Transcription
2/13/2020Suicide Risk AssessmentEileen P. Ryan, DOProfessor of Psychiatry and Behavioral HealthVice Chair of Clinical ServicesThe Ohio State University College of MedicineWexner Medical CenterFinancial Disclosures Royalties—Oxford Press Honorariums Grand Rounds Northwestern University American Physicians Institute2 1
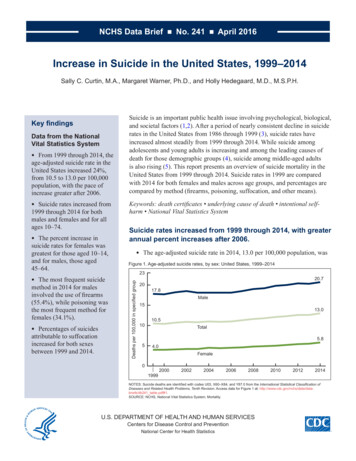
2/13/2020Overview Understanding the nature of suicideRisk factors versus warning signsRisk assessment, not predictionHow to ask about suicideSafety planning and treatment3 Scope of the Problem Suicide is the 10th leading cause of death in the US In the 10- to 34-year old group 2nd leading cause ofdeath 4th leading cause of death ages 35 to 54 8th leading cause of death ages 55-64 1 suicide per 11 minutes in the US In 2017, 47,000 suicides In 2017 the age-adjusted suicide rate was14.0/100,000 ( increase 33% since 1999) In 2017, firearms accounted for almost over 50%suicides4 2
2/13/2020Suicide and Primary Care 45% of individuals who die by suicide sawtheir primary care physician in the monthprior to their death; only 20% saw a mentalhealth professional 60% suicides were suffering from a majordepressive episode at the time of death Primary care doctors write 60% ofprescriptions for antidepressants Primary care providers are on the frontlines of suicide prevention5 Medicolegal Aspects Bad outcome is not an indication of clinician or hospitalnegligence Suicide is a low base rate event and not predictable NO standard of care exists for the PREDICTION ofsuicide Prevention prediction A standard of care does exist for clinicians toadequately assess suicide RISK when it is clinicallyindicated Suicide risk assessment is an informed clinicaljudgment NOT a prediction6 3
2/13/2020The Etiology of Suicidal Ideation (Shea, 2011)Three main etiologies:1. Situational2. Psychological3. BiologicalA blend of these factors are at work in most suicidalindividuals.Suicide has multiple causes. There is no one reason for aperson’s suicide.7 Stress-Diathesis Model of Suicide (Mann et al.) Proximal Factors Mental illnessAlcohol and substance usePsychosocial crisisLethal meansExposure to suicidal behavior Distal factors GeneticsPersonality/temperment (impulsivity, aggression)Childhood traumaPrenatal and perinatal factors8 4
2/13/2020Stress-Diathesis Model of Suicide (Mann et al.) Suicide as a complex interaction betweenstressors (life events or psychologicalpain) and biological susceptibility tosuicidal behavior that is independent ofpsychiatric disorders Proximal risk factors act as triggers orprecipitants when combined with distal riskfactors, thereby increasing the risk forsuicide.9 Precipitants for Suicidal Ideation1. External factors (situational) Public humiliation, job loss, death of a loved one, rejectionby a loved one, serious illness especially one involvingpain or anticipated cognitive deficits2. Psychological factors Cognitive distortions and binds Often exacerbated by stressors and biological factors3. Neurobiological dysfunction Brain changes related to major psychiatric disorders suchas major depression, bipolar disorder, psychosis, andsevere anxiety Toxins such as alcohol and other substances10 5
2/13/2020Risk Factors vs Warning Signs Risk factors are characteristics of a largesample of people who have died bysuicide that appear to be more commonthan in the general population A warning sign (sometimes called riskpredictor) is a characteristic of anindividual that indicates that the person isat more imminent risk for suicide Risk factors and warning signs can overlapin an individual11 Risk Factors History of a suicideattempt Physician Family history of suicidalbehavior, especiallysuicide History of sexual abuse Caucasian Male Increasing age Access to lethal means Alcohol/substance abuse Divorce TBI Prisoner, especially male Mental illness, especiallymood disorders Recent discharge from apsychiatrichospitalization ADHD especiallycomorbid LGBT Self-injurious behavior12 6
2/13/2020Warning Signs Suicidal thoughts orplans Talking or writing aboutdeath or suicide Significant moodchanges Talking about feeling likea burden to others No purpose for living Increasing alcohol ordrug use Increased or decreasedsleep Withdrawing from others Feeling trapped ordesperate Anxiety Agitation Impulsive or recklessbehavior Hopelessness Rage or anger Clinical depression Psychotic thinking13 The Three Tasks of Suicide RiskAssessment1. Obtaining information related to riskfactors and warning signs for suicide in aparticular patient2. Obtaining information related suicidalideation and planning3. Clinical decision-making applied to #1and #2Shea (2002)14 7
