Transcription
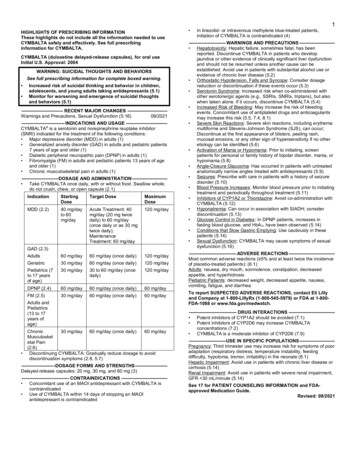
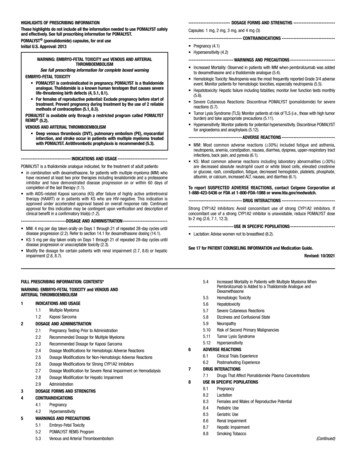
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to useLANTUS safely and effectively. See full prescribing information forLANTUS.LANTUS (insulin glargine injection) for subcutaneous injectionInitial U.S. Approval: 2000----------------------------RECENT MAJOR CHANGES-------------------------Dosage and Administration (2.1)11/2019Warnings and Precautions S AND USAGE--------------------------LANTUS is a long-acting human insulin analog indicated to improveglycemic control in adults and pediatric patients with type 1 diabetes mellitusand in adults with type 2 diabetes mellitus. (1)Limitations of UseNot recommended for treating diabetic ketoacidosis. (1)----------------------DOSAGE AND ADMINISTRATION---------------------- Individualize dosage based on metabolic needs, blood glucose monitoring,glycemic control, type of diabetes prior insulin use. (2.1, 2.3, 2.4) Administer subcutaneously into the abdominal area, thigh, or deltoid oncedaily at any time of day, but at the same time every day. (2.1) Do not dilute or mix with any other insulin or solution. (2.1) Rotate injection sites to reduce risk of lipodystrophy and localizedcutaneous amyloidosis. (2.2) Closely monitor glucose when changing to LANTUS and during initialweeks thereafter. (2.4)---------------------DOSAGE FORMS AND STRENGTHS---------------------Injection: 100 units/mL (U-100) available as: 10 mL multiple-dose vial (3) 3 mL single-patient-use SoloStar prefilled pen ------------------------------ During episodes of hypoglycemia (4) Hypersensitivity to LANTUS or one of its excipients (4) Hyperglycemia or hypoglycemia with changes in insulin regimen: Makechanges to a patient’s insulin regimen (e.g., insulin strength, manufacturer,type, injection site or method of administration) under close medicalsupervision with increased frequency of blood glucose monitoring. (5.2) Hypoglycemia: May be life-threatening. Increase frequency of glucosemonitoring with changes to: insulin dosage, coadministered glucoselowering medications, meal pattern, physical activity; and in patients withrenal or hepatic impairment and hypoglycemia unawareness. (5.3, 6.1) Medication Errors: Accidental mix-ups between insulin products canoccur. Instruct patients to check insulin labels before injection. (5.4, 6.3) Hypersensitivity reactions: Severe, life-threatening, generalized allergy,including anaphylaxis, can occur. Discontinue LANTUS. Monitor and treatif indicated. (5.5, 6.1) Hypokalemia: May be life-threatening. Monitor potassium levels inpatients at risk of hypokalemia and treat if indicated. (5.6) Fluid retention and heart failure with concomitant use ofthiazolidinediones (TZDs): Observe for signs and symptoms of heartfailure; consider dosage reduction or discontinuation of TZD if heart failureoccurs. (5.7)------------------------------ADVERSE REACTIONS------------------------------Adverse reactions commonly associated with LANTUS includehypoglycemia, allergic reactions, injection site reactions, lipodystrophy,pruritus, rash, edema and weight gain. (6.1)To report SUSPECTED ADVERSE REACTIONS, contact sanofi-aventisat 1-800-633-1610 or FDA at 1-800-FDA-1088 or -DRUG INTERACTIONS------------------------------ Drugs that affect glucose metabolism: Adjustment of insulin dosage maybe needed; closely monitor of blood glucose. (7) Antiadrenergic Drugs (e.g., beta-blockers, clonidine, guanethidine, andreserpine): Signs and symptoms of hypoglycemia may be reduced orabsent. (7)See 17 for PATIENT COUNSELING INFORMATION and FDAapproved patient labeling.-----------------------WARNINGS AND PRECAUTIONS----------------------- Never share a LANTUS SoloStar prefilled pen between patients, even ifthe needle is changed. (5.1)FULL PRESCRIBING INFORMATION: CONTENTS*1 INDICATIONS AND USAGE2 DOSAGE AND ADMINISTRATION2.1 Important Administration Instructions2.2 General Dosing Instructions2.3 Initiation of LANTUS Therapy2.4 Changing to LANTUS from Other Insulin Therapies3 DOSAGE FORMS AND STRENGTHS4 CONTRAINDICATIONS5 WARNINGS AND PRECAUTIONS5.1 Never Share a LANTUS SoloStar Prefilled Pen, Syringe, or NeedleBetween Patients5.2 Hyperglycemia or Hypoglycemia with Changes in Insulin Regimen5.3 Hypoglycemia5.4 