Transcription
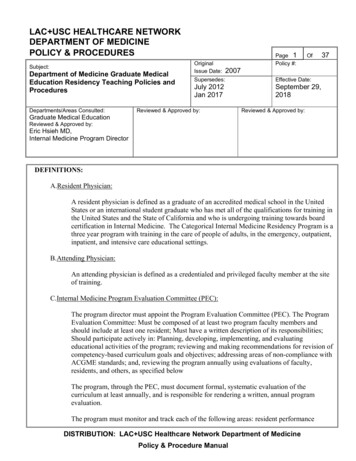
LAC USC HEALTHCARE NETWORKDEPARTMENT OF MEDICINEPOLICY & PROCEDURESSubject:Department of Medicine Graduate MedicalEducation Residency Teaching Policies andProceduresDepartments/Areas Consulted:OriginalIssue Date:Page 1Policy #:Of372007Supersedes:Effective Date:July 2012Jan 2017September 29,2018Reviewed & Approved by:Reviewed & Approved by:Graduate Medical EducationReviewed & Approved by:Eric Hsieh MD,Internal Medicine Program DirectorDEFINITIONS:A.Resident Physician:A resident physician is defined as a graduate of an accredited medical school in the UnitedStates or an international student graduate who has met all of the qualifications for training inthe United States and the State of California and who is undergoing training towards boardcertification in Internal Medicine. The Categorical Internal Medicine Residency Program is athree year program with training in the care of people of adults, in the emergency, outpatient,inpatient, and intensive care educational settings.B.Attending Physician:An attending physician is defined as a credentialed and privileged faculty member at the siteof training.C.Internal Medicine Program Evaluation Committee (PEC):The program director must appoint the Program Evaluation Committee (PEC). The ProgramEvaluation Committee: Must be composed of at least two program faculty members andshould include at least one resident; Must have a written description of its responsibilities;Should participate actively in: Planning, developing, implementing, and evaluatingeducational activities of the program; reviewing and making recommendations for revision ofcompetency-based curriculum goals and objectives; addressing areas of non-compliance withACGME standards; and, reviewing the program annually using evaluations of faculty,residents, and others, as specified belowThe program, through the PEC, must document formal, systematic evaluation of thecurriculum at least annually, and is responsible for rendering a written, annual programevaluation.The program must monitor and track each of the following areas: resident performanceDISTRIBUTION: LAC USC Healthcare Network Department of MedicinePolicy & Procedure Manual
Page2Of37Effective Date:Subject:Department of Medicine Graduate MedicalEducation Residency Teaching Policies andProceduresSeptember 2018Signatories’ Initials:Eric Hsieh, MD:(including outcome assessment of the educational effectiveness of inpatient and ambulatoryteaching); faculty development; graduate performance, including performance of programgraduates on the certification examination;program quality and progress on the previousyear’s action plan(s)The PEC must prepare a written plan of action to document initiatives to improveperformance in one or more of the areas listed above, as well as delineate how they will bemeasured and monitored.The PEC meets monthly. Standing meeting agenda items include the key components of theAccreditation Council for Graduate Medical Education (ACGME) Common ProgramRequirements (CPR) and Internal Medicine Residency Review Committee (RRC)requirements.D. Rotation:An educational unit or block.E. Core Requirements (Core):Statements that define structure, resource, or process elements essential to every graduatemedical educational program.F. Detail Requirements (Detail):Statements that describe a specific structure, resource, or process, for achieving compliancewith a Core Requirement. Programs and sponsoring institutions in substantial compliance withthe Outcome Requirements may utilize alternative or innovative approaches to meet CoreRequirements.G. Outcome Requirements (Outcome):Statements that specify expected measurable or observable attributes (knowledge, abilities,skills, or attitudes) of residents or fellows at key stages of their graduate medical education.INTRODUCTION:A. PHILOSOPHYResidency is an essential dimension of the transformation of the medical student to theindependent practitioner along the continuum of medical education. It is physically, emotionally,and intellectually demanding, and requires longitudinally-concentrated effort on the part of theresident. The specialty education of physicians to practice independently is experiential, andnecessarily occurs within the context of the health care delivery system. Developing the skills,DISTRIBUTION: LAC USC Healthcare Network Department of Medicine Policy Manual