2/13/202015 Dear Joanie,I want to explain why you’re reading this note. Mydeath has absolutely nothing and everything to dowith you and Anna. You two have meant everythingto me, but I can no longer live with my own pain andthe pain I am causing you. You have been a rockthrough it all—the hospitalizations, the rehabs, all ofit. There is no way to express my love and gratitudeexcept through my last act—to free you from beingmy caretaker. I’m taking away from all that Annadeserves, and she deserves the best from both of us,but I cannot give that to her. I’ve planned this down tothe last detail, and thank God neither you nor Annawill not be the ones to find my body. Finding myfather marked me for life. Just know that I believe in amerciful God who will forgive me, as I hope you andAnna can. All my love for all eternity.BillSAD PERSONS Scale16 (Patterson, Doan, Byrd et al.,1983)SSexMAAge 19 or 45DDepressionor other mood disorders; hopelessnessPPrevious suicide attemptEEthanolor other substance useRRational thinking losspsychotic thinkingSSocial supports lackingOOrganized planNNo spouseSSicknesschronic debilitating disease8
2/13/2020Guidelines for Action with SADPERSONS(Patterson et al., 1983)TOTAL POINTSPROPOSED CLINICAL ACTION0-2Send home with follow-up3-4Close follow-up; consider hospitalization5-6Strongly consider hospitalizationdepending on strength of the follow-uparrangement 7Hospitalize or commit17 The NO HOPE Scale(Shea,1987)NNo framework for meaningOOvert change in clinical conditionHHostile interpersonal environmentOOut of hospital recentlyPPredisposing personality factorsEExcuses for dying to help others18 9
2/13/2020Dear Joanie,I want to explain why you’re reading this note. My deathhas absolutely nothing and everything to do with you andAnna. You two have meant everything to me, but I can nolonger live with my own pain and the pain I am causing you.You have been a rock through it all—the hospitalizations,the rehabs, all of it. There is no way to express my loveand gratitude except through my last act—to free you frombeing my caretaker. I have been a failure as a husband andfather. I’m taking away from all that Anna deserves, andshe deserves the best from both of us, but I cannot givethat to her. I’ve planned this down to the last detail, andthank God neither you nor Anna will not be the ones to findmy body. Finding my father marked me for life. Just knowthat I believe in a merciful God who will forgive me, as Ihope you and Anna can. All my love for all eternity.19 BillScreening versus Risk Assessment Suicide screening is not the same as suicide riskassessment. Screening is typically done in non-mental healthsettings (primary care and ED) The problem with data and statistics No evidence that routine screening for SI in primarycare settings actually decreases suicide attempts ormortality, but . 54% of people who died by suicide did not have aknown mental health condition (CDC, NAMIwebsites)20 10
2/13/2020Suicide Screening Typically takes the form of validated instruments, but dolittle more than identify those for whom a more thoroughassessment is needed. PHQ-9 Useful for screening but not for diagnosis of MDD Some indication that item 9 may not be adequate forscreening for suicidal ideation and risk (Na et al., 2018) Columbia Suicide Screen Risk Scale (C-SSRS) ED-SAFE ASQ-421 Patient Health Questionnaire (PHQ-9)(Kroenke, Spitzer, Williams 2001)22 11
2/13/2020Columbia-Suicide Severity Rating Scale(C-SSRS)With Triage Points for Primary Care23 ED-SAFE Study (Miller et al, 2017)24 12
2/13/2020Suicide Screening—PediatricAsk Suicide-Screening Questions (ASQ)—ages 10-24 In the past few weeks have you wished you were dead? In the past few weeks, have you felt that you or yourfamily would be better off if you were dead? In the past week, have you been having thoughts aboutkilling yourself? Have you ever tried to kill yourself?If “Yes” to any of the above: Are you having thoughts of killing yourself right now? .shtml25 Suicide Risk Assessment More comprehensive than screening and done by aclinician (including a primary care physician) trained toassess risk No screening or assessment tool is a substitute forclinical judgment, but: Must know major risk factors for completed suicide Best defense in the event of a poor outcome is the abilityto: Convey a knowledge of the subject area Documentation of having performed a psychiatricevaluation Documentation of having performed a risk assessment Documentation of rationale with respect to treatmentand disposition26 13
2/13/2020Suicide Risk AssessmentThe following guideline for a suiciderisk assessment is not a recipe—theelimination of one or more of theseitems does NOT necessarily indicatean inadequate risk assessment27 Suicide Risk AssessmentMajor Risk Factors for CompletedSuicide Prior suicide attemptsFamily history of suicidal behaviorMental illness, especially mood disordersSubstance or alcohol abuseAccess to lethal means28 14
2/13/2020Other Risk Factors Caucasian Male Access to lethal means Divorce; significant loss TBI Physician Prisoner, especially male Trauma history, especially sexual abuse Recent discharge from a psychiatric hospitalization ADHD especially comorbid LGBT Self-injurious behavior29 Suicide Risk AssessmentMental Disorders Mood disorders—major depression and bipolardisorder Psychosis Anxiety—severe anxiety in combination withdepression Substance use disorders Recent increase? Involved in recent attempt? Is there a family history of mental illness? Suicide attempts Death by suicide30 15
2/13/2020Asking about SuicideGoal is to elicit valid information Interview patient separately and in private Appear unhurried Try not to type or take notes when asking about suicide Use segues and ask in a way that does not tap into fearsthat others perceive the patient as weak, “crazy,” selfish,etc.31 Asking about SuicideValidity techniques (Shea, 2011) Behavioral incident—asking for specifics (How many pills did you take?Did you empty the bottle?”) Shame attenuation--Sometimes when people are under a lot of stress,they have thoughts of suicide. Have you ever had thoughts of beingbetter off dead or killing yourself?) Gentle assumption --What often have you thought of killing yourself? Symptom amplification--How many times a day do you think about killingyourself—20, more? Denial of the specific—Have you thought of hanging yourself? Shootingyourself? Normalization—Sometimes when people are depressed, their thoughtsare so intense that they almost seem like voices. Has that ever happenedto you? Some of my patients of my patients with depression have thoughtthat their families would be better off without them. Have you everthought that?32 16
2/13/2020Asking about SuicideSuicidal Ideation Nature of the thoughts—suicide thinking as a continuum Desire to be dead but no thought of killing self Desire to kill self but no plan Desire to kill self with thoughts of how to do so How often do the thoughts occur? Have they increased in frequency or intensity? How do the thoughts make you feel?33 Asking about SuicideLethal Means Does the patient want to die? Does the patient want to be dead now? What methods have been considered and for whatreason? Level of potential lethality Preparatory behaviors Farthest they’ve come Access to lethal means34 17
2/13/2020Asking about SuicideAnticipated Method or Plan Obtain explicit details of plan What?When?Where?How? Have you thought of doing it in a way that no one couldsave you? Do you think this would kill you?35 Suicide Risk AssessmentSocial Supports and Community Resources Work and/or school performance Bullying—not just a “kid” thingExposure Friends or family School/community exposure-contagion? Media ExposureTrauma History Especially sexual abuse36 18
2/13/2020Suicide Risk AssessmentPrevious Attempts Have their been previous attempts to harm self? Self harm versus intent to die Details regarding previous attempts: Plans to avoid detection Potential for lethality Decision making regarding method Medical attention Suicide note Anyone told of plans? Was attempt aborted and how?37 Suicide Risk AssessmentImpulsivityRecent Losses or Legal ConsequencesFuture Orientation Hopeless? Reasons for Living38 19
2/13/2020Protective Factors Protective factors Reasons for living (family, moral, pets, etc.) Religious faith that can be harnessed in positive ways(requires discussion) Research around protective factors is equivocal Hopelessness is a risk/warning sign, but hopefulnessnot protective Religion39 Clinical VignetteMaura is a 38 yo divorced academic researcher with twochildren, ages 1 and 3, who presents with symptoms of aURI. She admits to getting only 2-3 hours of sleep a nightand lays in bed worrying about whether her most recentgrant submission will be funded. She endorses depressionand anxiety, and during adolescence made a suicideattempt by overdose for which she was hospitalized for 2weeks. She mentions that she is under considerable strainbecause one or more of her colleagues are attempting tosabotage her research.She describes her ex-husband as having been physicallyabusive to both her and their children. The court orderedher to pay spousal support, and he has visitation, which heexercises sporadically.40 20
2/13/2020Suicide Risk AssessmentObtain information from collateral sources Confusion regarding HIPAA In an emergency, in life and death issues(which suicide is), do not require consent,but good to obtain anyway. Can ALWAYS listen to information familywants to provide41 Safety Planning Family members and/or close friends should be involved insafety planning—increases buy-in and compliance Warning signs/precipitants and plan to avoid and/or cope Secure/remove lethal agents Individual coping Review reasons for living Distracting activities Relaxation, exercise, etc. Professionals who can help with contact information Crisis names and phone numbers Interpersonal coping Identify friends to help distract or lift mood Identify trusted adults to approach when having suicidalthoughts (parent, relative)42 21
2/13/2020Follow-up Strongest evidence-base is follow-up Phone, text, postcard if unable to get into mentalhealth treatment rapidly and doesn’t want or requirehospitalization Treat depression with therapeutic dosages Follow-up can be life saving especially if mentalhealth treatment is difficult to access or poor—seeweekly or more frequently if necessary The enemy of the good is the perfect—15 minuteswith a doctor who cares is better than waiting 1month for a 1-hour appointment with a therapist43 Thank YouEileeen.ryan@osumc.edu22
The Three Tasks of Suicide Risk Assessment 1. Obtaining information related to risk factors and warning signs for suicide in a particular patient 2. Obtaining information related suicidal ideation and planning 3. Clinical decision-making applied to #1 and #2 Shea (2002) 14 2/13/2020 8 Dear Joanie, I want to explain why you're reading this note.