Medication Errors5.5 Hypersensitivity and Allergic Reactions5.6 Hypokalemia5.7 Fluid Retention and Heart Failure with Concomitant Use of PPARgamma Agonists6 ADVERSE REACTIONS6.1 Clinical Trials Experience6.2 Immunogenicity6.3 Postmarketing Experience7 DRUG INTERACTIONS8 USE IN SPECIFIC POPULATIONS8.1 Pregnancy8.2 LactationRevised: 11/2019101112131416178.4 Pediatric Use8.5 Geriatric Use8.6 Hepatic Impairment8.7 Renal Impairment8.8 ObesityOVERDOSAGEDESCRIPTIONCLINICAL PHARMACOLOGY12.1 Mechanism of Action12.2 Pharmacodynamics12.3 PharmacokineticsNONCLINICAL TOXICOLOGY13.1 Carcinogenesis, Mutagenesis, Impairment of FertilityCLINICAL STUDIES14.1 Overview of Clinical Studies14.2 Clinical Studies in Adult and Pediatric Patients with Type 1Diabetes14.3 Clinical Studies in Adults with Type 2 DiabetesHOW SUPPLIED/STORAGE AND HANDLING16.1 How Supplied16.2 StoragePATIENT COUNSELING INFORMATION*Sections or subsections omitted from the full prescribing information are notlisted.1Reference ID: 4519571
FULL PRESCRIBING INFORMATION1INDICATIONS AND USAGELANTUS is indicated to improve glycemic control in adults and pediatric patients with type 1diabetes mellitus and in adults with type 2 diabetes mellitus.Limitations of UseLANTUS is not recommended for the treatment of diabetic ketoacidosis.2DOSAGE AND ADMINISTRATION2.1Important Administration Instructions Administer LANTUS subcutaneously once daily at any time of day but at the same timeevery day.Prior to initiation of LANTUS, train patients on proper use and injection technique.Patient should follow the Instructions for Use to correctly administer LANTUS.Administer LANTUS subcutaneously into the abdominal area, thigh, or deltoid, and rotateinjection sites within the same region from one injection to the next to reduce the risk oflipodystrophy and localized cutaneous amyloidosis. Do not inject into areas of lipodystrophyor localized cutaneous amyloidosis [see Warnings and Precautions (5.2), Adverse Reactions(6)].During changes to a patient’s insulin regimen, increase the frequency of blood glucosemonitoring [see Warnings and Precautions (5.2)].Visually inspect LANTUS vials and SoloStar prefilled pens for particulate matter anddiscoloration prior to administration. Only use if the solution is clear and colorless with novisible particles.The LANTUS SoloStar prefilled pen dials in 1-unit increments.Use LANTUS SoloStar prefilled pen with caution in patients with visual impairment whomay rely on audible clicks to dial their dose.Refrigerate unused (unopened) LANTUS vials and SoloStar prefilled pens.Do not administer intravenously or via an insulin pump.Do not dilute or mix LANTUS with any other insulin or solution.The SoloStar prefilled pen is for single patient use only [see Warnings and Precautions(5.1)].2.2 General Dosing InstructionsIndividualize and adjust the dosage of LANTUS based on the individual’s metabolic needs,blood glucose monitoring results and glycemic control goal.Dosage adjustments may be needed with changes in physical activity, changes in mealpatterns (i.e., macronutrient content or timing of food intake), during acute illness, or changesin renal or hepatic function. Dosage adjustments should only be made under medicalsupervision with appropriate glucose monitoring [see Warnings and Precautions (5.2)].2.3Initiation of LANTUS TherapyType 1 Diabetes2Reference ID: 4519571
In patients with type 1 diabetes, LANTUS must be used concomitantly with short-actinginsulin. The recommended starting dose of LANTUS in patients with type 1 diabetes shouldbe approximately one-third of the total daily insulin requirements. Short-acting, premealinsulin should be used to satisfy the remainder of the daily insulin requirements.Type 2 Diabetes The recommended starting dose of LANTUS in patients with type 2 diabetes who are notcurrently treated with insulin is 0.2 units/kg or up to 10 units once daily. One may need toadjust the amount and timing of short- or rapid-acting insulins and dosages of any oralantidiabetic drugs.2.4 Changing to LANTUS from Other Insulin TherapiesIf changing patients from once-daily TOUJEO (insulin glargine) 300 units/mL to once-dailyLANTUS, the recommended initial LANTUS dose is 80% of the TOUJEO dose that is beingdiscontinued. This dose reduction