Transcription
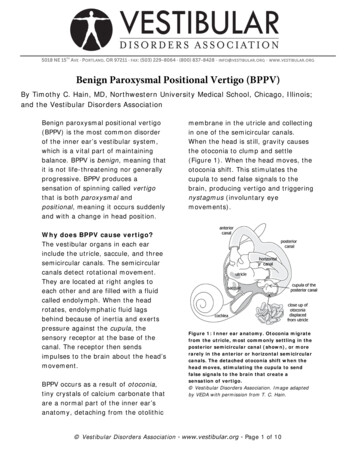
5018 NE 15 TH AVE · PORTLAND, OR 97211 · FAX: (503) 229-8064 · (800) 837-8428 · INFO@VESTIBULAR.ORG · WWW.VESTIBULAR.ORGBenign Paroxysmal Positional Vertigo (BPPV)By Timothy C. Hain, MD, Northwestern University Medical School, Chicago, Illinois;and the Vestibular Disorders AssociationBenign paroxysmal positional vertigo(BPPV) is the most common disorderof the inner ear’s vestibular system,which is a vital part of maintainingbalance. BPPV is benign, meaning thatit is not life-threatening nor generallyprogressive. BPPV produces asensation of spinning called vertigothat is both paroxysmal andpositional, meaning it occurs suddenlyand with a change in head position.Why does BPPV cause vertigo?The vestibular organs in each earinclude the utricle, saccule, and threesemicircular canals. The semicircularcanals detect rotational movement.They are located at right angles toeach other and are filled with a fluidcalled endolymph. When the headrotates, endolymphatic fluid lagsbehind because of inertia and exertspressure against the cupula, thesensory receptor at the base of thecanal. The receptor then sendsimpulses to the brain about the head’smovement.BPPV occurs as a result of otoconia,tiny crystals of calcium carbonate thatare a normal part of the inner ear’sanatomy, detaching from the otolithicmembrane in the utricle and collectingin one of the semicircular canals.When the head is still, gravity causesthe otoconia to clump and settle(Figure 1). When the head moves, theotoconia shift. This stimulates thecupula to send false signals to thebrain, producing vertigo and triggeringnystagmus (involuntary eyemovements).Figure 1: Inner ear anatomy. Otoconia migratefrom the utricle, most commonly settling in theposterior semicircular canal (shown), or morerarely in the anterior or horizontal semicircularcanals. The detached otoconia shift when thehead moves, stimulating the cupula to sendfalse signals to the brain that create asensation of vertigo. Vestibular Disorders Association. Image adaptedby VEDA with permission from T. C. Hain. Vestibular Disorders Association www.vestibular.org Page 1 of 10
Types of BPPVSubtypes of BPPV are distinguished bythe particular semicircular canalinvolved and whether the detachedotoconia are free floating within theaffected canal (canalithiasis) orattached to the cupula (cupulothiasis).BPPV is typically unilateral, meaning itoccurs either in the right or left ear,although in some cases it is bilateral,meaning both ears are affected. Themost common form, accounting for81% to 90% of all cases, iscanalithiasis in the posteriorsemicircular canal.1work and social life, as well as pose ahealth hazard due to an increased riskof falls associated with dizziness andimbalance.SymptomsIn addition to vertigo, symptoms ofBPPV include dizziness (lightheadedness), imbalance, difficultyconcentrating, and nausea. Activitiesthat bring on symptoms can vary ineach person, but symptoms areprecipitated by changing the head’sposition with respect to gravity. Withthe involvement of the posteriorsemicircularcanal in classic BPPV, commonproblematic head movements includelooking up, or rolling over and gettingout of bed.The most common cause of BPPV inpeople under age 50 is head injury and ispresumably a result of concussive forcethat displaces the otoconia. In peopleover age 50, BPPV is most commonlyidiopathic, meaning it occurs for noknown reason, but is generally associatedwith natural age-related degeneration ofthe otolithic membrane. BPPV is alsoassociated with migraine3 and ototoxicity.Viruses affecting the ear (such as thosecausing vestibular neuritis) and Ménière’sdisease are significant but unusualcauses. Occasionally BPPV followssurgery as a result of the trauma on theinner ear during the procedure combinedwith a prolonged supine (laying downface-up) position.4 BPPV may alsodevelop after long periods of inactivity.BPPV may be experienced for a veryshort duration or it may last a lifetime,with symptoms occurring in anintermittent pattern that varies byduration, frequency, and intensity. It isnot considered to be intrinsically lifethreatening. However, it can betremendously disruptive to a person’sCausesBPPV is the most common vestibulardisorder; 2.4% of all people willexperience it at some point in theirlifetimes.1 BPPV accounts for at least20% of diagnoses made by physicianswho specialize in dizziness andvestibular disorders, and is the causeof approximately 50% of dizziness inolder people.2 Vestibular Disorders Association www.vestibular.org Page 2 of 10