Page3Of37Effective Date:Subject:Department of Medicine Graduate MedicalEducation Residency Teaching Policies andProceduresSeptember 2018Signatories’ Initials:Eric Hsieh, MD:knowledge, and attitudes leading to proficiency in all the domains of clinical competency requiresthe resident physician to assume personal responsibility for the care of individual patients. For theresident, the essential learning activity is interaction with patients under the guidance andsupervision of faculty members who give value, context, and meaning to those interactions. Asresidents gain experience and demonstrate growth in their ability to care for patients, they assumeroles that permit them to exercise those skills with greater independence. This concept--gradedand progressive responsibility--is one of the core tenets of education in our training program.Supervision in the setting of our training program has the goals of assuring the provision of safeand effective care to the individual patient; assuring each resident’s development of the skills,knowledge, and attitudes required to enter the unsupervised practice of medicine and pediatrics;and establishing a foundation for continued professional growth.B. POLICIES AND PROCEDURES COMPLIANCEThis policy is in accordance with:1. Manual for Graduate Medical Education Programs of Los Angeles County University ofSouthern California Medical Center, the Keck School of Medicine of the University ofSouthern California2. Accreditation Council for Graduate Medical Education (ACGME) Institutional andCommon Program Requirements (CPR)3.ACGME Residency Review Committee (RRC) Internal Medicine Requirements.C. MILESTONES AND COMPETENCY BASED EDUCATIONAL GOALS ANDOBJECTIVESThe milestones and competency based educational goals and objectives by year of training aredefined in compliance with ACGME / RRC requirements for the Internal Medicine residencyeducation program. The resident is required to achieve milestone competency in patient care,medical knowledge, practice-based learning and improvement, interpersonal andcommunication skills, professionalism and systems based practice. Goals and objectives aredefined for the overall program and each rotation.I. INSTITUTIONS:I.A. Sponsoring Institution: USC/Los Angeles County University of Southern CaliforniaMedical Center: as the sponsoring institution LAC USC Medical CenterI.A.1. Assumes ultimate responsibility for the program, as described in theInstitutional Requirements, and this responsibility extends to residentassignments at all participating sites. (Core)DISTRIBUTION: LAC USC Healthcare Network Department of Medicine Policy Manual
Page4Of37Effective Date:Subject:Department of Medicine Graduate MedicalEducation Residency Teaching Policies andProceduresSeptember 2018Signatories’ Initials:Eric Hsieh, MD:I.A.2. Ensures that the program director has sufficient protected time and financialsupport for his or her educational and administrative responsibilities to theprogram. (Core) .I.A.2b-c. Ensures that the sufficient number of associate program directors (APD) areprovided based upon the number of residents and ensures that each APD as the salary support for20 hours per week of work.I.A.2d. Ensures that the sufficient number of core faculty are providedI.A.2.e – Ensure that the appropriate number of program administrators are provided for theoperation of the programI.A.2 f – Ensures that the residents have access to simulations labs (Surgical Skills Center andFresh Tissue Lab)I.A.2g – Ensures access to an Electronic Medical Record (Orchid)I.A.2.h) provide the resources to ensure the implementation of the following:I.A.2.h).(1) inpatient and outpatient systems to prevent residents from performing routine clericalfunctions, such as scheduling tests and appointments, and retrieving records and letters; (Core)I.A.2.h).(2) residents’ service responsibilities must be limited to patients for whom the teachingservice has diagnostic and therapeutic responsibility. (N.B.: Teaching Service is defined as thosepatients for whom internal medicine residents [PGY 1, 2, or 3] routinely provide care); (Core)I.A.2.h).