will lower the likelihood of hypoglycemia [see Warningsand Precautions (5.3)].If changing from a treatment regimen with an intermediate or long-acting insulin to aregimen with LANTUS, a change in the dose of the basal insulin may be required and theamount and timing of the shorter-acting insulins and doses of any oral antidiabetic drugs mayneed to be adjusted.If changing patients from once-daily NPH insulin to once-daily LANTUS, the recommendedinitial LANTUS dose is the same as the dose of NPH that is being discontinued.If changing patients from twice-daily NPH insulin to once-daily LANTUS, the recommendedinitial LANTUS dosage is 80% of the total NPH dose that is being discontinued. This dosagereduction will lower the likelihood of hypoglycemia [see Warnings and Precautions (5.3)].3DOSAGE FORMS AND STRENGTHSInjection: 100 units per mL (U-100) available as: 410 mL multiple-dose vial3 mL single-patient-use SoloStar prefilled penCONTRAINDICATIONSLANTUS is contraindicated: during episodes of hypoglycemia [see Warnings and Precautions (5.3)]in patients with hypersensitivity to LANTUS or one of its excipients [see Warnings andPrecautions (5.5)]5WARNINGS AND PRECAUTIONS5.1Never Share a LANTUS SoloStar Prefilled Pen, Syringe, or Needle BetweenPatientsLANTUS SoloStar prefilled pens must never be shared between patients, even if the needle ischanged. Patients using LANTUS vials must never re-use or share needles or syringes withanother person. Sharing poses a risk for transmission of blood-borne pathogens.3Reference ID: 4519571
5.2Hyperglycemia or Hypoglycemia with Changes in Insulin RegimenChanges in an insulin regimen (e.g., insulin strength, manufacturer, type, injection site or methodof administration) may affect glycemic control and predispose to hypoglycemia [see Warningsand Precautions (5.3)] or hyperglycemia. Repeated insulin injections into areas of lipodystrophyor localized cutaneous amyloidosis have been reported to result in hyperglycemia; and a suddenchange in the injection site (to unaffected area) has been reported to result in hypoglycemia [seeAdverse Reactions (6.)].Make any changes to a patient’s insulin regimen under close medical supervision with increasedfrequency of blood glucose monitoring. Advise patients who have repeatedly injected into areasof lipodystrophy or localized cutaneous amyloidosis to change the injection site to unaffectedareas and closely monitor for hypoglycemia. For patients with type 2 diabetes, dosageadjustments of concomitant oral and antidiabetic products may be needed.5.3HypoglycemiaHypoglycemia is the most common adverse reaction associated with insulin, includingLANTUS. Severe hypoglycemia can cause seizures, may be life-threatening or cause death.Hypoglycemia can impair concentration ability and reaction time; this may place an individualand others at risk in situations where these abilities are important (e.g., driving or operating othermachinery).Hypoglycemia can happen suddenly and symptoms may differ in each individual and changeover time in the same individual. Symptomatic awareness of hypoglycemia may be lesspronounced in patients with longstanding diabetes, in patients with diabetic nerve disease, inpatients using medications that block the sympathetic nervous system (e.g., beta-blockers) [seeDrug Interactions (7)], or in patients who experience recurrent hypoglycemia.Risk Factors for HypoglycemiaThe risk of hypoglycemia after an injection is related to the duration of action of the insulin and,in general, is highest when the glucose lowering effect of the insulin is maximal. As with allinsulin preparations, the glucose lowering effect time course of LANTUS may vary in differentindividuals or at different times in the same individual and depends on many conditions,including the area of injection as well as the injection site blood supply and temperature [seeClinical Pharmacology (12.2)]. Other factors which may increase the risk of hypoglycemiainclude changes in meal pattern (e.g., macronutrient content or timing of meals), changes in levelof physical activity, or changes to coadministered medication [see Drug Interactions (7)].Patients with renal or hepatic impairment may be at higher risk of hypoglycemia [see Use inSpecific Populations (8.6, 8.7)].Risk Mitigation Strategies for HypoglycemiaPatients and caregivers must be educated to recognize and manage hypoglycemia. Selfmonitoring of blood glucose plays an essential role in the prevention and management ofhypoglycemia. In patients at higher risk for hypoglycemia and patients who have reducedsymptomatic awareness of hypoglycemia, increased frequency of blood glucose monitoring isrecommended.The long-acting effect of LANTUS may delay recovery from hypoglycemia.5.4Medication Errors4Reference ID: 4519571
