Transcription
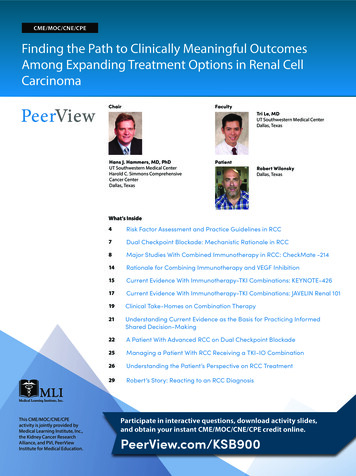
CME/MOC/CNE/CPEFinding the Path to Clinically Meaningful OutcomesAmong Expanding Treatment Options in Renal CellCarcinomaChairFacultyTri Le, MDUT Southwestern Medical CenterDallas, TexasHans J. Hammers, MD, PhDUT Southwestern Medical CenterHarold C. Simmons ComprehensiveCancer CenterDallas, TexasPatientRobert WilonskyDallas, TexasWhat’s InsideThis CME/MOC/CNE/CPEactivity is jointly provided byMedical Learning Institute, Inc.,the Kidney Cancer ResearchAlliance, and PVI, PeerViewInstitute for Medical Education.4Risk Factor Assessment and Practice Guidelines in RCC7Dual Checkpoint Blockade: Mechanistic Rationale in RCC8Major Studies With Combined Immunotherapy in RCC: CheckMate -21414Rationale for Combining Immunotherapy and VEGF Inhibition15Current Evidence With Immunotherapy-TKI Combinations: KEYNOTE-42617Current Evidence With Immunotherapy-TKI Combinations: JAVELIN Renal 10119Clinical Take-Homes on Combination Therapy21Understanding Current Evidence as the Basis for Practicing InformedShared Decision-Making22A Patient With Advanced RCC on Dual Checkpoint Blockade25Managing a Patient With RCC Receiving a TKI-IO Combination26Understanding the Patient’s Perspective on RCC Treatment29Robert’s Story: Reacting to an RCC DiagnosisParticipate in interactive questions, download activity slides,and obtain your instant CME/MOC/CNE/CPE credit online.PeerView.com/KSB900
Activity InformationMedia: Enduring MaterialAccredited Activity Release Date: June 12, 2020Accredited Activity Expiration Date: June 11, 2021Time to Complete Activity: 60 minutesActivity DescriptionIn this virtual educational activity, Hans Hammers, MD, PhD, providesexpert insight on the renal cell carcinoma (RCC) treatment landscape,including an overview of the latest treatment options and safety concernsin frontline therapy, and the use of dual immune checkpoint inhibitors andimmunotherapy-tyrosine kinase inhibitor combinations. He also leads a casediscussion with fellow Tri Le, MD, and a dialogue with a patient diagnosed withRCC, Robert Wilonsky.Target AudienceThis activity has been designed to meet the educational needs of medical andurologic oncologists, advanced practice clinicians, nurses, pharmacists, andother healthcare professionals involved in the care of patients with RCC.Educational ObjectivesUpon completion of this activity, participants will be able to: Evaluate current survival and quality of life evidence in the treatment ofadvanced renal cell carcinoma (RCC) with targeted therapies, immunecheckpoint inhibitors, and combination approaches Select optimal frontline treatment options, such as dual checkpointinhibition or targeted agents plus immune checkpoint inhibitors, forindividual patients with advanced RCC based on the latest evidence,relevant patient- and disease-related characteristics, and patient values andpreferences Recommend effective treatment options for patients with pretreatedadvanced RCC through multiple lines of therapy that reflect considerationsof prior treatment history and patient comorbidities Implement strategies to mitigate and manage treatment-relatedcomplications in patients with RCCProvidership, Credit, and SupportThis CME/MOC/CNE/CPE activity is jointly provided by Medical LearningInstitute, Inc., the Kidney Cancer Research Alliance, and PVI, PeerView Institutefor Medical Education.This activity is supported through an educational grant from Bristol MyersSquibb.Physician Continuing Medical EducationThis activity has been planned and implemented in accordance withthe accreditation requirements and policies of the AccreditationCouncil for Continuing Medical Education (ACCME) through the jointprovidership of Medical Learning Institute, Inc., the Kidney Cancer ResearchAlliance, and PVI, PeerView Institute for Medical Education. The MedicalLearning Institute, Inc. is accredited by the ACCME to provide continuingmedical education for physicians.The Medical Learning Institute, Inc. designates this enduring material for amaximum of 1.0 AMA PRA Category 1 CreditTM. Physicians should claim only thecredit commensurate with the extent of their participation in the activity.MOC StatementSuccessful completion of this CME activity, which includesparticipation in the evaluation