(3) residents must not be assigned more than two months of night float during any year oftraining, or more than four months of night float over the three years of residency training.Residents must not be assigned to more than one month of consecutive night float rotation; (Core)I.A.2.h).(4) residents should not be required to relate to an excessive number of physicians ofrecord; (Core)I.A.2.h).(5) residents from other specialties must not supervise internal medicine residents on anyinternal medicine inpatient rotation; and, (Core)I.A.2.h).(6) on inpatient rotations: (Core)I.A.2.h).(6).(a) a first-year resident must not be assigned more than five new patients per admittingday; an additional two patients may be assigned if they are in-house transfers from the medicalservices; (Core)I.A.2.h).(6).(b) a first-year resident must not be assigned more than eight new patients in a 48-hourperiod; (Core)DISTRIBUTION: LAC USC Healthcare Network Department of Medicine Policy Manual
Page5Of37Effective Date:Subject:Department of Medicine Graduate MedicalEducation Residency Teaching Policies andProceduresSeptember 2018Signatories’ Initials:Eric Hsieh, MD:I.A.2.h).(6).(c) a first-year resident must not be responsible for the ongoing care of more than 10patients; (Core)I.A.2.h).(6).(d) when supervising more than one first-year resident, the supervising resident mustnot be responsible for the supervision or admission of more than 10 new patients and four transferpatients per admitting day or more than 16 new patients in a 48-hour period; (Core)I.A.2.h).(6).(e) when supervising one first-year resident, the supervising resident must not beresponsible for the ongoing care of more than 14 patients; (Core)I.A.2.h).(6).(f) when supervising more than one first-year resident, the supervising resident mustnot be responsible for the ongoing care of more than 20 patients; (Core)I.A.2.h).(6).(g) residents must write all orders for patients under their care, with appropriatesupervision by the attending physician. In those unusual circumstances when an attendingphysician or subspecialty resident writes an order on a resident’s patient, the attending orsubspecialty resident must communicate his or her action to the resident in a timely manner;(Core)I.A.2.h).(6).(h) second- or third-year internal medicine residents or other appropriate supervisoryphysicians (e.g., subspecialty residents or attendings) with documented experience appropriate tothe acuity, complexity, and severity of patient illness must be available at all times on site tosupervise first-year residents; (Core)I.A.2.h).(6).(i) each physician of record has the responsibility to make management rounds on hisor her patients and to communicate effectively with the residents participating in the care of thesepatients at a frequency appropriate to the changing care needs of the patients; (Core)I.A.2.h).(6).(j) total required transplant rotations in dedicated units should not exceed one monthin three years. (Detail)I.B. Participating Sites:I.B.1. Keck Hospital of the University of Southern California (USC) where residentsparticipate in rotations on Keck Medicine, Keck Cardiology, Keck Liver, or Keck NightFloat. A program letter of agreement exists between the Medicine Program and KeckHospital of USC for this rotation.I.B.2. Norris Cancer Center where residents participate in one rotation of training inthree years on either the Norris Hematology or Oncology Rotation. A programletter of agreement exists between the Medicine Program and Norris CancerCenter for this rotation.DISTRIBUTION: LAC USC Healthcare Network Department of Medicine Policy Manual
Page6Of37Effective Date:Subject:Department of Medicine Graduate MedicalEducation Residency Teaching Policies andProceduresSeptember 2018Signatories’ Initials:Eric Hsieh, MD:I.B.3 VA Greater Los Angeles where residents participate in one week rotation in ComplementaryMedicine. A program letter of agreement exists between the Medicine Program and the VAGreater Los Angeles.I.C. The Program Letters of AgreementI.C.1. identify the faculty who assume both educational and supervisoryresponsibilities for residents at the participating site; (Detail)I.C.2. specify the responsibilities of the faculty for teaching, supervision, and formalevaluation of residents, as specified later in this document; (Detail)I.C.3. specify the duration and content of the educational experience; and, (Detail)I.C.4. state the policies and procedures that will govern resident education during theassignment. (Detail)I.C.5. The program director will submit any additions or deletions of participating sitesroutinely providing an educational experience, required for all residents, of onemonth full time equivalent (FTE) or more through the Accreditation Council forGraduate Medical Education (ACGME) Accreditation Data System (ADS).