Accidental mix-ups among insulin products, particularly between long-acting insulins and rapidacting insulins, have been reported. To avoid medication errors between LANTUS and otherinsulins, instruct patients to always check the insulin label before each injection [see AdverseReactions (6.3)].5.5Hypersensitivity and Allergic ReactionsSevere, life-threatening, generalized allergy, including anaphylaxis, can occur with insulinproducts, including LANTUS. If hypersensitivity reactions occur, discontinue LANTUS; treatper standard of care and monitor until symptoms and signs resolve [see Adverse Reactions (6.1)].LANTUS is contraindicated in patients who have had hypersensitivity reactions to insulinglargine or one of the excipients [see Contraindications (4)].5.6HypokalemiaAll insulin products, including LANTUS, cause a shift in potassium from the extracellular tointracellular space, possibly leading to hypokalemia. Untreated hypokalemia may causerespiratory paralysis, ventricular arrhythmia, and death. Monitor potassium levels in patients atrisk for hypokalemia, if indicated (e.g., patients using potassium-lowering medications, patientstaking medications sensitive to serum potassium concentrations).5.7Fluid Retention and Heart Failure with Concomitant Use of PPAR-gammaAgonistsThiazolidinediones (TZDs), which are peroxisome proliferator-activated receptor (PPAR)gamma agonists, can cause dose-related fluid retention, particularly when used in combinationwith insulin. Fluid retention may lead to or exacerbate heart failure. Patients treated with insulin,including LANTUS, and a PPAR-gamma agonist should be observed for signs and symptoms ofheart failure. If heart failure develops, it should be managed according to current standards ofcare, and discontinuation or dose reduction of the PPAR-gamma agonist must be considered.6ADVERSE REACTIONSThe following adverse reactions are discussed elsewhere: 6.1Hypoglycemia [see Warnings and Precautions (5.3)]Hypersensitivity and allergic reactions [see Warnings and Precautions (5.5)]Hypokalemia [see Warnings and Precautions (5.6)]Clinical Trials ExperienceBecause clinical trials are conducted under widely varying conditions, adverse reaction ratesobserved in clinical trials of a drug cannot be directly compared to rates in the clinical trial ofanother drug and may not reflect the rates observed in practice.The data in Table 1 reflect the exposure of 2327 patients with type 1 diabetes to LANTUS orNPH. The type 1 diabetes population had the following characteristics: Mean age was 38.5 years.Fifty four percent were male, 96.9% were Caucasian, 1.8% were Black or African American and2.7% were Hispanic. The mean BMI was 25.1 kg/m2.The data in Table 2 reflect the exposure of 1563 patients with type 2 diabetes to LANTUS orNPH. The type 2 diabetes population had the following characteristics: Mean age was 59.3 years.5Reference ID: 4519571
Fifty eight percent were male, 86.7% were Caucasian, 7.8% were Black or African Americanand 9% were Hispanic. The mean BMI was 29.2 kg/m2.The frequencies of adverse events during LANTUS clinical trials in patients with type 1 diabetesmellitus and type 2 diabetes mellitus are listed in the tables below.Table 1: Adverse Events in Pooled Clinical Trials up to 28 Weeks Duration in Adults withType 1 Diabetes (adverse events with frequency 5%)Upper respiratory tract infectionInfection*Accidental injuryHeadache* Body system not specifiedLANTUS, %(n 1257)NPH, %(n 1070)22.49.45.75.523.110.36.44.7Table 2: Adverse Events in Pooled Clinical Trials up to 1 Year Duration in Adults withType 2 Diabetes (adverse events with frequency 5%)Upper respiratory tract infectionInfection*Retinal vascular disorder* Body system not specifiedLANTUS, %(n 849)11.410.45.8NPH, %(n 714)13.311.67.4Table 3: Adverse Events in a 5 Year Trial of Adults with Type 2 Diabetes (adverse eventswith frequency 10%)Upper respiratory tract infectionEdema onchitisArthralgiaPain in extremityBack painCoughUrinary tract infectionDiarrheaDepressionHeadacheLANTUS, %(n .710.710.510.3NPH, %(n 110.39.79.36Reference ID: 4519571