component, enables the participant toearn up to 1.0 MOC points and patient safety MOC Credit in the American Boardof Internal Medicine’s (ABIM) Maintenance of Certification (MOC) program.Participants will earn MOC points equivalent to the amount of CME creditsclaimed for the activity. It is the CME activity provider’s responsibility to submitparticipant completion information to ACCME for the purpose of granting ABIMMOC credit.Participation information will be shared with ABIM through the ACCME’sProgram and Activity Reporting System (PARS). Blinded individual oraggregated participant data may be shared with the funder of the activity.Continuing Nursing EducationMedical Learning Institute, Inc. is accredited as a provider ofcontinuing nursing education by the American Nurses CredentialingCenter's Commission on Accreditation.Successful completion of this continuing nursing education activity will beawarded 1.0 contact hour(s).Continuing Pharmacy EducationThe Medical Learning Institute, Inc. is accredited by the AccreditationCouncil for Pharmacy Education as a provider of continuing pharmacyeducation.The Medical Learning Institute, Inc. (MLI) designates this continuing educationactivity for 1.0 contact hours (0.1 CEUs) of the Accreditation Council forPharmacy Education.Universal Activity Number: 0468-9999-20-008-H01-PType of Activity: ApplicationFaculty DisclosuresChairHans J. Hammers, MD, PhDAssociate Professor of Internal MedicineCo-Leader, Kidney Cancer ProgramDivision of Hematology and OncologyUT Southwestern Medical CenterHarold C. Simmons Comprehensive Cancer CenterDallas, TexasHans J. Hammers, MD, PhD, has a financial interest/relationship or affiliation inthe form of:Consultant and/or Advisor for ARMO Biosciences; Bayer; Bristol MyersSquibb; Corvus Pharmaceuticals; Exelixis, Inc.; Merck & Co., Inc.; NovartisPharmaceuticals Corporation; and Pfizer, Inc.Grant/Research Support from Bristol Myers Squibb and Merck & Co., Inc.Honoraria from Bristol Myers Squibb.Other Financial or Material Support from Bristol Myers Squibb and Merck & Co.,Inc. for travel.FacultyTri Le, MDHematology/Oncology FellowUT Southwestern Medical CenterDallas, TexasTri Le, MD, has no financial interests/relationships or affiliations in relation tothis activity.PatientRobert WilonskyDallas, TexasRobert Wilonsky has no financial interests/relationships or affiliations inrelation to this activity.Planning Committee DisclosuresTracy L. Greene, MSN, RN, FNP-C, Nurse Planner, MLI, has nothing to disclose.Teresa Haile, RPh, MBA, Pharmacy Planner, MLI, has nothing to disclose.The planners from Medical Learning Institute, Inc., the accredited provider,PeerView Institute for Medical Education, and the Kidney Cancer ResearchAlliance, joint providers, do not have any financial relationships with anACCME-defined commercial interest related to the content of this accreditedactivity during the past 12 months unless listed below.Dena Battle, Kidney Cancer Research Alliance, has a financial interest/relationship or affiliation in the form of:Advisory Board for Pfizer.Speakers Bureau for EMD Serono and Exelixis.Go online to complete the post-test and evaluation for CME/MOC/CNE/CPE creditPeerView.com/KSB9002
Activity InformationContent/Peer Reviewer DisclosuresThe following Content/Peer Reviewers have nothing to disclose:Natalie I. Vokes, MDAmita B. Patel, MSN, RN, AOCNP, NP-CPatricia A. Ensor, RPh, MBADisclosure of Unlabeled UseThis educational activity may contain discussions of published and/orinvestigational uses of agents that are not indicated by the FDA. The plannersof this activity do not recommend the use of any agent outside of the labeledindications. The opinions expressed in the educational activity are those ofthe faculty and do not necessarily represent the views of the planners. Pleaserefer to the official prescribing information for each product for discussion ofapproved indications, contraindications, and warnings.DisclaimerParticipants have an implied responsibility to use the newly acquiredinformation to enhance patient outcomes and their own professionaldevelopment. The information presented in this activity is not meant to serveas a guideline for patient management. Any procedures, medications, or othercourses of diagnosis or treatment