Transcription
ConnectiCare Benefits Inc.Individual MarketCompass Gold Alternative POSBenefit SummaryTiered Network PlanCompass Network - Includes Providers in Connecticut onlyDeductible and Out-of-PocketMaximumPreferred ProviderIn-Network (INET)Member PaysPlan deductibleIndividualFamily 2,000 per member 4,000 per familySeparate Prescription DrugDeductibleIndividualFamilyParticipating ProviderIn-Network (INET)Member Pays 3,500 per member 7,000 per familyIncluded in Plan Deductibleper member / per familyOut-of-Network(OON)Member Pays 7,000 per member 14,000 per familyIncluded in PlanDeductibleper member /per familyOut-of-Pocket Maximum 8,150 per member 16,300 per familyIndividualFamily(Includes deductible, copaymentsand coinsurance) 12,000 per member 24,000 per familyPreferred ProviderIn-Network (INET)Member PaysParticipating ProviderIn-Network (INET)Member PaysOut-of-Network(OON)Member PaysAdult/Pediatric PreventiveVisitsNo costSame as PreferredProvider cost share50% coinsurance pervisitPrimary Care Provider Office/Telemedicine Visits(includes services for illness,injury, follow-up care andconsultations) 20 copayment pervisit40% coinsurance pervisit after INET plandeductible50% coinsurance pervisit after OON plandeductible is metTelemedicine Services(services rendered by a Teladoc provider)No costSame as PreferredProvider cost share50% coinsurance pervisit after OON plandeductible is metSpecialist Office/TelemedicineVisits 60 copayment pervisitSame as PreferredProvider cost share50% coinsurance pervisit after OON plandeductible is metMental Health and SubstanceAbuse Office Visits 60 copayment pervisitSame as PreferredProvider cost share50% coinsurance pervisit after OON plandeductible is metBenefitsProvider Office VisitsOutpatient Diagnostic ServicesCBI/POS/Gold Tiered/IND BS (01/2022) 76962CT0040001-00 Effective Date: 1/2022Compass Gold A130348BPL CT P02157557Compass Gold Alternative POSBenefit ID: 40051Product ID: MS0400681
BenefitsPreferred ProviderIn-Network (INET)Member Pays20% coinsurance perservice after INETplan deductible ismet at a PreferredHospital FacilityAdvanced Radiology(CT/PET Scan, MRI)Laboratory ServicesNon-Advanced Radiology(X-ray, Diagnostic)Mammography Ultrasound 40 copayment perservice up to acombined annualmaximum of 375 forMRI and CAT scans; 400 for PET scansat a FreestandingFacility 10 copayment perservice20% coinsurance perservice after INETplan deductible ismet at a PreferredHospital Facility 10 copayment perservice at aFreestandingFacility20% coinsurance perservice after INETplan deductible ismet at a PreferredHospital Facility 10 copayment perservice at aFreestandingFacilityParticipating ProviderIn-Network (INET)Member Pays40% coinsurance perservice after INETplan deductible ismet at a HospitalFacilitySame as PreferredProvider cost sharewhen done at aFreestandingFacilitySame as PreferredProvider cost share40% coinsurance perservice after INETplan deductible ismet at a HospitalFacilitySame as PreferredProvider cost sharewhen done at aFreestandingFacility40% coinsurance perservice after INETplan deductible ismet at a HospitalFacilitySame as PreferredProvider cost sharewhen done at aFreestandingFacilityOut-of-Network(OON)Member Pays50% coinsurance perservice after OON plandeductible is met50% coinsurance perservice after OON plandeductible is met50% coinsurance perservice after OON plandeductible is met50% coinsurance perservice after OON plandeductible is metPrescription Drugs – Retail Pharmacy (cost share based on 30 day supply per prescription)Generic DrugsTier 1 10 copayment perprescriptionSame as PreferredProvider cost share50% coinsurance perprescription afterOON plan deductibleis metPreferred Brand DrugsTier 2 50 copayment perprescriptionSame as PreferredProvider cost share50% coinsurance perprescription afterOON plan deductibleis metCBI/POS/Gold Tiered/IND BS (01/2022) 76962CT0040001-00 Effective Date: 1/2022Compass Gold A130348BPL CT P02157557Compass Gold Alternative POSBenefit ID: 40051Product ID: MS0400682