Table 4: Adverse Events in a 28-Week Clinical Trial of Children and Adolescents withType 1 Diabetes (adverse events with frequency 5%)LANTUS, %(n 174)13.813.87.55.2Infection*Upper respiratory tract infectionPharyngitisRhinitis* Body system not specifiedNPH, %(n 175)17.716.08.65.1Severe HypoglycemiaHypoglycemia is the most commonly observed adverse reaction in patients using insulin,including LANTUS [see Warnings and Precautions (5.3)]. Tables 5, and 6, and 7 summarize theincidence of severe hypoglycemia in the LANTUS individual clinical trials. Severe symptomatichypoglycemia was defined as an event with symptoms consistent with hypoglycemia requiringthe assistance of another person and associated with either a blood glucose below 50 mg/dL ( 56mg/dL in the 5-year trial and 36 mg/dL in the ORIGIN trial) or prompt recovery after oralcarbohydrate, intravenous glucose or glucagon administration.Percentages of LANTUS-treated adult patients experiencing severe symptomatic hypoglycemiain the LANTUS clinical trials [see Clinical Studies (14)] were comparable to percentages ofNPH-treated patients for all treatment regimens (see Tables 5 and 6). In the pediatric phase 3clinical trial, children and adolescents with type 1 diabetes had a higher incidence of severesymptomatic hypoglycemia in the two treatment groups compared to the adult trials with type 1diabetes.Table 5: Severe Symptomatic Hypoglycemia in Patients with Type 1 DiabetesPercent ofpatientsStudy AType 1 DiabetesAdults28 weeksIn combination withregular insulinLANTUSNPHN 292N 29310.615.0Study BType 1 DiabetesAdults28 weeksIn combination withregular insulinLANTUSNPHN 264N 2708.710.4Study CType 1 DiabetesAdults16 weeksIn combination withinsulin lisproLANTUSNPHN 310N 3096.55.2Study DType 1 DiabetesPediatrics26 weeksIn combination withregular insulinLANTUSNPHN 174N 17523.028.67Reference ID: 4519571
Table 6: Severe Symptomatic Hypoglycemia in Patients with Type 2 DiabetesPercent ofpatientsStudy EType 2 DiabetesAdults52 weeksIn combination with oralagentsLANTUSNPHN 289N 2811.71.1Study FType 2 DiabetesAdults28 weeksIn combination with regularinsulinLANTUSNPHN 259N 2590.4Study GType 2 DiabetesAdults5 yearsIn combination with regularinsulinLANTUSNPHN 513N 5042.37.811.9Table 7 displays the proportion of patients experiencing severe symptomatic hypoglycemia in theLANTUS and Standard Care groups in the ORIGIN Trial [see Clinical Studies (14)].Table 7: Severe Symptomatic Hypoglycemia in the ORIGIN TrialPercent of patientsORIGIN TrialMedian duration of follow-up: 6.2 yearsLANTUSStandard CareN 6231N 62735.61.8Peripheral EdemaSome patients taking LANTUS have experienced sodium retention and edema, particularly ifpreviously poor metabolic control is improved by intensified insulin therapy.LipodystrophyAdministration of insulin subcutaneously, including LANTUS, has resulted in lipoatrophy(depression in the skin) or lipohypertrophy (enlargement or thickening of tissue) in some patients[see Dosage and Administration (2.2)].Insulin Initiation and Intensification of Glucose ControlIntensification or rapid improvement in glucose control has been associated with a transitory,reversible ophthalmologic refraction disorder, worsening of diabetic retinopathy, and acutepainful peripheral neuropathy. However, long-term glycemic control decreases the risk ofdiabetic retinopathy and neuropathy.Weight GainWeight gain has occurred with some insulin therapies including LANTUS and has beenattributed to the anabolic effects of insulin and the decrease in glucosuria.Allergic ReactionsLocal allergyAs with any insulin therapy, patients taking LANTUS may experience injection site reactions,including redness, pain, itching, urticaria, edema, and inflammation. In clinical studies in adultpatients, there was a higher incidence of treatment-emergent injection site pain in LANTUStreated patients (2.7%) compared to NPH insulin-treated patients (0.7%). The reports of pain atthe injection site did not result in discontinuation of therapy.8Reference ID: 4519571