discussed or suggested in this activity shouldnot be used by clinicians without evaluation of their patient's conditions andpossible contraindications and/or dangers in use, review of any applicablemanufacturer's product information, and comparison with recommendationsof other authorities.Method of ParticipationThere are no fees for participating in or receiving credit for this accreditedactivity. For information on applicability and acceptance of continuingeducation credit for this activity, please consult your professional licensingboard.A statement of credit will be issued only upon receipt of a completed activityevaluation form and will be emailed to you upon completion. You will receiveyour certificate from email@email.peerviewpress.com. If you have questionsregarding the receipt of your emailed certificate, please contact via email atinfo@PeerView.com.In order to receive credit, participants must view the activity and complete thepost-test and evaluation form. A score of 70% or higher is needed to obtainMOC/CNE credit. There are no prerequisites and there is no fee to participatein this activity or to receive MOC/CNE credit. Statements of Credit are awardedupon successful completion of the post-test and evaluation form.For Pharmacists: Upon receipt of the completed activity evaluation form, youwill receive an email from email@email.peerviewpress.com within 2 weeks witha link and directions to submit your credit to the NABP CPE Monitor Service. MLIwill accept your completed evaluation form for up to 30 days and will reportyour participation to the NABP only if you provide your NABP e-Profile numberand date of birth. Within 6 weeks, view your participation record at the NABPwebsite: mycpemonitor.net.About This CME/MOC/CNE/CPE ActivityPVI, PeerView Institute for Medical Education, and Medical Learning Institute,Inc. are responsible for the selection of this activity’s topics, the preparationof editorial content, and the distribution of this activity. Our activities maycontain references to unapproved products or uses of these products incertain jurisdictions. The preparation of PeerView activities is supported byeducational grants subject to written agreements that clearly stipulate andenforce the editorial independence of PVI and Medical Learning Institute, Inc.The materials presented here are used with the permission of the authorsand/or other sources. These materials do not necessarily reflect the views ofPeerView or any of its partners, providers, and/or supporters.Go online to complete the post-test and evaluation for CME/MOC/CNE/CPE creditPeerView.com/KSB9003
Finding the Path to Clinically Meaningful Outcomes AmongExpanding Treatment Options in Renal Cell CarcinomaRisk Factor Assessment andPractice Guidelines in RCCHans J. Hammers, MD, PhDUT Southwestern Medical CenterHarold C. Simmons Comprehensive Cancer CenterDallas, TexasDr. Hammers: Hi. My name is Hans Hammers. I’m a medicaloncologist at UT Southwestern Medical Center and the HaroldC. Simmons Comprehensive Cancer Center in Dallas, Texas.Welcome to this educational activity on expanding therapeuticdevelopments in the management of kidney cancer, during whichwe’ll explore advances with frontline treatment.In subsequent segments, I’ll introduce my fellow, Dr. [Tri] Le, fromour group here at UT Southwestern, and we’ll be visiting with oneof our patients, Mr. Robert Wilonsky.Our goal today is to explore some of the recent advances inadvanced renal cell carcinoma, particularly immunotherapyand immune-targeted combinations, and describe what these[advances] have meant for patients suffering from this disease.Let’s begin by reviewing the overall management landscapeand some of the tools that we can use for risk-adapted therapyselection.Know Your Risk: MSKCC and IMDC Risk Criteria1,2Risk Scoring SystemEntry CriteriaMSKCC CriteriaInitial Tx With IFNIMDC CriteriaInitial Tx With TKIKPS 80% 1 y from time of diagnosis to systemic therapy LDH 1.5 ULNHemoglobin LLN (normal: 120 g/L or 12 g/dL) Calcium ULN (normal: 8.5-10.2 mg/dL) So in the early 2000s, Dr. Motzer and his group developed theMemorial Sloan Kettering Cancer Center (MSKCC) criteria in theinterferon era. And what was found was that certain clinicalfactors, such as decreased performance status and decreased