Transcription
Table of ContentsState/Territory Name:MaineState Plan Amendment (SPA) #: 22-0002This file contains the following documents in the order listed:1) Approval Letter2) CMS 179 Form/Summary Form (with 179-like data)3) Approved SPA Pages
DEPARTMENT OF HEALTH & HUMAN SERVICESCenters for Medicare & Medicaid Services601 E. 12th St., Room 355Kansas City, Missouri 64106CENTERS FOR MEDICARE & MED ICAID SERVICESCENTER FOR MEDICAID & CHIP SERVICESMedicaid and CHIP Operations GroupApril 21, 2022Michelle Probert, DirectorOffice of MaineCare ServicesDepartment of Health and Human Services109 Capitol Street, 11 State House StationAugusta, Maine 04333-0011Re: Maine State Plan Amendment (SPA) 22-0002Dear Ms. Probert:The Centers for Medicare & Medicaid Services (CMS) reviewed your Medicaid State PlanAmendment (SPA) submitted under transmittal number (TN) 22-0002. This amendmentproposes to implement the Primary Care Plus (PCPlus) Program to replace Maine’s threeexisting primary care programs with a single simplified and integrated program.We conducted our review of your submittal according to statutory requirements in Title XIX ofthe Social Security Act and implementing regulations that generally require states to assurenecessary transportation for beneficiaries to and from covered services. This letter is to informyou that Maine Medicaid SPA 22-0002 was approved on April , 2022, with an effective dateof July 1, 2022.If you have any questions, please contact Gilson DaSilva at (617) 565-1227 or via email atgilson.dasilva@cms.hhs.gov.Sincerely,James G. Scott, DirectorDivision of Program Operationscc: Kristin Merrill, State Plan Manager, Office of MaineCare Services
FORM APPROVED0 MB No. 0938-0193DEPARTMENT OF HEALTH ANDHUMAN SERV ICESCENTERS FOR MEDICARE & MEDICAID SERVICES2.STATE1. TRANSMITTAL NUMBERTRANSMITTAL AND NOTICE OF APPROVAL OFSTATE PLAN MATERIALFOR: CENTERS FOR MEDICARE & MEDICAID SERVICES22---Maine (ME)0002- -----3. PROGRAM IDENTIFICATION: TITLE XIX OF THESOCIALSECURITY ACTTO: CENTER DIRECTORCENTERS FOR MEDICAID & CHIP SERVICESDEPARTMENT OF HEALTH AND HUMAN SERV ICES4. PROPOSED EFFECTIVE DATE5. FEDERAL STATUTE/REGULATION CITATION6. FEDERAL BUDGET IMPACT (Amounts in WHOLE dollars) NIAa FFY202104/01 /2022 07/01 /20221905(t) if the Social Security Actb. FFY7. PAGE NUMBER OF THE PLAN SECTION OR ATTACHMENTAttachment 3.1-A Pages 17-23 and Attachment 4.19-Bpages 10-152022 NIA8. PAGE NUMBER OF THE SUPERSEDED PLAN SECTIONOR ATTACHMENT (IfApplicable)NEW9. SUBJECT OF AMENDMENTImplementing Maine's Primary Care Plus (PCPlus) model.10. GOVERNOR'S REVIEW (Check One)r ···,!GOVERNOR'S OFFICE REPORTED NO COMMENTDG OTHER. AS SPECIFIED:COMMENTS OF GOVERNOR'S OFFICE ENCLOSED NO REPLY RECEIVED W ITH IN 45 DAYS OF SUBMITTAL15. RETURN TO11. SIGNATURE OF STATE AGENCY OFFICIALMichelle ProbertDirector, MaineCare Services#11 State House Station109 Capitol StreetAugusta, Maine 04333-001112 . TYPED NAMEMichelle Probert13. T ITLEDirector MaineCare Services14 . DATE SUBMITTEDJanua21 2022FOR CMS USE ONLY16. DATE RECEIVED 01/21 /202217. DATE APPROVED 0412 1/2022PLAN APPROVED· ONE COPY ATTACHED 1,1.:.;;: .:.··.: 18 . EFFECTIVE DATE OF APPROVED MATERIAL04/0 1/202220. TYPED NAME OF APPROV ING OFFICIALJames G. Scott .:.21. T ITLE OF APPROV ING OFFICIALDirector, Division of Program Operations22. REMARKS04/20/2022 - State provided pen-and-ink authority to revise the effective date to July 1, 2022.FORM CMS-179 (09/24)IiiInstructions on Back
STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACTSTATE: MaineAttachment 4.19-BPage 10Methods and Standards for Establishing Payments rates31. PRIMARY CARE PLUSDEFINITIONS: see Attachment 3.1-A, page 18MEMBER ATTRIBUTIONAttribution is the process of assigning members to a primary care provider (PCP) panel. MaineCaremembers will be attributed to a PCP if all the following criteria are met:A. The member is eligible for all MaineCare state plan services; andB. The member has received at least one eligible Primary Care Service from a PCP during theAssessment Period or has contacted MaineCare Member Services to request assignment to aparticipating practice.If the above criteria are not met, a member will not be attributed.The Department shall attribute members to a provider on a quarterly basis. Attribution will