(Core)II. Program Personnel and ResourcesII.A. Program DirectorII.A.1. There is a single program director with authority and accountability forthe operation of the program. A request for approval by the sponsoring institution’sGMEC will be made before a change in program director. (Core)II.A.1.a) Will a change in program director approved by the institutionalGMEC occur the program director will submit this change to the ACGMEvia the ADS. (Core)II.A.2. The program director will continue in his or her position for a length oftime adequate to maintain continuity of leadership and program stability.(Detail)II.A.3. Qualifications of the program director includes:II.A.3.a) requisite specialty expertise and documented educational andadministrative experience acceptable to the ReviewCommittee; (Core)DISTRIBUTION: LAC USC Healthcare Network Department of Medicine Policy Manual
Page7Of37Effective Date:Subject:Department of Medicine Graduate MedicalEducation Residency Teaching Policies andProceduresSeptember 2018Signatories’ Initials:Eric Hsieh, MD:II.A.3.b) The program director will be certified by the AmericanBoard of Internal or possess qualifications that are judged to beacceptable by the Review Committee. (Core)II.A.3.c) current medical licensure and appropriate medical staffappointment. (Core)II.A.4. The program director will administer and maintain an educationalenvironment conducive to educating the residents in each of theACGME competency areas. (Core) The program director will:II.A.4.a) oversee and ensure the quality of didactic and clinicaleducation in all sites that participate in the program; (Core)II.A.4.b) approve a local director at each participating site who isaccountable for resident education; (Core)II.A.4.c) approve the selection of program faculty as appropriate;(Core)II.A.4.d) evaluate program faculty; (Core)II.A.4.e) approve the continued participation of program faculty basedon evaluation; (Core)II.A.4.f) monitor resident supervision at all participating sites; (Core)II.A.4.g) prepare and submit all information required and requested bythe ACGME. (Core)II.A.4.g).(1) This includes but is not limited to the programapplication forms and annual program updates tothe ADS, and ensure that the information submittedis accurate and complete. (Core)II.A.4.h) ensure compliance with grievance and due processprocedures as set forth in the Institutional Requirements andimplemented by the sponsoring institution; (Detail)II.A.4.i) provide verification of residency education for all residents,including those who leave the program prior to completion;(Detail)DISTRIBUTION: LAC USC Healthcare Network Department of Medicine Policy Manual
Page8Of37Effective Date:Subject:Department of Medicine Graduate MedicalEducation Residency Teaching Policies andProceduresSeptember 2018Signatories’ Initials:Eric Hsieh, MD:II.A.4.j) implement policies and procedures consistent with theinstitutional and program requirements for resident dutyhours and the working environment, including moonlighting,(Core) and, to that end, will:II.A.4.j).(1) distribute these policies and procedures to theresidents and faculty; (Detail)II.A.4.j).(2) monitor resident duty hours, according tosponsoring institutional policies, with a frequencysufficient to ensure compliance with ACGMErequirements; (Core)II.A.4.j).(3) adjust schedules as necessary to mitigateexcessive service demands and/or fatigue; and,(Detail)II.A.4.j).(4) if applicable, monitor the demands of at-homecall and adjust schedules as necessary to mitigateexcessive service demands and/or fatigue. (Detail)II.A.4.k) monitor the need for and ensure the provision ofback up support systems when patient care responsibilitiesare unusually difficult or prolonged; (Detail)II.A.4.l) comply with the sponsoring institution’s writtenpolicies and procedures, including those specified in theInstitutional Requirements, for selection, evaluation andpromotion of residents, disciplinary action, and supervisionof residents; (Detail)II.A.4.m) be familiar with and comply with ACGME and ReviewCommittee policies and procedures as outlined in theACGME Manual of Policies and Procedures; (Detail)II.A.4.n) obtain review and approval of the sponsoring institution’sGMEC/DIO before submitting information or requests to theACGME, including: (Core)II.A.4.n).