timefrom the initial diagnosis to systemic therapy, were factors thatwould predict if patients would not do as well as patients whohave good performance status or [would predict if patients would]have the need for systemic therapy years down the road.There were certain laboratory factors, in particular, anemia andhigh calcium that would also help us to select patients who hadrisk of not doing well, and really, at the end of the day, [were]markers for disease burden, such as organ involvement and theinflammatory state.Those criteria were updated by Drs. Danny Heng and Toni Choueiriand their group, and we now have the International Metastatic RCCDatabase Consortium (IMDC) criteria, which were really developedin the tyrosine kinase inhibitor (TKI) era. And the [criteria] wereslightly modified, but really, they still carry most of the weightfrom the initial criteria, meaning decreased performance status,less than a year from diagnosis to systemic therapy, anemia, andhigh calcium were still carried over into these criteria. But we alsoadded neutrophil counts and platelet counts as indirect markersfor the inflammatory state.Patients who have none of those negative impacting criteria arewhat we call good risk. And they can do really well for a prolongedperiod of time. Neutrophil ULN (normal: 2.0-7.0 x 109/L) Platelets ULN (normal: 150,000-400,000)Distribution of risk groups 0 criteria (favorable) 1-2 criteria (intermediate) 3 criteria (poor)On this slide, you [can] see what we call the risk criteria. The truthis, kidney cancer is quite variable in its natural history, and when Isee a patient for the very first time, I try to gauge how aggressivetheir disease is. And [what] we really worry [about is, do] we needto use very potent effective therapy right now, or [if the patient isin] late recurrence of the disease, can [we just] watch their disease?The survival can really range from months to years, literally.80 pts (18%)269 pts (62%)88 pts (20%)157 pts (18%)440 pts (52%)252 pts (30%)1. Motzer RJ et al. J Clin Oncol. 2002;20:289-296. 2. Heng DY et al. J Clin Oncol. 2009;27:5794-5799.Go online to complete the post-test and evaluation for CME/MOC/CNE/CPE creditPeerView.com/KSB9004
Finding the Path to Clinically Meaningful Outcomes Among Expanding Treatment Options in Renal Cell CarcinomaAnd that’s reflected in the National Comprehensive CancerNetwork (NCCN) guidelines. As you can see here, we are essentiallybreaking down the patient population into two groups, favorablerisk or intermediate and poor risk.Risk Groups and Survival in RCC11FavorableIntermediatePoorProbability of OS0.80.60.4Favorable: 0 factorsMedian OS 43 mo0.2Poor: 3-6 factorsMedian OS 8 moP .0001001020304050Intermediate: 1-2 factorsMedian OS 22 mo60Months Since Therapy Initiation1. Heng DY et al. Lancet Oncol. 2013;14:141-148.As you can see on this slide, on the top, there are favorable-riskpatients and the overall survival. And as you can see, probablyindependent of therapy, these patients do well, and the medianoverall survival is measured in years.If you have three or more of these risk factors, you are poor risk,and the median survival is typically measured in the range ofmonths. And then the patients in the middle are intermediate risk,and have one to two of these risk factors, they’re in between thosetwo extremes, if you will.And we use these criteria to get a sense for how a patient is goingto do initially when we see them. But we also use [the criteria] forclinical trial development and for clinical trial stratification. Wewant to get a sense for how many poor-risk, favorable-risk, andintermediate-risk patients we put on a trial. That might tell ussomething about how the cohort, in general, will do.And in fact, we also [get] a sense that maybe some of these riskgroups may be more amenable to [a particular] therapy versusothers, and we will talk about that a little bit down the road.But really, the initial take-home message is RCC is quite a variabledisease, and we use fairly simple markers to risk-stratify patientsnot only for clinical use, but also for clinical trial development.Standards of Care for Advanced RCC in 2020Options for First-Line Therapy1PreferredRegimensRisk Favorable Poor/intermediate Other RecommendedRegimensAxitinib