be based onwhere the member received a plurality of eligible Primary Care Services during the Assessment Period. Inthe case of a tie, the most recent visit determines attribution. Regardless of primary care serviceutilization, members may also contact MaineCare Member Services to select assignment to a PCP whichwill be incorporated with the subsequent quarter’s attribution, since billing units are quarterly (paid outmonthly). If the Member does not receive at least one Primary Care Service from the PCP they selectedfor one year from the selection date, the Department will notify the Member and reassign them inaccordance with the Primary Care Services claims-based methodology. Members may not be attributed tomore than one PCP at any point in time. The Department shall provide Member panel and paymentreports to participating PCPs via a secure online portal on a monthly basis. Providers can notify theDepartment of any discrepancy regarding their panel or reports. Providers can appeal Departmentalactions, including payment.There is no minimum number of attributed members required for provider participation, nor does theDepartment set a maximum number of allowable attributed members.TN No. 22-0002SupersedesTN No. NEWApproval Date ϬϰͬϮϭͬϮϬϮϮEffective 7/1/2022
STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACTSTATE: MaineAttachment 4.19-BPage 11Methods and Standards for Establishing Payments ratesPAYMENT METHODOLOGYPopulation-Based PaymentPopulation-Based Payments (PBPs) are monthly payments that the Depa1tment shall calculate quarterly foreach paiticipating PCP. Only one payment will be made to a single PCP per Member in order to preventduplication. The Depaitment will check eligibility status monthly, prior to each monthly payment, toensure providers ai·e only being paid for cun ently eligible and enrolled members.The Depaitment calculates the PBP by adding the Tier PMPM Rate and the Population Group and RiskCatego1y PMPM Rate and multiplying the sum by the PCP's total number of Attlibuted Members. BothPMPM rates are detemrined annually.A. Tier PMPM RateThis PMPM rate is detennined by the provider's Tier,, as defined in Attachment 3. 1-A, and theDepa1tment adjusts this PMPM rate by the Perf01mance-Based Adjustment (PBA) when calculatingthe PBP. Each Tier has a PMPM rate:Tier One: 2.10Tier Two: 6.30Tier Three: 6.90B. Population Group and Risk Catego1y PMPM RateAnnually, the Depa1tment will assign Members to a population group based on their eligibilitycatego1y in the most recent month of the Assessment Period and a risk catego1y based on the mostrecent Risk Score. The population groups ai·e children, adults, aged/blind/disabled, and dual-eligible.The Iisk categories ai·e "generally well" and "complex." Each combination of population group andrisk catego1y has a PMPM rate (see Figure 1). The Depa1tment calculates the overall PMPM rate bymultiplying the number of attributed Members the PCP has in each combination of population groupand 1isk catego1y by the assigned PMPM rate. The Depa1tment then adds the totals from eachcombination and divides by the PCP's number of Members to result in an average PMPM rate.Providers may request a reassessment of their Population Group and Risk Catego1y PMPM if there is asignificant change within the practice, such as a relocation or inclusion of a new population.Reassessments will result in a change to the PMPM for the following qua1ter.More info1mation on the 1isk score model and the risk categolies of "generally well" and "complex" is found·'ders/value-based-cai·eory PMPM ratesChildrenAdultsA0 ed, Blind, DisabledDualsTN No. 22-0002SupersedesTN No. NEW 1.65 2.25 2.50 3.00 6.60 8.75Approval Date 04/21/2022Effective 7/1/2022
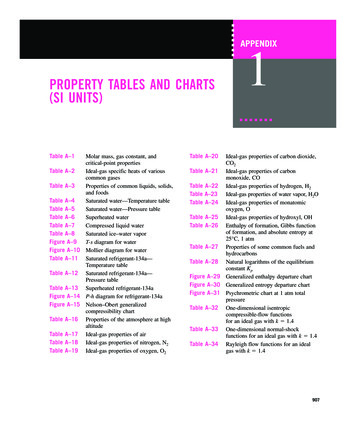
STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACTSTATE: MaineAttachment 4.19-BPage 12Methods and Standards for Establishing Payments ratesPerformance-Based AdjustmentsThe PBA is based on a PCP’s performance on no more than ten (10) quality measures. Current qualitymeasures will be listed on: ed-purchasing/primarycare. The PBA may range from negative ten percent (-10%) to a positive twenty five percent (25%) and isapplied quarterly to the Tier PMPM rate.For the first year of the PCPlus program, the Department will apply a PBA of 25% to Tier One PCPs,8.3% to Tier Two PCPs, and 7.6% to Tier Three PCPs. Performance data will be shared for informationalpurposes only during this time period.One year after the effective date of the PCPlus program, the Department will calculate and apply thePBA, as described herein.A. Calculation of PBA. The PBA equals the sum of the quality measures’ Improvement andAchievement Adjustments (see subparts 3 and 4), which are based on a PCP’s Percentile Score (seesubpart 1) for each quality measure and each quality measure’s domain (see subpart 2).1. Percentile Score. To calculate the Percentile Score, the Department first calculates the PCP’sperformance on each quality measure. Calculating performance varies for each measure. Forexample, performance on the Lead Testing in Children quality measure equals the percentage ofMembers two (2) years of age who had at least one capillary or venous lead blood test for leadpoisoning by their second birthday.The Department then compares the PCP’s performance on each quality measure with theperformance of the PCPs in its MaineCare Peer Group to determine its Percentile Score for eachquality measure. A PCP’s Percentile Score represents the percentage of PCPs that performedbelow the PCP’s performance level, e.g. a PCP with a Percentile Score of 65% performed betterthan 65% of the PCPs in its MaineCare Peer Group.2. Domain. Each quality measure falls under either the Utilization or Comprehensive Care domain.For example, Acute Hospital Utilization falls under the Utilization domain, and DevelopmentalScreening in the First Three Years of Life and Total Cost of Care fall under the ComprehensiveCare domain. Each domain has a unique set of Improvement and Achievement Adjustmentpercentages that apply to the quality measures that fall under each domain (see Figure 2). Thetotal minimum and maximum adjustment amounts from the quality measure(s) under theUtilization and Comprehensive Care domains are 30% and 70%, respectively, of the minimumand maximum PBA.TN No. 22-0002SupersedesTN No. NEWApproval Date ϬϰͬϮϭͬϮϬϮϮEffective 7/1/2022
STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACTSTATE: MaineAttachment 4.19-BPage 13Methods and Standards for Establishing Payments rates3. Improvement Adjustment. The Department will determine Improvement Adjustments bycomparing the PCP’s Percentile Score for each quality measure in the most recent AssessmentPeriod to the PCP’s Percentile Score in the calendar year that falls two (2) years prior to the enddate of the current Assessment Period, e.g. an Assessment Period ending July 30, 2023 would becompared to calendar year 2021.A PCP’s Percentile Score must improve by at least three percent (3%), regardless of whether thePCP’s MaineCare Peer Group is different than its MaineCare Peer Group in the comparison year,to be eligible for the Improvement Adjustment, e.g. a PCP with a Percentile Score of 65% in thecomparison year would have to achieve a Percentile Score of at least 68% in the AssessmentPeriod to obtain the Improvement Adjustment for a quality measure (see Figure 2).4. Achievement Adjustment. The Department will determine Achievement Adjustments for eachquality measure based on Percentile Score (see Figure 2).a. Through December 31, 2023, the Department will calculate Percentile Scores for theAchievement Adjustments by comparing the PCP’s performance to its MaineCare PeerGroup’s performance from the most recent Assessment Period.b. Beginning January 1, 2024, the Department will calculate Percentile Scores for theAchievement Adjustments by comparing the PCP’s performance from the most recentAssessment Period to the performance of its MaineCare Peer Group in the calendar year thatfalls two (2) years prior to the end date of the current Assessment Period. These benchmarkswill be posted on the following website by July 1, e-based-purchasing/primary-care (effectiveJuly 1, 2023).5. Methodology Illustration. To illustrate the methodology, Figure 2 shows that a PCP with aPercentile Score between 60% and 69% for the Acute Hospital Utilization quality measure wouldreceive an Achievement Adjustment of 1.5%. If the PCP’s Percentile Score improved by at least3% from the comparison year, it would also earn the 1.3% Improvement Adjustment. If the PCPearned a Percentile Score between 50% and 59% for the Total Cost of Care quality measure, itwould receive a 0.3% Achievement Adjustment. If the PCP’s Percentile Score did not improve byat least 3% from the comparison year, it would not earn the 0.1% Improvement Adjustment. Thisassessment is done for each quality measure, and the PBA equals the sum of the Achievementand Improvement Adjustments.TN No. 22-0002SupersedesTN No. NEWApproval Date ϬϰͬϮϭͬϮϬϮϮEffective 7/1/2022
STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACTSTATE: MaineAttachment 4.19-BPage 14Methods and Standards for Establishing Payments ratesRESERVED FOR FUTURE USETN No. 22-0002SupersedesTN No. NEWApproval Date ϬϰͬϮϭͬϮϬϮϮEffective 7/1/2022
STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACTSTATE: MaineAttachment 4.19-BPage 15Methods and Standards for Establishing Payments ratesFigure 2. Achievement and Improvement Adjustments* under the Utilization and ComprehensiveCare domains, adapted from the Centers for Medicare and Medicaid Innovation Ptimary Care Firstmethodoloe:v.Comprehensive CarePercentile ScoresUtilizationRelative to Peer GroupAchievementadjustment (%)Improvementadjustment (ifearned) (%)Achievementadjustment (%)Improvementadjustment(if earned)(%) 1.51.30.40.470-793.51.01.00.380-895.00.91.50.2 907.00.52.10. 1*The adjustment percentages in Figure 2 are based on using nine (9) quality measures, one (1) under theUtilization domain and eight (8) under the Comprehensive Care domain. If more or fewer qualitymeasures are used, the Depaitment will change the adjustment percentages prop01tionally, so the PBArange remains between negative ten (-10) and 25% and so the total minimum and maximum adjustmentamounts from the quality measure(s) under the Utilization and Comprehensive Care domains remains30% and 70%, respectively, of the minimum and maximum PBA. Tables co1Tesponding to differentmeasure amounts ai·e listed on: edpurchasing/primary-care (effective 7/1/2022).B. The Depaitment shall use a rolling twelve (12)-month Assessment Period to collect claims data for thePBA and apply the PBA six (6) months after the Assessment Period ends to allow for three (3) monthsof claims nm out and three (3) months to calculate the PBA.C. A quality measure will only be used to assess perfo1mance if there is a sufficient quality measureeligible population size to allow for approp1iate assessment. The sufficient quality measure-eligiblepopulation size for each quality measure will be listed based-purchasing/primary-care. If a quality measurecannot be included in the perfo1mance assessment because of an insufficient quality measure-eligiblepopulation size, the respective portion of the PBA for that quality measure will be redistributed equallyamong all other qualifying quality measures within the same domain.D. PCPs must have a sufficient quality measure-eligible population size on at least one (1) qualitymeasure in the Utilization domain and at least three (3) quality measures in the Comprehensive Cai·edomain to be eligible for each quality measure's adjustments within their domain. If a PCP does notmeet the minimum quality measure requirement for a domain, they shall receive a neutral PBA (zeropercent (0%)) for that domain.E. The Depaitment will notify PCPs at least one hundred twenty (120) days prior to any changes to thequality measures. The Department will provide PCPs quaiterly reports on perfo1mance on qualitymeasures, begirming no later than the second quaiter of PCPlus program implementation.TN No. 22-0002SupersedesTN No. NEWApproval Date04/21/2022Effective 7/1/2022
STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACTSTATE: MaineAttachment 3.1-APage 17AMOUNT, DURATION AND SCOPE OF MEDICAL AND REMEDIAL CAREAND SERVICES PROVIDED TO THE CATEGORICALLY NEEDY31. PRIMARY CARE PLUSPrimary Care Plus (PCPlus) is a model that gives Primary Care Providers (PCPs) greaterflexibility and incentives to effectively meet MaineCare members’ health care needs bytransitioning away from a volume-based (fee-for-service) payment system with little connectionto value, toward an approach that provides Population-Based Payments (PBPs) tied to cost- andquality-related outcomes. PCPlus services include locating, coordinating and monitoring healthcare services, in