BenefitsPreferred ProviderIn-Network (INET)Member PaysParticipating ProviderIn-Network (INET)Member PaysOut-of-Network(OON)Member PaysNon-Preferred BrandTier 350% coinsurance perprescription afterINET plan deductibleis metSame as PreferredProvider cost share50% coinsurance perprescription afterOON plan deductibleis metSpecialty DrugsTier 450% coinsurance upto a maximum of 500 perprescription afterINET plan deductibleis metSame as PreferredProvider cost share50% coinsurance perprescription afterOON plan deductibleis metPrescription – Mail Order Pharmacy (up to a 90 day supply per prescription)Generic DrugsTier 1 20 copayment perprescriptionSame as PreferredProvider cost share50% coinsurance perprescription afterOON plan deductibleis metPreferred Brand DrugsTier 2 100 copayment perprescriptionSame as PreferredProvider cost share50% coinsurance perprescription afterOON plan deductibleis metNon-Preferred BrandTier 350% coinsurance perprescription afterINET plan deductibleis metSame as PreferredProvider cost share50% coinsurance perprescription afterOON plan deductibleis metOutpatient Rehabilitative and Habilitative Services (40 visits per calendar year limit combined forRehabilitative physical, speech and occupational therapies. Separate 40 visits per calendar yearlimit combined for Habilitative speech, physical and occupational therapies.)Speech Therapy 50 copayment pervisit after INET plandeductible is metSame as PreferredProvider cost share50% coinsurance pervisit after OON plandeductible is metPhysical and OccupationalTherapy 30 copayment pervisit after INET plandeductible is metSame as PreferredProvider cost share50% coinsurance pervisit after OON plandeductible is metChiropractic Services(up to 20 visits per calendar year) 50 copayment pervisitSame as PreferredProvider cost share50% coinsurance pervisit after OON plandeductible is metDiabetic Equipment andSupplies20% coinsurance perequipment/supplySame as PreferredProvider cost share50% coinsurance perequipment/supplyafter OON plandeductible is metDurable Medical Equipment(DME)20% coinsurance perequipment/supplySame as PreferredProvider cost share50% coinsurance perequipment/supplyafter OON plandeductible is metOther ServicesCBI/POS/Gold Tiered/IND BS (01/2022) 76962CT0040001-00 Effective Date: 1/2022Compass Gold A130348BPL CT P02157557Compass Gold Alternative POSBenefit ID: 40051Product ID: MS0400683
BenefitsPreferred ProviderIn-Network (INET)Member PaysParticipating ProviderIn-Network (INET)Member PaysOut-of-Network(OON)Member PaysHome Health Care Services(up to 100 visits per calendaryear) 25 copayment pervisitSame as PreferredProvider cost share25% coinsurance pervisit after separate 50 deductible is metOutpatient Services(in a hospital or ambulatoryfacility)20% coinsurance pervisit after INET plandeductible is met at aPreferred OutpatientHospital Facility 300 copayment pervisit at an AmbulatorySurgery Center40% coinsurance pervisit after INET plandeductible is met atan OutpatientHospital FacilitySame as PreferredProvider cost sharefor Outpatientbehavioral health,mental health andsubstance abuseservices50% coinsurance pervisit after OON plandeductible is metInpatient ServicesInpatient hospital servicesinclude mental health,substance abuse, maternity,hospice, skilled nursingfacility* and all IP settings.(*skilled nursing facility stay islimited to 90 days percalendar year)20% coinsurance peradmission after INETplan deductible ismet at a PreferredHospital Facility40% coinsurance peradmission after INETplan deductible ismetThe cost share forInpatient behavioralhealth, mental healthand substance abuseservices is the sameas Preferred Provider50% coinsurance peradmission after OONplan deductible is metEmergency and Urgent CareAmbulance Services20% coinsurance perservice after INETplan deductible ismetSame as PreferredProvider cost share20% coinsurance perservice after INETplan deductible is metEmergency Room20% coinsurance pervisit after INET plandeductible is metSame as PreferredProvider cost share20% coinsurance pervisit after INET plandeductible is metUrgent Care Centers 75 copayment pervisitSame as PreferredProvider cost share50% coinsurance pervisit after OON plandeductible is metSame as PreferredProvider cost share50% coinsurance pervisit after OON plandeductible is metPediatric Dental Care (for children under ageDiagnostic & PreventiveNo cost26)CBI/POS/Gold Tiered/IND BS (01/2022) 76962CT0040001-00 Effective Date: 1/2022Compass Gold A130348BPL CT P02157557Compass Gold Alternative POSBenefit ID: 40051Product ID: MS0400684