(1) all applications for ACGME accreditation of newprograms; (Detail)II.A.4.n).(2) changes in resident complement; (Detail)II.A.4.n).(3) major changes in program structure or length ofDISTRIBUTION: LAC USC Healthcare Network Department of Medicine Policy Manual
Page9Of37Effective Date:Subject:Department of Medicine Graduate MedicalEducation Residency Teaching Policies andProceduresSeptember 2018Signatories’ Initials:Eric Hsieh, MD:training; (Detail)II.A.4.n).(4) progress reports requested by the ReviewCommittee; (Detail)II.A.4.n).(5) requests for increases or any change to residentduty hours; (Detail)II.A.4.n).(6) voluntary withdrawals of ACGME-accreditedprograms; (Detail)II.A.4.n).(7) requests for appeal of an adverse action; and,(Detail)II.A.4.n).(8) appeal presentations to a Board of Appeal or theACGME. (Detail)II.A.4.o) obtain DIO review and co-signature on all program applicationforms, as well as any correspondence or documentsubmitted to the ACGME that addresses: (Detail)II.A.4.o).(1) program citations, and/or, (Detail)II.A.4.o).(2) request for changes in the program that wouldhave significant impact, including financial, on the programor institution. (Detail)II.A.4.p) monitor resident stress, including mental or emotional conditions inhibiting performanceor learning, and drug- or alcohol-related dysfunction. (Core)II.A.4.p).(1) Both the program director and faculty should be sensitive to the need for timelyprovision of confidential counseling and psychological support services to residents. (Detail)II.A.4.p).(2) Situations that demand excessive service or that consistently produce undesirablestress on residents must be evaluated and modified; (Detail)II.A.4.q) dedicate no less than 50% (at least 20 hours per week) of his or her professional effort tothe administrative and educational activities of the internal medicine educational program andreceive institutional support for this time; (Detail)II.A.4.r) be available and accessible to residents at the primary teaching site(s); (Detail) II.A.4.s)oversee development of an effective resident advising program; (Detail)DISTRIBUTION: LAC USC Healthcare Network Department of Medicine Policy Manual
Page10Of37Effective Date:Subject:Department of Medicine Graduate MedicalEducation Residency Teaching Policies andProceduresSeptember 2018Signatories’ Initials:Eric Hsieh, MD:II.A.4.t) supervise any internal medicine subspecialty training programs sponsored by theinstitution and linked to their core program to ensure compliance with the ACGME accreditationstandards; (Core)II.A.4.u) have supervisory authority over all educational tracks in the internal medicine residencyprogram; (Detail)II.A.4.v) conduct the internal medicine component of special educational tracks under the auspicesof the Department of Internal Medicine; (Detail)II.A.4.w) ensure that the residency does not place excessive reliance on residents for service asopposed to education; (Core)II.A.4.x) participate in academic societies and in educational programs designed to enhance his orher educational and administrative skills. (Detail)II.B. FacultyII.B.1. There will be a sufficient number of faculty at each participating sitewith documented qualifications to instruct and supervise all residentsat that location. (Core) The faculty will:II.B.1.a) devote sufficient time to the educational program to fulfill theirsupervisory and teaching responsibilities; and todemonstrate a strong interest in the education of residents;and, (Core)II.B.1.b) administer and maintain an educational environmentconducive to educating residents in each of the ACGMEcompetency areas. (Core)II.B.2. The physician faculty will have current certification by the American Board ofMedicine or possess qualifications judged acceptable to the ReviewCommittee. (Core)II.B.3. The physician faculty will possess current medical licensure and appropriatemedical staff appointment. (Core)II.B.4. The nonphysician faculty will have appropriate qualifications in their field andhold appropriate institutional appointments. (Core)II.B.5. The faculty will establish and maintain an environment of inquiry and scholarshipwith an active research component. (Core)II.B.5.a) The faculty will regularly participate in organized clinical discussions, rounds,DISTRIBUTION: LAC USC Healthcare Network Department of Medicine Policy Manual