Figure 2a: Canalith repositioningprocedure (CRP) for right-sided BPPV.Steps 1 & 2 of CRP are identical to theDix-Hallpike maneuver used to elicitnystagmus for diagnosis. The patient ismoved from a seated supine position; herhead is then turned 45 degrees to theright and held for 15-20 seconds.DiagnosisBPPV is diagnosed based on medicalhistory, physical examination, theresults of vestibular and auditory(hearing) tests, and possibly lab workto rule out other diagnoses. Vestibulartests include the Dix-Hallpikemaneuver (see Figure 2a) and theSupine Roll test. These tests allow aphysician to observe the nystagmus34elicited in responseto a change in headposition. The problematic semicircularcanal can be identified based on thecharacteristics of the observednystagmus.Frenzel goggles, especially of the typeusing a TV camera, are sometimesused as a diagnostic aid in order tomagnify and illuminate nystagmus. Ifelectronystagmography (ENG) is employed to observe nystagmus withposition changes, it is important thatthe equipment used is capable ofmeasuring vertical eye movements. Aphysician may also order radiographicimaging such as a magnetic resonanceimaging scan (MRI) to rule out otherproblems such as a stroke or braintumor, but such scans are not helpfulin diagnosing BPPV.5 In addition, aphysician may order auditory tests tohelp pinpoint a specific cause of BPPV,such as Ménière’s disease orlabyrinthitis.Treating BPPV with in-office particlerepositioning head maneuversRecommended treatment for mostforms of BPPV employs particlerepositioning head maneuvers thatmove the displaced otoconia out of theaffected semicircular canal. Thesemaneuvers involve a specific series ofpatterned head and trunk movementsthat can be performed in a health careprovider’s office in about 15 minutes.Maneuvers for posterior canalBPPVParticle repositioning head maneuvers5are considered to be more effectivethan medication or other forms ofexercise-based therapy6 in treatingposterior canal BPPV. However, evenwith successful treatment with suchmaneuvers, BPPV recurs in about onethird of patients after one year, and inabout 50% of all patients treated afterfive years.7,8,9The canalith repositioning procedure(CRP) is the most common and Vestibular Disorders Association www.vestibular.org Page 3 of 10
empirically proven treatment forposterior canal BPPV.1 Also called theEpley maneuver or the modifiedliberatory maneuver, CRP involvessequential movement of the head intofour positions, with positional shiftsspaced roughly 30 seconds apart(Figure 2a and 2b). Differing opinionsexist about the benefits of usingmastoid vibration during CRP,10 with arecent evidence-based researchreview suggesting that it probablydoes not benefit patients.1Occasionally, when CRP is beingperformed, neurological symptoms(e.g., weakness, numbness, and visualchanges other than vertigo) occur,caused by compression of the vertebralarteries.11 In this case, persisting withthe maneuver can lead to stroke.However, medical professionals canmodify the exercises or use specialequipment so that the positions areattained by moving body and headsimultaneously, thereby avoiding theproblematic compression.The Semont maneuver involves aprocedure whereby the patient israpidly moved from lying on one sideto lying on the other. Although manyphysicians have reported successtreating patients with the Semontmaneuver12 and support its use, morestudies are required to determine itseffectiveness.1Figure 2b: Canalith repositioning procedure (CRP) for right-sided BPPV(continued). In Step 3 of the CRP, the head is turned 90 degrees until the unaffected leftear is facing the floor. The patient turns her body to follow her head, and the position is heldfor 15-20 seconds (Step 4); afterwards, she returns to a seated position (Step 5). Themirror image of these maneuvers can be performed for left-sided BPPV. Vestibular Disorders Association www.vestibular.org Page 4 of 10