BenefitsPreferred ProviderIn-Network (INET)Member PaysParticipating ProviderIn-Network (INET)Member PaysOut-of-Network(OON)Member PaysBasic Services50% coinsurance pervisitSame as PreferredProvider cost share50% coinsurance pervisit after OON plandeductible is metMajor Services50% coinsurance pervisitSame as PreferredProvider cost share50% coinsurance pervisit after OON plandeductible is metOrthodontia Services(medically necessary only)50% coinsurance pervisitSame as PreferredProvider cost share50% coinsurance pervisit after OON plandeductible is metSame as PreferredProvider cost shareNot covered 50 copayment pervisitSame as PreferredProvider cost share50% coinsurance pervisit after OON plandeductible is metAdult Routine Eye Exam by aSpecialist - over age 26(one exam per calendar year) 50 copayment pervisitSame as PreferredProvider cost share50% coinsurance pervisit after OON plandeductible is metAllergy Injections(up to 20 visits per year) 20 copayment pervisitSee ParticipatingPrimary Care Provideror Specialist cost share50% coinsurance pervisit after OON plandeductible is metAllergy Testing(up to one visit per year) 20 copayment pervisitSee ParticipatingPrimary Care Provideror Specialist cost share50% coinsurance pervisit after OON plandeductible is metArtificial Limbs(includes associated supplies andequipment)20% coinsuranceSame as PreferredProvider cost share50% coinsuranceafter OON plandeductible is metPediatric Vision Care (for children under agePrescription Eye Glasses(one pair of frames and lenses orcontact lens per calendar year)Routine Eye Exam by aSpecialist(one exam per calendar year)26)Lenses: 50%coinsurance Collectionframe: 50% coinsuranceNon-collection frame:Members choosing toupgrade from acollection frame to anon-collection framewill be given a creditsubstantially equal tothe cost of thecollection frame andwill be entitled to anydiscount negotiated bythe carrier with theretailerAdditional Covered ServicesCBI/POS/Gold Tiered/IND BS (01/2022) 76962CT0040001-00 Effective Date: 1/2022Compass Gold A130348BPL CT P02157557Compass Gold Alternative POSBenefit ID: 40051Product ID: MS0400685
BenefitsPreferred ProviderIn-Network (INET)Member PaysParticipating ProviderIn-Network (INET)Member PaysOut-of-Network(OON)Member PaysOutpatient mental health,alcohol and substance abusetreatment(intensive outpatient treatmentand partial hospitalization)20% coinsurance pervisit after INET plandeductible is metSame as PreferredProvider cost share50% coinsurance pervisit after OON plandeductible is metRetail Clinic40% coinsurance pervisit after INET plandeductible is metSame as PreferredProvider cost share50% coinsurance pervisit after OON plandeductible is metCBI/POS/Gold Tiered/IND BS (01/2022) 76962CT0040001-00 Effective Date: 1/2022Compass Gold A130348BPL CT P02157557Compass Gold Alternative POSBenefit ID: 40051Product ID: MS0400686
Important information This is a brief summary of benefits. Refer to your ConnectiCare Benefits, Inc. policy for completedetails on benefits, conditions, limitations and exclusions. All benefits described are per member percalendar year. Mammogram screenings, breast ultrasounds, and breast MRIs – Please refer to the policy for details. Insulin and noninsulin drugs are covered up to a cost share maximum of 25 for each 30-day supply. Diabetes Devices and Diabetic Ketoacidosis Devices are covered up to a cost share maximum of 100per 30-day supply. Please refer to your policy for additional cost share maximums regarding diabetic