pembrolizumabPazopanibSunitinib Nivolumab ipilimumab(category 1)Axitinib pembrolizumab(category 1)CabozantinibUseful UnderCertain Circumstances Nivolumab ipilimumabCabozantinib(category 2B)Axitinib avelumab PazopanibSunitinibAxitinib avelumab Patients with excellent performance status and normal organ function.1. NCCN Clinical Practice Guidelines in Oncology. Kidney Cancer. Version n gls/PDF/kidney.pdf. Active surveillanceAxitinib(category 2B)High-dose IL-2aAxitinib(category 2B)High-dose IL-2aTemsirolimusThat is based largely on the outcomes of one study—thenivolumab ipilimumab [study]—for which we have FDAapproval in the poor- and intermediate-risk group only. We do use[nivolumab ipilimumab] sometimes in the favorable-risk group,and we’ll go into that in a second. But I would say the FDA approvalis in the poor- and intermediate-risk groups versus other regimens,such as combinations of PD-1 inhibitors with VEGF inhibitors, andare also approved in the favorable-risk group.And so we have preferred regimens for the favorable-risk groupand for the poor- and intermediate-risk group. It’s also importantto know what’s actually appropriate or covered officially by theFDA approval.Nonetheless, if you look at the favorable-risk group patients, theyactually have quite [a few] options. So if you look at the preferredregimens, typically axitinib pembrolizumab—a regimen thathas shown overall survival benefit—is preferred, for example,over nivolumab ipilimumab or cabozantinib. But these are alsoregimens that are appropriate when a physician feels there’s areason to use those particular combinations.At the end of the day, the favorable-risk patients have a lot ofoptions. Often, these are patients who have late recurrences. Theyhave options of focal therapy, surgery, and radiation. They haveoptions for different systemic therapies.Probably, the preferred [option] in 2020 would be axitinib pembrolizumab, but also, the use of nivolumab ipilimumab andcabozantinib in selected patients are potential options.But also, patients may still use all of the immunotherapies, whichare a little bit difficult to administer, such as high-dose IL-2, andhave shown very durable responses. In fact, we probably believe[some of these agents] are cures in some of these patients whohave a [particular] risk profile of a disease; they can walk into atherapy that might not be too effective up front.In poor-risk patients, it’s really very straightforward. I would saythat typically the two most commonly used regimens are eithernivolumab ipilimumab, so a combination of two immunecheckpoint inhibitors, or axitinib pembrolizumab. Both of theseare preferred regimens, because both of them have shown anoverall survival benefit in these patient populations.aAxitinib avelumab are similar to axitinib pembrolizumab, alsoa combination of the PD-L1 inhibitor, in this case, with a tyrosinekinase inhibitor. But this regimen has not yet shown an overallsurvival benefit, and is therefore more in the category of otherGo online to complete the post-test and evaluation for CME/MOC/CNE/CPE creditPeerView.com/KSB9005
Finding the Path to Clinically Meaningful Outcomes Among Expanding Treatment Options in Renal Cell Carcinomarecommended regimens. So for poor- and intermediate-riskpatients—which, by the way, make up roughly 75% to 80% of thepatients who you will see—[we use] these two regimens.But it really depends on the physician and the patient and theirdiscussions on what will be used as the next line of therapy. Buttypically we would use combinations or agents that haven’t beenused in the front line.Single-agent tyrosine kinase inhibitor use, I would say in generalterms, has clearly declined because patients would like to haveaccess to a therapy that may lead to more durable responses,maybe with a chance of coming off therapy rather than beingexposed to drugs that we feel are purely palliative in nature.Nonetheless, tyrosine kinase inhibitors remain the workhorses inrenal cell carcinoma, and certainly, have [their] place and will keeptheir place in the management of this disease.Standards of Care for Advanced RCC in 2020Options for Second-Line Therapy or Later1Preferred Regimens Cabozantinib(category 1)Nivolumab (category 1)Nivolumab ipilimumabUseful UnderCertain CircumstancesOther