Maneuvers for horizontal canal BPPVBecause of the relative rarity of horizontal canal BPPV, there are no best practicesestablished for treatment maneuvers; however, the most widely studied is theLempert maneuver.1 This maneuver entails moving the head through a series of90 angles and pausing between each turn for 10 to 30 seconds. Other techniquessuch as the Gufoni maneuver and the Vannucchi-Asprella liberatory maneuver havealso been used to treat horizontal canal BPPV, but additional well-supported clinicalstudies are needed to assess their effectiveness.1Maneuvers for anterior canal BPPVThere is no definitive treatment foranterior canal BPPV and no controlledstudies of it have yet been completed.However, there is a logical modifiedmaneuver for the anterior canal that isessentially a deep (exaggerated) DixHallpike.13 Other proposed treatmentsemploy reverse versions of themaneuvers used for posterior canalBPPV; for example, the reverseSemont (starting nose down andturned to the unaffected side), or thereverse Epley (again starting nosedown). These treatments aregeometrically reasonable, but requireadditional study to prove theirefficacy.on the side of the treated ear, wear acervical collar as a reminder to avoidquick head turns, and avoid exercisesthat involve looking up or down orhead rotation (such as freestyle lapswimming). Such precautions arethought to help reduce the risk thatthe repositioned debris might return tothe sensitive back part of the earbefore it either adheres or isreabsorbed.Post-treatment considerationsAfter successful treatment withparticle repositioning maneuvers,residual dizziness is often experiencedfor up to three months. Whether posttreatment activity restrictions areuseful has not been adequatelystudied.1 Nevertheless, manyphysicians recommend that theirpatients sleep in an elevated positionwith two or more pillows and/or notVestibular rehabilitation homeexercisesExercises performed at home aresometimes recommended. BrandtDaroff exercises(Figure 3) involve repeating vertigoinducing movements two to threetimes perOther BPPV treatment optionsIf head maneuvers don’t work, othertreatment options include home-basedexercise therapy, surgery, medication,or simply coping with the symptomswhile waiting for them to resolve. Vestibular Disorders Association www.vestibular.org Page 5 of 10
day for up to three weeks. Afterreceiving training from a doctor orphysical therapist, a patient canperform the exercises at home, butthey are more arduous than officetreatments. With adherence to theprescribed schedule, Brandt-Daroffexercises have been reported toreduce vertiginous responses to headmovements in 95% of cases.14Patients performing Brandt-Daroffexercises may develop multicanalBPPV as a complication and so shouldnote any symptom changes to theirphysicians.14Another home exercise method isdaily self-administration of particlerepositioning head maneuvers. Onepotential problem with this method isthat it may cause the condition toworsen or initiate problems in anothersemicircular canal. Although onestudy15 has reported a cure rate ashigh as 95% for this strategy,insufficient evidence exists torecommend or refute its use.For horizontal canal BPPV that doesnot respond to head maneuvers, ahome treatment called forcedprolonged positioning may berecommended. This requires a patientto rest in bed for at least 12 hourswith the head turned toward theunaffected ear, permitting thecanaliths to gradually move out of thecanal.Finally, some physicians suggest thatafter office treatment, patients mightperform a daily self-canalithrepositioning exercise at home tosupport the treatment’s continuedffectiveness. However, such hometreatment probably does not affect thereoccurrence rate of posterior canalBPPV.16Figure 3: Brandt-Daroff exercises. The patient sits upright, turns her head 45 degrees tothe left, then lies down quickly on her right side for 10 seconds. After returning to an uprightseated position, the patient turns her head 45 degrees to the right, lies down quickly on herleft side for 10 seconds, then returns to an upright seated position. Vestibular Disorders Association www.vestibular.org Page 6 of 10
SurgeryIf head maneuvers and vestibularrehabilitation exercises are ineffectivein controlling symptoms, surgery issometimes considered. The goal ofsurgery is to stop the inner ear fromtransmitting false signals about headmovement to the brain. Severalsurgical approaches are possible;however, a procedure called posteriorcanal plugging, also called fenestrationand occlusion of the posterior canal, ispreferable to other methods. Theseinclude removing the balance organswith a labyrinthectomy; severing thevestibular portion of the vestibulocochlear nerve with a vestibular nervesection, thus terminating all vestibularsignals from the affected side; orsevering the nerve that transmitssignals