Page11Of37Effective Date:Subject:Department of Medicine Graduate MedicalEducation Residency Teaching Policies andProceduresSeptember 2018Signatories’ Initials:Eric Hsieh, MD:journal clubs, and conferences. (Detail)II.B.5.b) Some members of the faculty will also demonstrate scholarship by one ormore of the following:II.B.5.b).(1) peer-reviewed funding; (Detail)II.B.5.b).(2) publication of original research or review articles in peerreviewed journals, or chapters in textbooks; (Detail)II.B.5.b).(3) publication or presentation of case reports or clinical series atlocal, regional, or national professional and scientific societymeetings; or, (Detail)II.B.5.b).(4) participation in national committees or educationalorganizations. (Detail)II.B.5.c) Faculty will encourage and support residents in scholarly activities. (Core)II.C. Other Program Personnel: The institution and the program will jointly ensure theavailability of all necessary professional, technical, and clerical personnel for theeffective administration of the program. (Core)II.C.1. Associate Program DirectorsAssociate program directors (APDs) are faculty who assist the program director in theadministrative and clinical oversight of the educational program.II.C.1.a) Qualifications of the associate program directors are as follows:II.C.1.a).(1) must be clinicians with broad knowledge of, experience with, and commitment tointernal medicine as a discipline, patient centered care, and to the generalist training ofresidents, and (DetailII.C.1.a).(2) must hold current certification from the American Board of Internal Medicine(ABIM) in either internal medicine or a subspecialty. (Core)II.C.1.b) Responsibilities for associate program directors are as follows:II.C.1.b).(1) must dedicate an average of at least 20 hours per week to the administrative andeducational aspects of the educational program, as delegated by the program director, andreceive institutional support for this time; (Core)II.C.1.b).(2) must report directly to the program director; and, (Detail)DISTRIBUTION: LAC USC Healthcare Network Department of Medicine Policy Manual
Page12Of37Effective Date:Subject:Department of Medicine Graduate MedicalEducation Residency Teaching Policies andProceduresSeptember 2018Signatories’ Initials:Eric Hsieh, MD:II.C.1.b).(3) must participate in academic societies and in educational programs designed toenhance their educational and administrative skills. (Detail)II.C.2. Subspecialty Education CoordinatorsIn conjunction with division chiefs, the program director must identify a qualified individual,the Subspecialty Education Coordinator, in each of the following subspecialties of internalmedicine: cardiology, critical care, endocrinology, hematology, gastroenterology, geriatricmedicine, infectious diseases, nephrology, oncology, pulmonary disease, and rheumatology.(Core)II.C.2.a) The Subspecialty Education Coordinator must be:II.C.2.a).(1) currently certified in the subspecialty by the ABIM, and (Core)II.C.2.a).(2) accountable to the program director for coordination of the residents’subspecialty educational experiences in order to accomplish the goals and objectives in thesubspecialty. (N.B.: Core Faculty may also serve as Subspecialty Education Coordinators.)(Detail)II.C.3. Core Faculty The residency program must include institutionally based core faculty inaddition to the program director and associate program directors. The core faculty are theexpert competency evaluators who work closely with the program director and associateprogram directors, who assist in developing and implementing the evaluation system, andwho teach and advise residents. (Core)The core faculty must:II.C.3.a) be ABIM-certified internists who are clinically active, either in direct patient care orin the supervision of patient care; (Core)II.C.3.b) dedicate an average of at least 15 hours per individual per week throughout the yearto residency training; (Core)II.C.3.c) be specifically trained in the evaluation and assessment of the ACGMEcompetencies; (Detail)II.C.3.d) spend significant time in the evaluation of residents including the direct observationof residents with patients; and, (Detail)II.C.3.e) advise residents with respect to their career and educational goals. (Detail)DISTRIBUTION: LAC USC Healthcare Network Department of Medicine Policy Manual