Recommended Regimens Axitinib (category 1)Lenvatinib everolimus(category 1)Axitinib pembrolizumabEverolimusPazopanibSunitinibAxitinib avelumab (category 3) Bevacizumab or biosimilar(category 2B)Sorafenib (category 2B)High-dose IL-2 forselected patientsa(category 2B)Temsirolimus(category 2B)Patients with excellent performance status and normal organ function.1. NCCN Clinical Practice Guidelines in Oncology: Kidney Cancer. Version n gls/PDF/kidney.pdf.aWhat about second-line therapy? So that really depends on whatyou used in the frontline therapy. Typically, if [a patient] progresseson a combination, such as axitinib pembrolizumab, you willprobably go directly to a more broadly acting tyrosine kinaseinhibitor, such as cabozantinib.If [the patient] is coming off a tyrosine kinase inhibitormonotherapy, you can then engage them with nivolumab [per]category 1 evidence, or nivolumab ipilimumab, if [the patient]was never exposed to these immune checkpoint inhibitors.But there are also other subsequent combinations. Typically, if[a patient has] failed on immunotherapy, [they] will be managedprimarily with a tyrosine kinase inhibitor of the VEGF pathway. Socabozantinib is a very common initial choice.In some patients who don’t have an overwhelming symptomaticdisease burden, more selective tyrosine kinase inhibitors, if theyaren’t yet used, are also appropriate. For example, patients whohave progressed on nivolumab ipilimumab, we may exposethem to axitinib, which is a more selective VEGF inhibitor. And ifthat drug fails, then we can go to cabozantinib.After cabozantinib, I’ll often use lenvatinib everolimus. [Thiscombination] is approved in the settings of the prior therapies andis a very potent combination. I personally don’t use everolimus assingle agent anymore, simply because this particular combinationseems to be somewhat synergistic and quite effective.Go online to complete the post-test and evaluation for CME/MOC/CNE/CPE creditPeerView.com/KSB9006
Finding the Path to Clinically Meaningful Outcomes Among Expanding Treatment Options in Renal Cell CarcinomaDual Checkpoint Blockade:Mechanistic Rationale in RCCHans J. Hammers, MD, PhDUT Southwestern Medical CenterHarold C. Simmons Comprehensive Cancer CenterDallas, TexasIs CTLA-4 Blockade Synergistic With Anti–PD-1?1,2 The PD-1 receptor on T cellsacts as an “off switch” todownregulate immune responsePD-1TumorB7 PD-1/PD-L1 inhibitors actto destroy cancer cells inboth the lymph node andthe tumor microenvironmentPD-L1T-cell receptorMHC with antigenCD28PD-L1Dendritic cellPD-L1/PD-L2T cellPD-L1PD-1PD-1Lymph NodeTumorMicroenvironment1. Postow MA et al. J Clin Oncol. 2015;33:1974-1982. 2. Lee L et al. J Clin Pharmacol. 2016;56:157-169.Is CTLA-4 Blockade Synergistic With Anti–PD-1?1,2Lymph Node CTLA-4 activation downregulatesthe function of T cells Blockade of CTLA-4 ultimatelyallows upregulation of immuneresponses targeting tumor antigensT-cell receptorMHC with antigenB7Dendritic cellCD28T cellB7CTLA-41. Postow MA et al. J Clin Oncol. 2015;33:1974-1982. 2. Lee L et al. J Clin Pharmacol. 2016;56:157-169.Dr. Hammers: Let’s look into combination immunotherapy.So dual immune checkpoint blockade and immune-targetedcombinations are now the front workhorses in renal cell carcinomain the most recent editions of the practice guidelines. We’ll nowtake a look at the evidence supporting their use in renal cellcarcinoma, starting with immunotherapy combinations.If you look at PD-1, it’s kind of like an off switch for activated T cells,and the interaction of PD-L1, the ligand for the receptor of PD-1,is really important in the tumor microenvironment. So T cells arebeing activated, they infiltrate the tumor and want to destroy theircognate target, but then the PD-L1 may interfere with the activityof these T cells, either directly from tumor cells, or sometimes alsofrom bystander cells, stopping short the T-cell effector response.And we have seen some of those dramatic responses with PD-1/PD-L1 inhibitors, which have really revolutionized immunotherapyacross solid tumors. And so the combination of [CTLA-4 blockadeand PD-1/PD-L1 inhibition] is quite interesting, because theyprobably have different targets. And that’s the rationale for thisparticular combination.But first, let’s explore how dual