services. Somediabetic services fall under preventive care and cost share may be waived. This Compass plan has a tiered network which offers you the opportunity to pay less when you visit a“Preferred” PCP or hospital. Preferred PCPs and hospitals can be found in the “Find a doctor”directory on www.connecticare.com. These providers are identified with the compass symbol. Youcan still visit other health care providers who accept your plan, they’re called “ParticipatingProviders” but you will pay more. An ambulatory surgery center is a facility that exclusively provides outpatient surgical services topatients who do not require hospitalization and whose expected stay in the center does not exceed 24hours. Ambulatory surgery centers are not owned by a hospital. An outpatient hospital facility offers surgical procedures and related care that, in the opinion of theattending physician, can be safely performed without requiring overnight inpatient hospital care.Outpatient hospital facilities are owned by a hospital or hospital system. If you have questions regarding your plan, visit our website at www.connecticare.com or call us at(860) 674-5757 or 1-800-251-7722. To learn more about your Teladoc benefits contact Teladoc at teladoc.com/connecticare or call1-800-835-2362 (TTY: 711). Out-of-Network reimbursement is based on the maximum allowable amount. Members are responsibleto pay any charges in excess of this amount. Please refer to your ConnectiCare Benefits, Inc.policy for more information. Under this program covered prescription drugs and supplies are put into categories (i.e. tiers) todesignate how they are to be covered and the member's cost-share. The placement of a drug orsupply into one of the tiers is determined by the ConnectiCare Pharmacy Services Department andapproved by the ConnectiCare Pharmacy & Therapeutics Committee based on the drugs or suppliesclinical effectiveness and cost, not on whether it is a generic drug or supply or brand name drug orsupply. Amounts paid by members because they must pay a price difference for a brand name drug do notcount towards meeting any deductible, coinsurance, copayment, coinsurance or cost share maximum. Most specialty drugs are dispensed through specialty pharmacies by mail, up to 30-day supply.Specialty Pharmacies have the same member cost share as all other participating pharmacies and arenot part of the ConnectiCare's Voluntary Mail Order program. Many services require that you obtain our Pre-Certification or Pre-Authorization prior to obtainingcare prescribed or rendered by Non-Participating providers or a benefit reduction may apply. Withoutpre-authorization you may be responsible for the total cost of the service or benefits may be reducedby the lesser of 500 or 50%. Refer to the "Pre-Authorization and Pre-Certification Addendum" inyour policy for more details. For mental health, alcohol and substance abuse services call 1-888-946-4658 to obtain PreAuthorization. In-network preventive and wellness services as defined by the United States Preventive Service TaskForce (USPSTF), including immunizations recommended by the Advisory Committee onImmunizations Practices at the Centers for Disease Control (CDC), and preventive care andscreenings supported by the Health Resources and Services Administration (HRSA) are exempt forfrom all cost shares under the Patient Protection and Affordable Care Act (PPACA). Visit our websiteat www.connecticare.com to view a list of preventive and wellness services.CBI/POS/Gold Tiered/IND BS (01/2022) 76962CT0040001-00 Effective Date: 1/2022Compass Gold A130348BPL CT P02157557Compass Gold Alternative POSBenefit ID: 40051Product ID: MS0400687
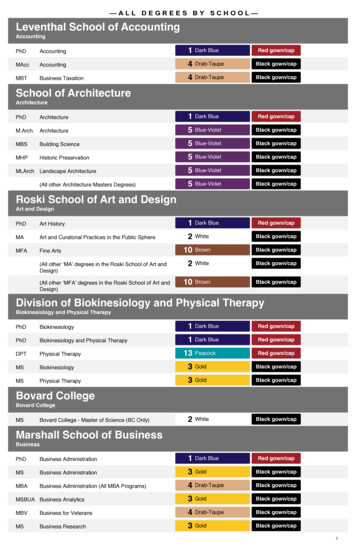
Out-of-Network (OON) Member Pays Participating Provider In-Network (INET) Member Pays Preferred Provider In-Network (INET) Member Pays CBI/POS/Gold Tiered/IND BS (01/2022) 76962CT0040001-00 Effective Date: 1/2022 Compass_Gold_A130348 BPL CT P02157557 Compass Gold Alternative POS Benefit ID: 40051 Product ID: MS040068