withformation of vesicles that coalesce,unroof, and form characteristic ulcers. Patients may demonstrate concomitant lymphadenitis, fever, andmalaise.The disease is self-limited, resolving over a period of 7 to 10 days. Viral shedding, and thus the ability toinfect other hosts, persists until lesion epithelialization is complete.11As the infection subsides, the virusavoids immune clearance by achieving a latent state and retreating tonervous ganglia.11 Recurrences canbe induced by psychological orphysical stress, other infections,fever, sun exposure, and other precipitants. Patients sometimes perceive a prodrome of pain, tingling,or numbness. Diagnosis is usuallymade on the basis of the history andphysical examination findings, butcan be confirmed with cultures ofthe vesicular fluid (requires 1 to 5days), Tzanck smear (less sensitivethan cultures), or a rise in serum antibody titers.The cornerstone of treatment is tonot mistake the infection for aparonychia or felon. Unnecessarydeep incision and drainage can leadto superinfection. To treat excessively painful early lesions, somehave recommended superficial unroofing of the vesicles, which hasbeen followed by some diminutionof the pain (but no change in the natural history of the infection).19 Treatment with acyclovir has been recommended to prevent recurrences,abort recurrent infections in patientswho have a prodrome, decrease theclinical course in particularly protracted cases, and induce remissionin patients with AIDS.11Flexor TenosynovitisThe flexor sheath is a mesothelialinvesting structure with a closedspace between the visceral layer adherent to the flexor tendon and theparietal layer. The sheath extendsfrom the proximal end of the A1 pulley to the level of the distal interphalangeal joint. The sheath of thethumb is contiguous with the radialbursa, and the sheath for the smallfinger is contiguous with the ulnarbursa. The radial and ulna bursaeextend proximally to the carpal tunnel. In 50% to 80% of persons, the radial and ulnar bursae communicate1,20 (Fig. 3).Pyogenic flexor tenosynovitis is abacterial infection of the flexorsheath. It usually results from penetrating trauma, although hematogenous spread is usual for gonococcalinfections. Staphylococcus aureus isthe most common causative organism. Streptococcus and Gram-negative organisms are frequently involved. In rare cases, atypicalmycobacteria are responsible for achronic indolent infection characterized by abundant tenosynovitis.9,20Kanavel described four signscharacteristic of pyogenic flexortenosynovitis: (1) flexed resting position of the involved digit, (2) ten-223
Hand InfectionsTendonsheathsMetacarpalheadsRadial bursaUlnarbursaS R M ITFlexor tendonsderness over the flexor sheath, (3)fusiform swelling, and (4) severepain on passive extension.1,21 Allsigns may not be present, especiallyearly in the course. Treatment delaycan result in tendon vascular compromise and necrosis, eventuatingin adhesions and poor gliding.Spread to contiguous deep spacescan also occur. Infection of thethumb-flexor sheath can, via contiguous spread through communication of the radial and ulnar bursae,result in infection of the small-fingersheath, and vice versa (“horseshoeabscess”). More extensive proximalspread can lead to infection ofParona’s space (the quadrilateral potential space at the wrist bordered bythe pronator quadratus, digital flexors, pollicis longus, and flexor ulnaris), sometimes resulting in acutemedian-nerve compression.20 Contiguous spread from the index-finger flexor sheath can cause infectionof the thenar space.224Fig. 3Anatomy of flexorsheath and radial and ulnarbursae. Note that the radialbursa is contiguous with theflexor pollicis tendon sheath,and the ulnar bursa is contiguous with the small-fingerflexor sheath. In 50% to 80%of persons, the ulnar and radial bursae communicate. S small finger; R ring finger; M middle finger; I index finger; T thumb.Early infections (within 24 hours)can be treated with elevation, splinting, and IV antibiotics.1 If improvement is not noted in the first 24hours, surgical treatment is necessary. Limited incisions and catheterirrigation have become popular, allowing more rapid rehabilitation andrecovery. A proximal incision ismade just proximal to the A1 pulley,near the distal palmar crease. A midlateral or volar transverse distalcounterincision is made in the distalinterphalangeal joint flexion creaseto allow through-and-through irrigation.1,20,22 A 5F pediatric feeding tubeor an angiocatheter is placed into theflexor sheath, usually in the proximalincision, and sutured in place. Caremust be taken to ensure that thecatheter is within the sheath so thatadequate irrigation of the infectioncan occur; otherwise, there is the potential for a compartment syndromein the digit due to the presence of irrigating fluid in the interstitial tissue.The sheath must be copiously irrigated. The hand is placed in a splintwith absorptive padding in thepalm. We prefer a simple closed system for irrigation that is easily understood by the floor nurses andminimizes contamination. One endof a piece of IV extension tubing isconnected to the flexor sheathcatheter. The other end is attachedto a port of a three-way stopcock. A5-mL syringe is placed in the secondport of the stopcock. An IV tube connected to a bag of normal saline is attached to the third port of the stopcock. Three times a day, 10 to 20 mLis drawn from the IV bag into the syringe by using the stopcock. Thestopcock is then directed toward thepatient, and the fluid is injectedthrough the extension tubing intothe flexor sheath. After 48 hours, thewet dressing and the irrigationcatheter are removed, and digitalmotion is started. Daily warm soaksand