Page13Of37Effective Date:Subject:Department of Medicine Graduate MedicalEducation Residency Teaching Policies andProceduresSeptember 2018Signatories’ Initials:Eric Hsieh, MD:II.D. Resources: The institution and the program will jointly ensure the availability of adequateresources for resident education, as defined in the specialty program requirements. (Core)II.D.5. Patient PopulationII.D.5.a) The patient population must have a variety of clinical problems and stages of disease.(Core)II.D.5.b) There must be patients of both sexes, with a broad age range, including geriatric patients.(Core)II.D.6. There must be services available from other health care professionals such as nurses, socialworkers, case managers, language interpreters, dieticians, etc. to assist with patient care. (Detail)II.D.7. Consultations from other clinical services must be available in a timely manner in all caresettings where the residents work. All consultations should be performed by or under thesupervision of a qualified specialist.II.E. Medical Information Access: Residents will have ready access to specialty-specific andother appropriate reference material in print or electronic format. Electronic medical literaturedatabases with search capabilities will be available. (Detail)III. Resident AppointmentsIII.A. Eligibility Criteria: The program director will comply with the criteria for residenteligibility as specified in the Institutional Requirements. (Core)III.A.1. All prerequisite post-graduate clinical education required forinitial entry or transfer into ACGME-accredited residency programs will becompleted in ACGME-accredited residency programs, or in Royal College ofPhysicians and Surgeons of Canada (RCPSC)-accredited or College ofFamily Physicians of Canada (CFPC)-accredited residency programs locatedin Canada. Residency programs will receive verification of each applicant’slevel of competency in the required clinical field using ACGME orCanMEDS Milestones assessments from the prior training program. (Core)III.A.2. A physician who has completed a residency program thatwas not accredited by ACGME, RCPSC, or CFPC may enteran ACGME-accredited residency program in the same specialty at the PGY-1level and, at the discretion of the program director at the ACGME-accreditedprogram may be advanced to the PGY-2 level based on ACGME Milestonesassessments at the ACGME-accredited program. This provision applies onlyto entry into residency in those specialties for which an initial clinical year isnot required for entry. (Core)DISTRIBUTION: LAC USC Healthcare Network Department of Medicine Policy Manual
Page14Of37Effective Date:Subject:Department of Medicine Graduate MedicalEducation Residency Teaching Policies andProceduresSeptember 2018Signatories’ Initials:Eric Hsieh, MD:III.A.3. A Review Committee may grant the exception to the eligibilityrequirements specified in Section III.A.2.b) for residencyprograms that require completion of a prerequisite residencyprogram prior to admission. (Core)III.A.4. Review Committees will grant no other exceptions to theseeligibility requirements for residency education. (Core)III.B. Number of Residents: The program’s educational resources will be adequate tosupport the number of residents appointed to the program. (Core)III.B.1. The program director may not appoint more residents than approved bythe Review Committee, unless otherwise stated in the specialtyspecific requirements. (Core)III.C. Resident TransfersIII.C.1. Before accepting a resident who is transferring from anotherprogram, the program
The PEC must prepare a written plan of action to document initiatives to improve performance in one or more of the areas listed above, as well as delineate how they will be . USC/Los Angeles County University of Southern California Medical Center: as the sponsoring institution LAC USC Medical Center I.A.1. Assumes ultimate responsibility .