accordance with Section 1905(t) of the Social Security Act.PCPlus seeks to improve health care access and outcomes for MaineCare members,demonstrating cost-effective use of resources, and creating an environment where providers areincentivized to deliver high-value care. Programmatically, Maine will evaluate providerparticipation in this service and whether providers advance through payment tiers, as theirprovider characteristics advance.Maine will also regularly assess provider performance on no more than ten (10) quality measuresto evaluate quality of comprehensive person-centered primary care (e.g. provision of preventiveservices) and control of health care costs (e.g. acute hospitalization). Maine will track overallprogram performance and improvements over time as an indicator of program success. Lastly,Maine will share performance data regularly with providers and offer technical assistance onrelevant topics.TN No. 22-0002SupersededTN No. NEWApproval Date: ϬϰͬϮϭͬϮϬϮϮEffective Date: 7/1/2022
STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACTSTATE: MaineAttachment 3.1-APage 18AMOUNT, DURATION AND SCOPE OF MEDICAL AND REMEDIAL CAREAND SERVICES PROVIDED TO THE CATEGORICALLY NEEDYDEFINITIONS:Attribution Assessment Period is twenty-four- (24) month “lookback” period for member attributionAttributed Members are MaineCare members assigned to a participating PCPlus provider for thepurposes of population-based payments and performance assessment.MaineCare Peer Group is a group of PCPs, determined by the Department, based on Risk Scores andinfluenced by Tier level, practice size, practice type, and rurality, as needed. MaineCare Peer Groupassignment will be determined upon acceptance into PCPlus and reassessed at least annually or when aPCP undergoes a significant change, which may include a relocation or inclusion of new populations.Members are MaineCare members attributed to a PCP for the purposes of service delivery andreimbursement.Performance-Based Adjustments (PBA) are quarterly adjustments made to participating PCPs’ PBPsbased on PCP performance on PCPlus performance measures.Performance-Based Adjustment Assessment Period: is the twelve (12)-month “lookback” period usedfor assessing PBAs.Population-Based Payments (PBP) are monthly payments that the Department calculates quarterly byadding the Tier per member per month (PMPM) rate and the population group and risk category PMPMrate and multiplying the sum by the PCP’s total number of Attributed Members.Primary Care Services are evaluation and management, preventive, and wellness services. See the fulllist of procedure and diagnosis codes used here: edpurchasing/primary-care (Effective date: 7/1/2022)Risk Score is a metric from a patient classification model that evaluates and forecasts individualhealthcare utilization and costs for each individual Member using demographic and heath care data from atwelve-(12) month period with a two-month claims run out period.TN No. 22-0002SupersededTN No. NEWApproval Date: ϬϰͬϮϭͬϮϬϮϮEffective Date: 7/1/2022
STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACTSTATE: MaineAttachment 3.1-APage 19AMOUNT, DURATION AND SCOPE OF MEDICAL AND REMEDIAL CAREAND SERVICES PROVIDED TO THE CATEGORICALLY NEEDYPROVIDER ELIGIBILITY:Eligible providers participating in PCPlus receive PBPs as detailed in Attachment 4.19-B pages10-10(e). All eligible providers must:A. Be approved by the Maine Department of Health and Human Services (the Department)through the PCPlus application process. The application process will open annually, ata minimum, and providers must receive initial approval and subsequently recertifyannually;B. Be a provider or provider group (i.e. solo or group practice) that delivers Primary CareServices, limited to the following:1. A physician (including residents), nurse practitioner, certified nurse midwife, orphysician assistant with a primary specialty designation of pediatrics, generalpractice, family practice/medicine, geriatrics, internal medicine, obstetrics,gynecology, or other specialties approved by the Department, where Primary CareServices account for at least fifty percent (50%) of the service location’s collectivebilling;2. A rural health clinic;3. A federally qualified health center; or4. A tribal health