immunotherapy can alter theimmune and tumor microenvironment and the rationale for itsuse.You have two primary targets with currently approvedimmunotherapy. One is called CTLA-4. This particular target isbroadly expressed and also presents in secondary lymphoidorgans, such as lymph nodes, so at the very earliest stages ofimmune activation when dendritic cells present tumor antigens,for example, to T cells.In that initial interaction, CTLA-4 plays a very important role,and, typically, would downregulate activated T cells after initialstimulation. So you can really drive these cells in hyperdrive andunleash them, if you will, by targeting this particular pathway.The mechanisms for CTLA-4 inhibition, however, arequite complex, and there are other targets in the tumormicroenvironment, such as T-regulatory cells, that also play amajor role.Go online to complete the post-test and evaluation for CME/MOC/CNE/CPE creditPeerView.com/KSB9007
Finding the Path to Clinically Meaningful Outcomes Among Expanding Treatment Options in Renal Cell CarcinomaMajor Studies With CombinedImmunotherapy in RCC:CheckMate -214Hans J. Hammers, MD, PhDUT Southwestern Medical CenterHarold C. Simmons Comprehensive Cancer CenterDallas, TexasI would say at this point it’s important to note that the dosing[regimen] of nivolumab ipilimumab is different than the dosingregimen that we use in melanoma. For melanoma, we use a higherdose of ipilimumab and a lower dose of nivolumab.In the early phase of the development of these particularcombinations in kidney cancer, we tried the doses that were usedin melanoma in renal cell carcinoma. And roughly, the responserates were the same, but the toxicities were higher with the highdose of ipilimumab. And so, the reverse dosing of what we use inmelanoma [is used] in renal cell carcinoma and in other tumors,such as in lung cancer.CheckMate -214: OS in ITT Patients1CheckMate -214: Nivolumab Ipilimumabin Newly Diagnosed Advanced RCC1Stratification IMDC prognostic score(0 vs 1-2 vs 3-6) Region(United States vsCanada/Europe vsrest of the world)Treatment naïve,inoperable, locallyadvanced, ormetastatic RCC Clear cell histologya KPS 70%N 1,096Nivolumab 3 mg/kg, IV Q3W ipilimumab 1 mg/kg, IV Q3Wx 4 doses, thennivolumab 3 mg/kg Q2WR1:1Sunitinib 50 mg orally QD(4 wk on, 2 wk off)Endpoints Coprimary (intermediate/poor risk): PFS, OS, ORR Secondary: safetyProbability of OSKey eligibility criteriaMedian OS(95% CI), m1.00.90.80.70.60.50.40.30.20.10No. at RiskNIVO IPISUNNIVO IPINR (NE)SUN83%71%64%78%61%37.9 (32.2-NE)HR (95% CI) 0.71 (0.59-0.86)P .000356%Nivolumab 4354434044253674103452124Time, 45585545001. Motzer RJ et al. Lancet Oncol. 2019;20:1370-1385.Approximately 70% of patients with RCC have this histology type.1. Motzer RJ et al. Lancet Oncol. 2019;20:1370-1385.aDr. Hammers: Now let’s review some of the evidence leadingto the approval of dual immunotherapy options with nivolumaband ipilimumab for advanced renal cell carcinoma based on theevidence of the CheckMate -214 study.This was a very large study of [over] 1,000 patients. And it accruedall three risk groups. However, the primary cohort of interestfor which the primary endpoints were really designed for wasrestricted to intermediate- and poor-risk patients. So 800 of thesepatients were intermediate and poor risk. And the coprimaryendpoints were progression-free survival, overall survival, andresponse, which were really designed for that particular cohort.There were secondary endpoints, for example, looking at theintent-to-treat population combining all three, meaning favorable,intermediate, and poor risk. But really, the study was designed tolook at intermediate and poor risk specifically.Clear cell renal cell carcinoma patients were accrued, stratified bythe IMDC score and treatment region, and then either treated withnivolumab at 3 mg/kg and ipilimumab at 1 mg/kg followed afterfour of these combination doses with nivolumab at 3 mg/kg orsuniti
A Patient With Advanced RCC on Dual Checkpoint Blockade Managing a Patient With RCC Receiving a TKI-IO Combination Understanding the Patient's Perspective on RCC Treatment Robert's Story: Reacting to an RCC Diagnosis This CME/MOC/CNE/CPE activity is jointly provided by Medical Learning Institute, Inc., the Kidney Cancer Research