Systemic allergySevere, life-threatening, generalized allergy, including anaphylaxis, generalized skin reactions,angioedema, bronchospasm, hypotension, and shock may occur with any insulin, includingLANTUS and may be life threatening.6.2ImmunogenicityAs with all therapeutic proteins, there is potential for immunogenicity. All insulin products canelicit the formation of insulin antibodies. The presence of such insulin antibodies may increase ordecrease the efficacy of insulin and may require adjustment of the insulin dose. In phase 3clinical trials of LANTUS, increases in titers of antibodies to insulin were observed in NPHinsulin and LANTUS treatment groups with similar incidences.6.3Postmarketing ExperienceThe following adverse reactions have been identified during postapproval use of LANTUS.Because these reactions are reported voluntarily from a population of uncertain size, it is notalways possible to reliably estimate their frequency or establish a causal relationship to drugexposure.Medication errors have been reported in which other insulins, particularly rapid-acting insulins,have been accidentally administered instead of LANTUS [see Patient Counseling Information(17)]. To avoid medication errors between LANTUS and other insulins, patients should beinstructed to always verify the insulin label before each injection.Localized cutaneous amyloidosis at the injection site has occurred. Hyperglycemia has beenreported with repeated insulin injections into areas of localized cutaneous amyloidosis;hypoglycemia has been reported with a sudden change to an unaffected injection site.7DRUG INTERACTIONSTable 8 includes clinically significant drug interactions with LANTUS.Table 8: Clinically Significant Drug Interactions with LANTUSDrugs that May Increase the Risk of HypoglycemiaDrugs:Intervention:Antidiabetic agents, ACE inhibitors, angiotensin II receptor blocking agents, disopyramide,fibrates, fluoxetine, monoamine oxidase inhibitors, pentoxifylline, pramlintide, salicylates,somatostatin analogs (e.g., octreotide), and sulfonamide antibiotics.Dose reductions and increased frequency of glucose monitoring may be required whenLANTUS is coadministered with these drugs.Drugs that May Decrease the Blood Glucose Lowering Effect of LANTUSDrugs:Intervention:Atypical antipsychotics (e.g., olanzapine and clozapine), corticosteroids, danazol, diuretics,estrogens, glucagon, isoniazid, niacin, oral contraceptives, phenothiazines, progestogens (e.g.,in oral contraceptives), protease inhibitors, somatropin, sympathomimetic agents (e.g.,albuterol, epinephrine, terbutaline), and thyroid hormones.Dose increases and increased frequency of glucose monitoring may be required whenLANTUS is coadministered with these drugs.Drugs that May Increase or Decrease the Blood Glucose Lowering Effect of LANTUSDrugs:Alcohol, beta-blockers, clonidine, and lithium salts. Pentamidine may cause hypoglycemia,which may sometimes be followed by hyperglycemia.9Reference ID: 4519571
Intervention:Dose adjustment and increased frequency of glucose monitoring may be required whenLANTUS is coadministered with these drugs.Drugs that May Blunt Signs and Symptoms of HypoglycemiaDrugs:Intervention:beta-blockers, clonidine, guanethidine, and reserpineIncreased frequency of glucose monitoring may be required when LANTUS is coadministeredwith these drugs.8USE IN SPECIFIC POPULATIONS8.1PregnancyRisk SummaryPublished studies with use of insulin glargine during pregnancy have not reported a clearassociation with insulin glargine and adverse developmental outcomes (see Data). There arerisks to the mother and fetus associated with poorly controlled diabetes in pregnancy (seeClinical Considerations).Rats and rabbits were exposed to insulin glargine in animal reproduction studies duringorganogenesis, respectively 50 times and 10 times the human subcutaneous dose of 0.2units/kg/day. Overall, the effects of insulin glargine did not generally differ from those observedwith regular human insulin (see Data).The estimated background risk of major birth defects is 6% to 10% in women with pregestationaldiabetes with an HbA1c 7 and has been reported to be as high as 20% to 25% in women with