clinic; andC. Meet Tier One PCP requirements. PCPs who meet Tier Two or Tier Threerequirements are eligible for enhanced reimbursement.Tier One PCP Requirements:A. The PCP shall ensure twenty-four (24) hour availability of information for triage andreferral to treatment for medical emergencies. This requirement may be fulfilledthrough an after-hours telephone number that connects the patient to:1. The PCP or an authorized licensed medical practitioner providing coverage for thePCP;2. A live voice call center system or answering service that directs the patient to theappropriate care site or connects the patient to the PCP/authorized covering medicalpractitioner; or3. A hospital, if the PCP has standing orders with the hospital to direct patients to theappropriate care site within the hospital.The following are examples of what does not constitute adequate coverage:x A twenty-four (24) hour telephone number answered only by an answering machinewithout provision for arranging for interaction with the PCP or their coveringprovider;x Referring to hospital Emergency Departments (EDs) that do not offer phone triageor assistance in reaching the PCP or their covering provider; orTN No. 22-0002SupersededTN No. NEWApproval Date: ϬϰͬϮϭͬϮϬϮϮEffective Date: 7/1/2022
STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACTSTATE: MaineAttachment 3.1-APage 20AMOUNT, DURATION AND SCOPE OF MEDICAL AND REMEDIAL CAREAND SERVICES PROVIDED TO THE CATEGORICALLY NEEDYxB.C.D.E.Emergency medical technicians who do not offer phone triage or assistance inreaching the PCP.The PCP shall inform members of their normal office hours and explain to members theprocedures that should be followed when seeking care outside of office hours. The PCPshall update its twenty-four (24)-hour availability information with the Department.The PCP shall ensure that their covering provider(s) is/are authorized to provide allnecessary referrals for services for Members while providing coverage. The coveringprovider shall be a participating MaineCare provider and shall have real-time access tocurrent, up-to-date medical records in the electronic health record during hours they arecovering;Annually, at least one representative from each PCP shall participate in designatedDepartment-sponsored quality improvement initiatives and technical assistanceactivities. The PCP’s representative shall be involved in clinical care, population health,and/or quality improvement.The PCP shall adopt and maintain, at a minimum, a Certified Electronic Health RecordTechnology (CEHRT); andThe PCP shall, annually with the PCPlus application/recertification, submit a completedassessment of the PCP’s Behavioral and Physical Health Integration progress andidentify an area of focus for the following twelve (12) month period to improvebehavioral and physical health integration. The Department will provide the assessmenttool.The PCP shall, as appropriate and at a minimum of once biennially, educate Membersabout the appropriate use of office visits, urgent care clinics, and the ED. PCPs mayprovide this education through methods including, but not limited to, pamphlets,signage, direct discussion, or Member letters.TN No. 22-0002SupersededTN No. NEWApproval Date: ϬϰͬϮϭͬϮϬϮϮEffective Date: 7/1/2022
STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACTSTATE: MaineAttachment 3.1-APage 21AMOUNT, DURATION AND SCOPE OF MEDICAL AND REMEDIAL CAREAND SERVICES PROVIDED TO THE CATEGORICALLY NEEDYTier Two PCP Requirements:Tier two Providers shall meet all Tier One criteria and shall:A. Hold active patient-centered medical home recognition through a Department-approvedorganization OR be approved by the Centers for Medicare and Medicaid Innovation asa Primary Care First practice and participate in the Primary Care First alternativepayment model;B. Maintain a Participant Agreement for data sharing with Maine’s statewide statedesignated Health Information Exchange (HIE). Tribal health clinics may connect tothe HIE as view-only participants;C. Conduct a standard, routine assessment or screening to identify health-related socialneeds of Members and use the results to make necessary referrals;D. Have a current documented relationship with at least one Behavioral Health HomeOrganization in the PCP’s service area