from an individual canal with asingular neurectomy.Canal plugging stops the movement ofparticles within the posteriorsemicircular canal with minimal impacton the rest of the inner ear. Thisprocedure should not be considereduntil the diagnosis of BPPV is certainand all maneuvers or exercises havebeen attempted and foundineffective.17 The surgery poses asmall risk to hearing; some studiesshow it to be effective in 85% to 90%of individuals who have had noresponse to any other treatment,18although further research isrecommended.1MedicationMotion sickness medications aresometimes helpful in controlling thenausea associated with BPPV and aresometimes used to help with acutedizziness during particle repositioningmaneuvers. Otherwise, medicationsare rarely considered beneficial.Medication that suppresses vestibularfunction in the long term can interferewith a person making necessaryadaptations to symptoms or remainingphysically active because of sideeffects such as drowsiness. TheAmerican Academy ofOtolaryngology—Head and NeckSurgery recommends against usingvestibular suppressant medications,including antihistamines andbenzodiazapines, to control BPPV.5Likewise, the American Academy ofNeurology reports that there is noevidence supporting the routine use ofmedication to treat the disorder.1Wait-and-seeSometimes, adopting a “wait-and-see”approach is used for BPPV. Physiciansoften choose to monitor patients withBPPV before attempting treatmentbecause it frequently resolves withoutintervention.1 This may also be theapproach taken with rare variants ofBPPV that occur spontaneously orafter maneuvers and exercises.Coping strategies during this waitand-see phase can involve modifyingdaily activities to help minimizesymptoms. For example, this may Vestibular Disorders Association www.vestibular.org Page 7 of 10
involve using two or more pillowswhile in bed, avoiding sleeping on theaffected side, and rising slowly frombed in the morning. Othermodifications include avoiding lookingup, such as at a high cupboard shelf,or bending over to pick up somethingfrom the floor. Patients with BPPV arealso cautioned to be careful whenpositioned in a dentist’s orhairdresser’s chair, when lying supine,or when participating in sportsactivities.Finding diagnosis and treatmentfor BPPVA list of vestibular disorder specialistsis available from the VestibularDisorders Association (VEDA) Web siteat www.vestibular.org/find-medicalhelp.php. This provider directory isannotated to indicate those specialistswho are trained to perform canalithrepositioning maneuvers.Additional resourcesSome helpful documents available fromVEDA: Benign Paroxysmal PositionalVertigo (BPPV)—What You Need toKnow(Book B-8) Inner Ear Surgeries Meant toControl Vertigo/Disequilibrium(Pub. T-6) Vestibular Rehabilitation: AnEffective, Evidenced-BasedTreatment (Pub. F-7)Video demonstrations of variousparticle repositioning head maneuversare available 2.References1. Fife TD, Iverson DJ, Lempert T,Furman JM, Baloh RW, Tusa RJ, HainTC, Herdman S, Morrow MJ, GronsethGS. Practice parameter: therapies forbenign paroxysmal positional vertigo(an evidence-based review): report ofthe Quality Standards Subcommitteeof the American Academy ofNeurology. Neurol. 2008;70:2067–2074.2. Froehling DA, Silverstein MD, MohrDN, Beatty CW, Offord KP, Ballard DJ.Benign positional vertigo: incidenceand prognosis in a population-basedstudy in Olmsted County, Minnesota.Mayo Clin Proc. 1991;66(6):596–601.3. Ishiyama A, Jacobson KM, Baloh RW.Migraine and benign positionalvertigo. Ann Otol Rhinol Laryngol.2000;109:377–380.4. Atacan E, Sennaroglu L, Genc A,Kaya S. Benign paroxysmal positionalvertigo after stapedectomy.Laryngoscope. 2001;111:1257–1259.5. Bhattacharyya N, Baugh RF, OrvidasL, Barrs D, Bronston L, Cass S,Chalian AA, Desmond AL, Earll JM,Fife TD, Fuller DC, Judge JO, MannNR, Rosenfeld RM, Schuring LT,Steiner RWP, Whitney SL, Haidari J.Clinical practice guideline: benignparoxysmal positional vertigo. ArchOtolaryngol Head Neck Surg.2008;139:S47–S81. Vestibular Disorders Association www.vestibular.org Page 8 of 10
6. Herdman SJ, ed. VestibularRehabilitation. 3rd ed. Philadelphia:F.A. Davis Co.; 2007.7. Nunez RA, Cass SP, Furman JM.Short and long-term outcomes ofcanalith repositioning for benignparoxysmal positional vertigo. ArchOtolaryngol Head Neck Surg.2000;122:647–652.8. Sakaida M, Takeuchi K, Ishinaga H,Adachi M, Majima Y. Long-termoutcome of benign paroxysmalpositional vertigo. Neurol.2003;60(9):1532–1534.9. Brandt T, Steddin S, Daroff RB.Therapy for benign paroxysmalpositioning vertigo, revisited. Neurol.1994;44(5):796–800.10. Hain TC, Helminski JO, Reis I, UddinM. Vibration does not improve resultsof the canalith repositioningmaneuver. Arch Otolaryngol HeadNeck Surg. 2000;126:617–622.11. Sakaguchi M, Kitagawa K, HougakuH, Hashimoto H, Nagai Y, YamagamiH, Ohtsuki T, Oku N, Hashikawa K,Matsushita K, Matsumoto M and HoriM. Mechanical compression of theextracranial vertebral artery duringneck rotation. Neurol.2003;61(6):845–847.12. Levrat E, van Melle G, Monnier P,Maire R. Efficacy of the Semontmaneuver in benign paroxysmalpositional vertigo. Arch OtolaryngolHead Neck Surg. 2003;129(6):629–633.13. Kim YK, Shin JE, Chung JW. Theeffect of canalith repositioning foranterior semicircular canalcanalithiasis. Otorhinolaryngol RelatSpec. 2005;67:56–60.14. Hain TC. Home treatment of BPPV:Brandt-Daroff exercises. Available v.html#home. Accessed Jan 26, 2009.15. Radtke A, von Brevern M, Tiel-WilckK, Mainz-Perchalla A, Neuhauser H,Lempert T. Self-treatment of benignparoxysmal positional vertigo:Semont maneuver vs Epleyprocedure. Neurol. 2004;63:150–152.16. Helminski JO, Janssen I, Hain TC.Daily exercise does not preventrecurrence of benign paroxysmalpositional vertigo. Otol Neurol.2008;29(7):976–981.17. Parnes LS. Update on posteriorcanal occlusion for benign paroxysmalpositional vertigo. Otolaryngol ClinNorth Am. 1996;29(2):333–342.18. Shaia WT, Zappia JJ, Bojrab DI,LaRouere ML, Sargent EW, Diaz RC.Success of posterior semicircularcanal occlusion and application of thedizziness handicap inventory.Otolaryngol Head Neck Surg.2006;134(3):424–430. 2009 Vestibular Disorders AssociationVEDA’s publications are protected under copyright.For more information, see our permissions guide atwww.vestibular.org.This document is not intended as a substitute forprofessional health care. Vestibular Disorders Association www.vestibular.org Page 9 of 10
02/12PO Box 13305 · Portland, OR 97213 · fax: (503) 229-8064 · (800) 837-8428 · INFO@VESTIBULAR.ORG · WWW.VESTIBULAR.ORGDid this free publication from VEDA help you?Thanks to VEDA, vestibular disorders are becomingrecognized for their impacts on lives and our economy.We see new diagnostic tools and research studies,more accessible treatments, and a growing respectfor how life-changing vestibular disorders can be.VEDA provides tools to help people have a betterquality of life: educational materials, support networks,professional resources, and elevated public awareness.Your support of VEDA matters. Please help us tocontinue providing such great help by becominga member or donor.Members receive an information packet; discountson purchases; a subscription to VEDA’s newsletter, Onthe Level, containing information on diagnosis, treatment, research, and coping strategies; and the optionof communicating directly with others who understandthe personal impacts of a vestibular disorder. Professional members also receive the option to list trainingopportunities on our site, bulk-discounted prices onpatient education materials, and a listing on VEDA’sprovider directory, the only of its kind serving patientsseeking help from a vestibular specialist.SSUPPORT VEDAMembership, 1-year 40 Basic 110 ProfessionalMemberships include electronic & online newsletter & freepublications. For hard copies, include optional shipping fees. 5 Shipping (domestic)15 Shipping (international) Please indicate your desiredsubscription amount here.Optional ContributionI’d to support VEDA with adonation (instead of or inaddition to membership). Please indicate your desiredsubscription amount here. Check this box if you preferthat your donation remainanonymous. TotalPAYMENT INFORMATIONIf you prefer, you can make your purchases online at http://www.vestibular.org. Check or money order in US funds, payable to VEDA (enclosed) Visa MC AmexACard numberExp. date (mo./yr.)Billing address of card (if different from mailing information)MAILING INFORMATIONNameAddress CityState/Province Zip/Postal code CountryTelephone E-mail Vestibular Disorders Association www.vestibular.org Page 10 of 10
By Timothy C. Hain, MD, Northwestern University Medical School, Chicago, Illinois; and the Vestibular Disorders Association . Benign paroxysmal positional vertigo (BPPV) is the most common disorder of the inner ear's vestibular system, which is a vital part of maintaining balance. BPPV is benign, meaning that