aHbA1c 10. The estimated background risk of miscarriage for the indicated population isunknown. In the U.S. general population, the estimated background risk of major birth defectsand miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.Clinical ConsiderationsDisease-associated maternal and/or embryo-fetal riskPoorly controlled diabetes in pregnancy increases the maternal risk for diabetic ketoacidosis,preeclampsia, spontaneous abortions, preterm delivery, and delivery complications. Poorlycontrolled diabetes increases the fetal risk for major birth defects, stillbirth, and macrosomiarelated morbidity.DataHuman dataPublished data do not report a clear association with insulin glargine and major birth defects,miscarriage, or adverse maternal or fetal outcomes when insulin glargine is used duringpregnancy. However, these studies cannot definitely establish the absence of any risk because ofmethodological limitations including small sample size and some lacking comparator groups.Animal dataSubcutaneous reproduction and teratology studies have been performed with insulin glargine andregular human insulin in rats and Himalayan rabbits. Insulin glargine was given to female ratsbefore mating, during mating, and throughout pregnancy at doses up to 0.36 mg/kg/day, which isapproximately 50 times the recommended human subcutaneous starting dose of 0.2 units/kg/day(0.007 mg/kg/day), on a mg/kg basis. In rabbits, doses of 0.072 mg/kg/day, which is10Reference ID: 4519571
approximately 10 times the recommended human subcutaneous starting dose of 0.2 units/kg/dayon a mg/kg basis, were administered during organogenesis. The effects of insulin glargine didnot generally differ from those observed with regular human insulin in rats or rabbits. However,in rabbits, five fetuses from two litters of the high-dose group exhibited dilation of the cerebralventricles. Fertility and early embryonic development appeared normal.8.2LactationRisk SummaryThere are either no or only limited data on the presence of insulin glargine in human milk, theeffects on breastfed infant, or the effects on milk production. Endogenous insulin is present inhuman milk. The developmental and health benefits of breastfeeding should be considered alongwith the mother's clinical need for LANTUS, and any potential adverse effects on the breastfedchild from LANTUS or from the underlying maternal condition.8.4Pediatric UseThe safety and effectiveness of LANTUS have been established in pediatric patients (age 6 to 15years) with type 1 diabetes [see Clinical Studies (14.2)]. The safety and effectiveness ofLANTUS in pediatric patients younger than 6 years of age with type 1 diabetes and pediatricpatients with type 2 diabetes have not been established.The dosage recommendation when changing to LANTUS in pediatric patients (age 6 to 15 years)with type 1 diabetes is the same as that described for adults [see Dosage and Administration (2.2,2.4), Clinical Studies (14)]. As in adults, the dosage of LANTUS must be individualized inpediatric patients (age 6 to 15 years) with type 1 diabetes based on metabolic needs and frequentmonitoring of blood glucose.In the pediatric clinical trial, pediatric patients (age 6 to 15 years) with type 1 diabetes had ahigher incidence of severe symptomatic hypoglycemia compared to the adults in trials with type1 diabetes [see Adverse Reactions (6.1)].8.5Geriatric UseOf the total number of subjects in controlled clinical studies of patients with type 1 and type 2diabetes who were treated with LANTUS, 15% were 65 years of age and 2% were 75 years ofage. The only difference in safety or effectiveness in the subpopulation of patients 65 years ofage compared to the entire study population was a higher incidence of cardiovascular eventstypically seen in an older population in the LANTUS and NPH treatment groups.Nevertheless, caution should be exercised when LANTUS is administered to geriatric patients.
5.1 Never Share a LANTUS SoloStar Prefilled Pen, Syringe, or Needle Between Patients LANTUS SoloStar prefilled pens must never be shared between patients, even if the needle is changed. Patients using LANTUS vials must never re-use or share needles or syringes with another person. Sharing poses a risk for transmission of blood-borne pathogens .