wet-gauze dressing changes arecontinued until the wound hashealed by secondary intention.Physical therapy and use of awhirlpool are often beneficial earlyin the mobilization process.If, at the time of initial incisionand drainage, the purulent materialin the sheath is too viscous to beevacuated by irrigation, opendrainage is necessary. It is imperative to perform this with the use of amidlateral incision instead of aBrunner-type incision. The latterhas a propensity for flap-tip necrosis, eventuating in exposed flexortendons. Once adequately debrided,the midlateral incision can be looselytacked closed over the irrigationdrainage system.Deep-Space InfectionsThe deep spaces of the hand include the dorsal subaponeurotic,thenar, midpalmar, Parona’s quadrilateral, and interdigital subfascialweb spaces. Deep-space infectionsusually occur via penetrating inocu-Journal of the American Academy of Orthopaedic Surgeons
Reid A. Abrams, MD, and Michael J. Botte, MDlation or contiguous spread; occasionally, hematogenous seeding isresponsible. Streptococcus, S aureus,and coliform organisms are the mostcommon infectious agents.1The dorsal subaponeurotic space iscontained by the extensor tendonsand fascia dorsally and the metacarpals and interosseous muscles palmarly. Infection of this space is accompanied by considerable dorsalhand swelling and may be difficult todistinguish from a subcutaneous abscess. A preferred method of incisionand drainage is with two longitudinalincisions (over the second metacarpaland over the interspace between thefourth and fifth metacarpals), followed by local wound care and earlymotion.23 Incisions directly over thedigital extensor tendons should beavoided, so as to prevent compromiseof their coverage.The thenar space is bordered dorsally by the adductor pollicis, palmarly by the index-finger flexor tendon, and ulnarly by the midpalmarseptum (which extends from themiddle-finger metacarpal to the palmar fascia).23 Radially, the thenarspace is contained by the adductorpollicis insertion into the proximalphalanx and the thenar muscle fascia (Fig. 4). Infection of this spaceusually results from penetratingtrauma or from contiguous spreadfrom index-finger flexor tenosynovitis. Infection can spread around thedistal edge of the adductor pollicisand first dorsal interosseous musclesto involve the dorsal first web, or itcan invade the interval between theadductor pollicis and first dorsal interosseous, causing a “pantaloon”effect.23 Examination reveals considerable thenar and first-web swelling.Since the volume of the thenar spaceis greatest with the thumb palmarlyabducted, this is the usual restingposture. Pain is exacerbated by passive adduction or opposition.Dorsal, palmar, and combinedincisions have been described forsurgical treatment22 (Fig. 5). Manysurgeons prefer the combined dorsal-palmar two-incision approachto ensure adequate drainage.1,20,22Another reasonable incision is onethat perpendicularly traverses thefirst-web commissure and extendsdorsally and palmarly.23 Incisionsthat parallel the first-web commissure are discouraged to avoid webcontracture. The palmar cutaneousbranch of the median nerve, the digital nerves and arterial branches tothe thumb and index finger, and thedorsal ulnar digital nerve to theMidpalmar (oblique)septumHypothenar septumThenar spaceMidpalmar spaceFig. 4 Cross section through the hand depicts the thenar and deep palmar spaces. (Adaptedwith permission from Neviaser RJ: Infections, in Green DP [ed]: Operative Hand Surgery, 3rded. New York: Churchill Livingstone, 1993, vol 1, pp 1021-1038.)Vol 4, No 4, July/August 1996ABFig. 5 Recommended incisions for drainageof thenar-space infections. Palmar (A) anddorsal (B) incisions are preferred by manysurgeons to ensure adequate decompressionof purulence, which can track dorsally fromthe thenar space to the interval between theadductor pollicis and the first dorsal interosseous muscles or to the subcutaneousarea dorsal to the first dorsal interosseousmuscle (pantaloon effect).thumb must be considered whenmaking these incisions.With adequate debridement, inthe absence of necrotic tissue,wounds can be loosely approximatedover a catheter with a similar bulkyabsorptive dressing and irrigationsetup as described for flexor tenosynovitis.1,22 Alternatively, continuousirrigation can be used.22 If there is anydoubt regarding the adequacy of thedrainage or tissue viability, thewound should be left open anddressed with loose wet-gauze packing, which must be changed daily.The deep palmar space is bordered dorsally by the middle- andring-finger metacarpals and the second and third palmar interosseousmuscles, palmarly by the flexor tendons and lumbricals, radially by themidpalmar septum, and ulnarly bythe hypothenar muscles (Fig. 4). Direct penetration or, in rare cases,contiguous spread from the flexorsheaths of the middle and ring fingers may cause infection.22,23 On presentation, the palm is markedly tender. The normal concavity of thepalm is lost, so that it instead appears flattened or convex. Dorsal225
Hand Infectionshand swelling may be so impressivethat the palmar process can be overlooked. Passive motion of the middle and ring fingers elicits pain.Transverse and oblique longitudinal incisions have been described fordrainage, as well as a distal approachin the third interspace, which allowsevacuation of the abscess through thelu
scesses, septic joints, and cellulitis. The complex anatomy of the hand also makes it susceptible to unique infections. Optimal care requires the clinician to understand this anatomy and how it influences the behavior of certain infections, so that they can be recognized and treated appropri-ately. Management usually necessi-