that describes procedures and protocols forregular communication and collaboration between the PCP and the Behavioral HealthHome Organization to effectively serve shared members;E. Maintain processes and procedures to initiate and coordinate care with a CommunityCare Team (CCT), in the PCP service area, for Members who are high-risk and/or highcost whose needs cannot be managed solely by the PCP and are eligible for CCTcovered services;F. Offer Medication for Addiction Treatment (MAT) services in alignment with AmericanSociety for Addiction Medicine guidelines for appropriate level of care, have acooperative referral process with specialty behavioral health providers, including amechanism for co-management for the provision of MAT as needed, or be co-locatedwith a MAT provider. Note: MAT services are not billed or reimbursed under thisprogram;G. Offer telehealth as an alternative to traditional office visits and/or for non-office visitsupports and outreach to increase access to the care team and clinicians in a way thatbest meets the needs of Members;H. Include MaineCare Members and/or their families in advisory activities to identifyneeds and solutions for practice improvement;I. Submit to the Department an environmental scan of which populations served by thePCP could benefit from Community Health Worker (CHW) engagement. This scanshall include basic demographic information of the practice to identify populationgroups that may benefit from CHW services and the identification and description ofany CHW services currently offered through the provider’s practice or throughpartnerships with community-based organizations;TN No. 22-0002SupersededTN No. NEWApproval Date: ϬϰͬϮϭͬϮϬϮϮEffective Date: 7/1/2022
STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACTSTATE: MaineAttachment 3.1-APage 22AMOUNT, DURATION AND SCOPE OF MEDICAL AND REMEDIAL CAREAND SERVICES PROVIDED TO THE CATEGORICALLY NEEDYTier Three PCP Requirements:Tier Three Providers shall meet all Tier One and Tier Two criteria, unless otherwise noted,and shall:A. Be included in the list of Accountable Communities (AC) primary care sites forattribution purposes in the AC program;B. Submit an aligned AC and PCPlus Joint Care Management and Population HealthStrategy (Strategy) to the Department on or before July 31st of every year, beginning7/31/2022. The Strategy shall include a high-level description of the process used toensure that care is coordinated, efficient, and based on patient goals and needs;C. Maintain a Participant Agreement for data sharing with Maine’s statewide, statedesignated HIE for the purpose of submitting the required data elements to allow theHIE to produce specified clinical quality measures within PCPlus.TN No. 22-0002SupersededTN No. NEWApproval Date: ϬϰͬϮϭͬϮϬϮϮEffective Date: 7/1/2022
STATE PLAN UNDER TITLE XIX OF THE SOCIAL SECURITY ACTSTATE: MaineAttachment 3.1-APage 23AMOUNT, DURATION AND SCOPE OF MEDICAL AND REMEDIAL CAREAND SERVICES PROVIDED TO THE CATEGORICALLY NEEDYMEMBER INCLUSION:A. Member participation in PCPlus is voluntary. Members may opt out of the PCPlusprogram at any time by contacting MaineCare Member Services, in which case theDepartment shall remove the Member from attribution and no PCP shall receivePCPlus reimbursement for the Member.B. MaineCare members will be attributed to a PCP based on where the member received aplurality of eligible Primary Care Services. Regardless of primary care serviceutilization, members may also contact MaineCare Member Services to selectassignment to a PCP. If the Member does not receive at least one Primary Care Servicefrom the PCP they selected for one (1) year from the selection date or does not receivea plurality of Primary Care Services from the selected PCP, the Department will verifythat the selected PCP is still the Member’s choice. If the Member does not respond, theDepartment will attribute the Member in accordance with the Primary Care Servicesbased
601 E. 12th St., Room 355 Kansas City, Missouri 64106 Medicaid and CHIP Operations Group April 21, 2022 Michelle Probert, Director Office of MaineCare Services Department of Health and Human Services 109 Capitol Street, 11 State House Station Augusta, Maine 04333-0011 Re: Maine State PlanAmendment (SPA) 22-0002 Dear Ms. Probert: