Transcription
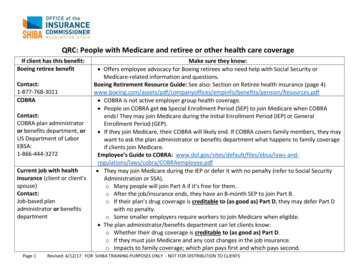
2021RetireeBenefit SummaryEFFECTIVE JANUARY 1, 2021 MEDICAL,D E N TA L ,VIS ION , P R E SC R I P TI OND RU G , A N D L I F EINSURANCEBENEFITSBenefits Plan Highlights for 2021¡¡ The tobacco-user surcharge andattestation will be discontinued.¡¡ There will be no changes toinsurance vendors for 2021.Employee and Retiree Service Center ¡ 45 W. Gude Drive, Suite 1200, Rockville, MD 20850301-517-8100 ¡ www.montgomeryschoolsmd.org/departments/ersc
Board of EducationMrs. Shebra L. EvansPresidentMs. Brenda WolffVice PresidentMs. Jeanette E. DixonDr. Judith R. DoccaVISIONWe inspire learning byproviding the greatestpublic education to eachand every student.MISSIONEvery student will havethe academic, creativeproblem solving, andsocial emotional skillsto be successful incollege and career.CORE PURPOSEMrs. Patricia B. O’NeillMs. Karla SilvestreMrs. Rebecca K. SmondrowskiMr. Nicholas W. AsanteStudent MemberMontgomery CountyPublic Schools (MCPS)AdministrationJack R. Smith, Ph.D.Superintendent of SchoolsMonifa B. McKnight, Ed.D.Deputy SuperintendentPrepare all students tothrive in their future.Henry R. Johnson, Jr., Ed.D.CORE VALUESDerek G. Chief of StaffChief of Engagement, Innovation, and OperationsJanet S. Wilson, Ph.D.Chief of Teaching, Learning, and Schools850 Hungerford DriveRockville, Maryland 20850www.montgomeryschoolsmd.org
Employee and Retiree Service CenterMONTGOMERY COUNTY PUBLIC SCHOOLSRockville, MarylandOctober 6, 2020MEMORANDUMTo:Montgomery County Public Schools RetireesThrough:Mr. Krishna A. Tallur, DirectorEmployee and Retiree Service CenterFrom:Richard C. Johnstone, DirectorBenefits Strategy and Vendor RelationsSubject:Retiree Benefits Open EnrollmentMontgomery County Public Schools (MCPS) will conduct the annual Retiree BenefitsOpen Enrollment Monday, October 12, 2020, through Friday, November 6, 2020. DuringOpen Enrollment, MCPS retirees will have an opportunity to make changes to theirmedical, dental, vision, and prescription plans; drop coverage; or, under certaincircumstances, add coverage that was previously dropped. Changes made during OpenEnrollment will be effective January 1, 2021, which begins the new plan year.It is important to understand your benefit choices and make sure you take any necessaryaction to take advantage of the options available to you. Please read this memorandumcarefully. You should also acquaint yourself with the benefit offerings and premium costsby reviewing the attached 2021 Retiree Benefit Summary and the 2021 Retiree BenefitRate Schedules.Benefits Plan Highlights for 2021 The tobacco-use surcharge and attestation will be discontinued. There are no changes to MCPS-offered medical, prescription, dental, or visionvendors for 2021.Retiree Benefit Plan Open EnrollmentIf you wish to make changes to any component of your benefit plan(s) during the annualretiree Open Enrollment (October 12–November 6, 2020), the Employee and RetireeService Center (ERSC) must receive your changes by the close of business on Friday,November 6, 2020.If you make a change, you will receive a written confirmation of the change. Please reviewthe confirmation upon receipt so any errors may be corrected promptly. Confirmations willbe mailed twice weekly.
MCPS Retirees2October 6, 2020Unbundling Your Benefit PlanYou are given the option to enroll in the full benefit package that includes medical, dental,vision, and prescription drug coverage or choose only those specific components thatmeet your individual needs. For example, if you have medical insurance through anothersource and only require prescription coverage, you may choose prescription coverageonly. You and your eligible dependents must be enrolled in the same benefit plancomponents.If you enroll in the Kaiser Permanente HMO, you also must select Kaiser’s prescriptioncoverage. Kaiser does not permit enrollment in its prescription coverage unless you alsocarry medical coverage with Kaiser. Moreover, the CVS/Caremark prescription plan is notavailable to Kaiser members.If you cancel any component of coverage, you may reenroll during a future retiree OpenEnrollment if that coverage was cancelled on or after July 1, 1998. Also, you will needdocumented proof that you have had other coverage for the 12 months immediatelypreceding reenrollment in the MCPS benefit plan.Open Enrollment Benefit WebinarsDue to the COVID-19 pandemic, ERSC will hold online Open Enrollment BenefitWebinars this year. ERSC staff and representatives from the health plans will be availablevirtually to answer your benefit questions. Dates, times, and plan/vendor options are asfollows:BENEFIT WEBINAR DATES/TIMESBENEFIT OPTIONS/VENDORSMonday, October 12, 20203:00–5:00 p.m.CareFirst Indemnity, POS, and HMO medicalplans for non-Medicare-eligible retireesTuesday, October 13, 20203:00–5:00 p.m.Kaiser Permanente HMO medical andprescription plans for Medicare Advantage andnon-Medicare-eligible retireesWednesday, October 14, 20203:00–5:00 p.m.CareFirst Dental PPO & Aetna DMOThursday, October 15, 20203:00–5:00 p.m.CVS/CareMark and SilverScript prescription drugplansRetirees may make benefit plan changes between Monday, October 12, 2020, andFriday, November 6, 2020. To make and submit your benefits decisions, refer to thisbooklet, the 2021 Retiree Benefit Summary, which includes health plan comparisoncharts and MCPS Form 455-22, Retiree Benefit Plan Enrollment. Also, review the 2021Retiree Benefit Rate Schedules, which details the monthly cost of benefits at each costsharing arrangement while factoring in Wellness Initiatives credits. Both of thesebooklets were mailed to you. They also will be made available online at
MCPS Retirees3October 6, etirees/benefits/ the week beforeOpen Enrollment begins.During Open Enrollment, ERSC staff members will be available to assist you Monday–Friday from 7:30 a.m. to 4:45 p.m. via email at ERSC@mcpsmd.org or by telephone l K. Marella, Chief Financial Officer
2021Montgomery County Public Schools2021 RETIREE BENEFIT SUMMARYMontgomery County Public Schools (MCPS) provides a comprehensive benefit plan for retirees and theireligible dependents. As an eligible MCPS retiree, you have a variety of benefit options from which tochoose, including medical, dental, vision, and prescription drug coverage.The 2021 Retiree Benefit Summary provides an overview of the benefits available to eligible retirees,effective January 1, 2021. This summary includes information about eligibility for MCPS benefits, accessto benefit costs, important contact information, and enrollment forms.Keep in mind that this is a summary of the MCPS retiree benefits and is intended to help you understandand properly enroll in the plan. Full benefit plan details are available on the Employee and RetireeService Center (ERSC) website at www.montgomeryschoolsmd.org/departments/ersc. Informationavailable on the website includes this benefit summary, the Retiree Benefit Rate Schedules, and specificevidence of coverage documents that provide additional details about each plan.During Open Enrollment, ERSC staff is available to assist you via email or by telephone Monday–Friday,from 7:30 a.m.–4:45 p.m. Staff is available throughout the year to assist you via email or by telephoneMonday through Friday from 8:00 a.m.–4:15 p.m. Due to the COVID-19 pandemic, ERSC is closed for inperson service until further notice. Our email address and telephone number are below:Montgomery County Public SchoolsEmployee and Retiree Service Center45 W. Gude Drive, Suite 1200Rockville, Maryland 20850ERSC@mcpsmd.org301-517-8100Important NoticeYou are not enrolled automatically in MCPS retiree benefits. New retirees must enroll 30 days prior to their effective date ofretirement or wait for a future Open Enrollment, held each fall, with coverage effective January 1. In addition, if you or youreligible dependents are Medicare-eligible at your retirement, you will need to submit your Medicare Part A and B card to ERSC60 days prior to your effective date of retirement. You must complete MCPS Form 455-22, Retiree Benefit Plan Enrollment, tojoin the Retiree Benefit Plan. This enrollment form also is used to designate and change beneficiaries for retiree life insuranceor to make changes during Open Enrollment or due to a qualifying life event.RETIREE BENEFIT SUMMARY
2021Table of ContentsAbout Your Benefits . 1Who Can Participate in Open Enrollment? . 1Who is Eligible For Benefits? . 1Who is Ineligible for Benefits? . 1Eligible Dependents . 1Disabled Dependents. 2Adding Dependents . 2Changes in Coverage . 2Loss of Non-MCPS Coverage. 3Paying for Coverage. 3When Benefits Coverage Ends . 3Continuation of Benefits (COBRA) . 3Out-of-Area Coverage. 4Coordination of Benefits . 4Enrollment in Medicare . 5Coordination of Medicare Benefits . 6Medicare Part D . 7Accessing Benefits Forms . 7Your Benefits at a Glance . 8Wellness Initiatives . 9Medical Coverage . 9Point-of-Service (POS) Plan . 10Health Maintenance Organizations (HMOs) . 10Indemnity/Medicare Supplemental Plan . 12Preventive Care Services . 13Other Benefit Plan Coverage . 22Dental Coverage. 22Vision Coverage . 24Prescription Drug Coverage . 25CVS Caremark Prescription Drug Plan. 25Kaiser Permanente Prescription Drug Plans . 29SilverScript/Caremark Medicare Part D Prescription Drug Plan . 30Defined Contribution Plans . 31Life Insurance. 31Retiree Benefit Rates . 32Frequently Requested Websites and Telephone Numbers . 34RETIREE BENEFIT SUMMARY
2021 About Your BenefitsWHO CAN PARTICIPATE IN OPENENROLLMENT? Retirees: who currently are enrolled in an MCPShealth plan; or who retired on or after July 1, 1998, andopted to discontinue their MCPS coverage(Proof of other coverage during the previous12 months is required.)ELIGIBLE DEPENDENTSYou may choose to cover your eligible dependentsunder the MCPS retiree benefit plan. Eligiblecovered dependents must be enrolled in the samebenefits plan in which you are enrolled.WHO IS ELIGIBLE FOR BENEFITS?Eligible dependents include your— spouse, and eligible children who meet the following agerequirements:o until the end of the month in which theyturn 26 for medical and prescriptioncoverageo until the end of the month in which theyturn 24 for dental and vision coverageo until September 30 following their 23rdbirthday for life insurance coverageRetirees with at least five cumulative years ofMCPS-eligible service who*: have a current hire date that is prior toJuly 1, 2006, with no break in employment; or retired on or before July 1, 2011; or were hired prior to July 1, 2011, with at least30 years of eligible service in the state coreplan; or were hired prior to July 1, 2011, and were atleast 55 years of age as of July 1, 2011The documentation you submit to showeligibility of a spouse or child(ren) must includebut is not limited to the following:Retirees with at least 10 cumulative years ofMCPS-eligible service who retired after July 1,2011, and who*: were hired on or after July 1, 2006, andbefore July 1, 2019; and were under 55 years of age as of July 1, 2011Spouse: Social Security number and valid marriage certificate or current joint taxreturn (signed by both parties or a copy ofthe confirmation of electronic submission)Retirees with at least 10 continuous years ofMCPS-eligible service who were*: hired or rehired on or after July 1, 2019*Biological Children: Social Security number and valid birth certificate or valid birthregistration* from most recent hire or rehire date at the time of retirementWHO IS INELIGIBLE FOR BENEFITS? If you retired on or before June 30, 1998,and did not have coverage at that time, youand your dependents are not eligible toenroll in the MCPS plan at any time.If any dependents were not eligible at thetime of your retirement, they are ineligiblefor coverage after you retire.Stepchildren:Social Security number andvalid birth certificate or valid birthregistration and shared or joint custody agreement (courtvalidated) up to age 18If you or your dependents do not meetminimum eligibility requirements asoutlined above, then you are ineligible forcoverage under the MCPS plan.If you were not eligible for coverage as anactive employee, you and/or your dependent(s)are not eligible for coverage after you retire. Adopted Children, Foster Children, Children inGuardianship or Custodial Relationships:RETIREE BENEFIT SUMMARYPAGE 1
2021 Social Security number and one of thefollowing:o adoption documents (court validated)o guardianship or custody documents(court validated)o foster child documents (county, state, orcourt validated) ADDING DEPENDENTSDependents of anyone retired on or beforeJune 30, 1998, who were not covered at thattime, are not eligible for coverage. Children maybe added to your retiree benefit plan up to age26. To enroll a child in your retiree benefits, youmust complete MCPS Form 455-22, RetireeBenefit Plan Enrollment. New spouses and anychildren who were not eligible at the time ofyour retirement are not eligible for coverageunder the plan and may not be added afterretirement. Spouses and/or dependents whowere eligible for benefit coverage at the timeof your retirement may be added or reenrolledwith proof of other coverage during theprevious 12 months.DISABLED DEPENDENTSYour disabled dependent child(ren)’s benefitscoverage may be continued beyond the standardeligibility if— he or she is permanently incapable of selfsupport because of intellectual disability orphysical disability, or he or she became disabled and the disabilityoccurred before he or she reached age 19.Coverage will continue as long as the disabledchild is incapacitated and dependent unlesscoverage is otherwise terminated in accordancewith the terms of the plan. You will be asked toprovide the plan administrator with proof thatthe child’s incapacity and dependency existedprior to age 19. Before the plan administratoragrees to the extension of coverage, the planadministrator may require that a physician,chosen by your health plan provider, examinethe child. The plan administrator may ask forproof that the child continues to meet theseconditions of incapacity and dependency. If youdo not provide proof that the child’s incapacityand dependency existed prior to age 19, asdescribed above, coverage for that child will endat the end of the month in which he/she turnsage 26 for medical and prescription coverage,and at the end of the month he/she turns age 24for dental and vision benefits.CHANGES IN COVERAGEIn general, eligible retirees may enroll in ormake changes to health plans only during OpenEnrollment. However, benefits changes due to aqualifying life event may be made during theplan year. Qualifying life events include: DivorceLoss or gain of alternative coverageChange of work statusRelocation outside your current plan serviceareaRetirementDeathIf you experience a qualifying life event, youhave 60 days from the date of the event tosubmit the required enrollment forms to ERSC.You must use MCPS Form 455-22, RetireeBenefit Plan Enrollment to change your benefitplan enrollment, and you must attach allrequired documentation to the enrollmentform before you submit the form. If you failto submit all required information withMCPS Form 455-22, your form will berejected and returned to you.If you change your medical plan, you will berequired to submit for review new medicaldocumentation to the new health plan provider.It is your responsibility to notify MCPS of thechild’s incapacity and dependency to beconsidered for continuous benefits coverage. IfMCPS is not notified prior to— the dependent’s 24th birthday, dental andvision coverage will be cancelled; andSeptember 30 following the dependent’s 23rdbirthday, life insurance will be cancelled.the dependent’s 26th birthday, medical andprescription benefits will be cancelled;RETIREE BENEFIT SUMMARYPAGE 2
2021If you do not submit the form and requireddocumentation within the 60-day period, youmust wait until a future Open Enrollment tomake any changes.benefits coverage will be effective the first ofthe month following your enrollment.You may drop a dependent or cancel allcoverage at any time by completing MCPS Form455-22, Retiree Benefit Plan Enrollment.Benefit plan premiums are deducted from yourretirement check or directly billed to you whenyour retirement check is not sufficient to coveryour premiums.PAYING FOR COVERAGEHowever, you may not cancel individualcomponents of your benefit plan during the planyear. If you choose to cancel coverage, you mustcancel the entire retiree benefit plan (with theexception of life insurance coverage).Refer to the Retiree Benefit Rate Schedules thatwill be mailed to your home address before OpenEnrollment for your 2021 health coverage costs.WHEN BENEFITS COVERAGE ENDSYou may drop one or more components of yourbenefit plan during the annual Open Enrollment.Retiree coverage is provided to the retiree andeligible surviving spouse for life. Please keep inmind that your medical benefits change whenyou become eligible for Medicare. For moreinformation about how Medicare affects yourMCPS retiree benefits, see the section in thisdocument titled “Enrollment in Medicare.”If ERSC receives your changes by the fifth ofthe month, they will go into effect on the firstday of the following month. If the fifth day ofthe month falls on a weekend or holiday, thedeadline is the last business day prior to thefifth. Enrollment forms received after the fifthday of the month will have coverage commenceon the first day of the second month.IF YOU SUBMIT YOURENROLLMENT FORM:YOUR COVERAGE WILLBEGIN ON:On or before January 5February 1Between January 6and February 5March 1On February 10April 1Benefits coverage for a dependent child’smedical and prescription plans automaticallyends at the end of the month in which he/sheturns 26. Benefits coverage for a dependentchild’s dental and vision plans automaticallyends at the end of the month in which he/sheturns 24. For life insurance coverage, adependent’s coverage ends on September 30tfollowing his/her 23rd birthday.CONTINUATION OF BENEFITS(COBRA)It is your responsibility to promptly notifyERSC of all changes, including removal ofcoverage or death of dependents and changes toname, address, and phone number. Removing adependent’s coverage could change your coveragelevel and reduce your monthly premium.If coverage ends, your dependent(s) may be eligibleto continue coverage as provided under COBRA.LOSS OF NON-MCPS COVERAGEUnder COBRA, your dependent(s) may continuecoverage by paying the full cost of coverageplus a two percent administrative fee for aperiod legally mandated by COBRA regulations(generally 18–36 months).You may enroll in an MCPS-provided benefitsplan during the plan year if you or your benefitseligible dependents lose coverage provided by abusiness or organization other than MCPS. YourMCPS does not share the cost of COBRAcoverage. A COBRA rate chart can be found onthe ERSC website. If your dependents’ coverageends, he/she will receive a qualifying eventRETIREE BENEFIT SUMMARYPAGE 3
2021BlueChoice service area, you may access carewhile traveling/visiting outside your specificservice area by contacting a CareFirst customerservice representative at 1-888-452-6403. Anydependent or retiree who resides or attends schooloutside the service area will only be covered forurgent care or emergency services. You haveaccess to the AFHC Program, which providesbenefits for participants residing outside of thelocal HMO service area for 90 days or more. Someareas of the country do not participate in AFHC.To take advantage of AFHC, contact CareFirstBlueChoice at 1-888-452-6403 for details andenrollment procedures.notice directly from Benefits Strategies, theMCPS third-party COBRA administrator.Benefits may also be available through a StateHealth Insurance Exchange or the nationalAffordable Care Act website.OUT-OF-AREA COVERAGEEach health plan has different requirementswhen retirees travel or reside outside of thecoverage area.Retirees enrolled in the Kaiser PermanenteHealth Maintenance Organization (HMO) arerequired to live in the Kaiser Permanente servicearea (mid-Atlantic). If you are covered by theKaiser Permanente HMO and you live or moveoutside of the Kaiser Permanente service area,please consult ERSC for additional plan options.Eligible dependents who reside or attend schooloutside the service area of the HMO will becovered only for urgent care or emergencyservices. There is no authorization required foremergency services received in an emergencyroom while out of the Kaiser Permanente servicearea. Your dependents must contact the medicalplan for authorization before receiving out-ofarea medical care, and the plan may deny out-ofarea care only for cases in which care is notadministered in an emergency room.Members of the CareFirst BlueChoice POS planhave access to a national network ofapproximately 1 million PPO providers. Thisplan allows you to seek care in-networknationally. If you are covered by the CareFirstBlueChoice POS plan, you also have the optionto see a nonparticipating provider, but your outof-pocket expense will be higher if you do. Ifyou receive services from a provider outside ofthe network, you will have to— pay the provider’s actual charge at the timeyou receive care, file a claim for reimbursement, and satisfy a deductible and coinsurance.COORDINATION OF BENEFITSIf you are enrolled in the CareFirst BlueChoiceHMO Open Access plan, any dependent orretiree who resides or attends school outside theservice area will only be covered for urgent careor emergency services. You have access to theAway From Home Care (AFHC) Program,which provides benefits for participants residingoutside of the local HMO service area for 90days or more. Some areas of the country do notparticipate in the AFHC Program. To takeadvantage of AFHC, contact CareFirstBlueChoice at 1-888-452-6403 for details andenrollment procedures. Enrollment in thisprogram may alter copays and coverage to theplan available in that service area.If you or one of your dependents is covered bymore than one insurance plan, there is an orderof benefits determination established by theNational Association of InsuranceCommissioners. The primary plan will be thefirst to consider the medical services renderedfor coverage. Any medical care not covered infull by the primary plan will be considered forpayment by the secondary plan. Your plan isprimary coverage over any other plan that coversyou as a dependent spouse.If you or your eligible dependents are coveredby Medicare Parts A and B, Medicare alwayswill be primary. For more detailed information see“Enrollment in Medicare” later in this booklet.If you are enrolled in the CareFirst ExclusiveProvider Option (EPO), an HMO plan forretirees living outside of the CareFirstRETIREE BENEFIT SUMMARYPAGE 4
2021the health insurance plan through MCPS will bethe secondary medical coverage.Birthday RuleIf dependent children are enrolled for insurancecoverage with both biological parents (oneMCPS plan, one non-MCPS plan), the primaryinsurance plan for the children is determined bythe birthday of the parents.If you and/or your covered dependent(s) deferredenrollment in Medicare Part B because you wereactively employed, you must contact the SSA atleast three months prior to your retirement dateto enroll in Medicare Parts A and B to coincidewith your retirement date. You must submit acopy of the Medicare card with Parts A and B toERSC with your retirement forms. Instructionsfor enrolling online in Medicare Part B areavailable at https://www.ssa.gov/pubs/EN-0510531.pdf. If you are enrolled in Medicare PartA, be sure to contact your local SSA officebefore enrolling online.The plan of the parent with the birthday thatcomes first in the calendar year (month and dayonly) is primary for the child(ren). This order ofbenefits determination for dependent children isknown as the birthday rule.All medical plans offered by MCPS use thebirthday rule for primary insurance plandetermination. The birthday rule does not applyto stepchildren. Primary care for dependentstepchildren is determined by the courts.Once you apply for Medicare Part B, pleasevisit www.Medicare.gov, register and create ausername and password. This will allow you totrack the progress of your Medicare Part Bapplication at the SSA and provide you withaccess to a PDF version of your Medicare Part Bcard. Please email the pdf version of yourMedicare Part B card to ERSC at ersc@mcpsmd.org.ENROLLMENT IN MEDICAREMCPS requires all participants in the MCPSretiree benefit plan to enroll in Medicare Parts Aand B when first eligible for Medicare in orderto maintain medical and prescription benefitsthrough MCPS.If you and/or your covered dependent(s) becomeeligible for Medicare after you retire, you mustcontact the SSA at least three months before youbecome eligible to enroll in Medicare Parts Aand B. It is the retiree and/or dependent’sresponsibility to enroll in Medicare Parts A andB and submit a copy of the Medicare card toERSC three months prior to the effective date ofMedicare coverage. Sending the Medicare cardto ERSC will initiate the process to notify theinsurance carriers and update your benefitenrollment plan, thereby reducing your monthlypremium.You are eligible for Medicare if you: are age 65 (or over if you have beenemployed and covered by an active grouphealth plan), or receive disability benefits from the SocialSecurity Administration (SSA) and arebeginning the 25th month of entitlement, or have end-stage renal disease (ESRD).You are eligible for Medicare the first day of themonth that you turn age 65 if you have notqualified for enrollment before age 65. If youwill be age 65 on the first day of the month, youwill be eligible for Medicare the first day of theprevious month. ERSC requires that a copy ofthe Medicare card or a benefit entitlement letterfrom S
There are no changes to MCPS-offered medical, prescription, dental, or vision vendors for 2021. Retiree Benefit Plan Open Enrollment If you wish to make changes to any component of your benefit plan(s) during the annual . CareFirst Dental PPO & Aetna DMO Thursday, October 15, 2020 3:00-5:00 p.m. CVS/CareMark and SilverScript prescription drug