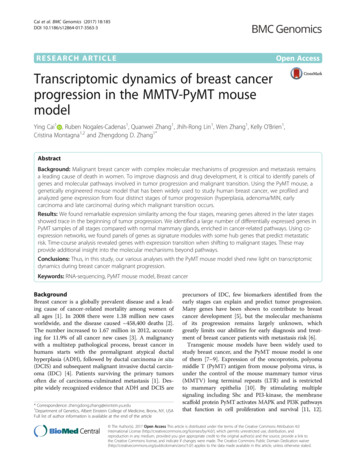
Transcription
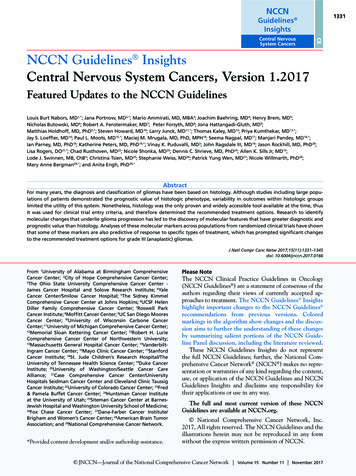
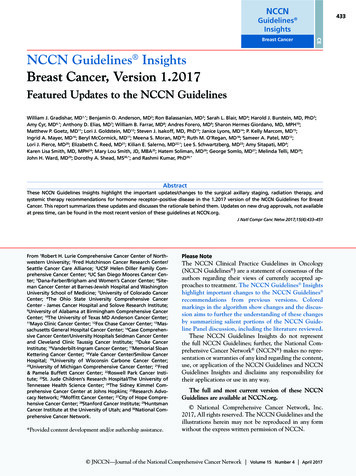
NCCN433Guidelines InsightsCEBreast CancerNCCN Guidelines InsightsBreast Cancer, Version 1.2017Featured Updates to the NCCN GuidelinesWilliam J. Gradishar, MD1,*; Benjamin O. Anderson, MD2; Ron Balassanian, MD3; Sarah L. Blair, MD4; Harold J. Burstein, MD, PhD5;Amy Cyr, MD6,*; Anthony D. Elias, MD7; William B. Farrar, MD8; Andres Forero, MD9; Sharon Hermes Giordano, MD, MPH10;Matthew P. Goetz, MD11; Lori J. Goldstein, MD12; Steven J. Isakoff, MD, PhD13; Janice Lyons, MD14; P. Kelly Marcom, MD15;Ingrid A. Mayer, MD16; Beryl McCormick, MD17; Meena S. Moran, MD18; Ruth M. O’Regan, MD18; Sameer A. Patel, MD12;Lori J. Pierce, MD20; Elizabeth C. Reed, MD21; Kilian E. Salerno, MD22,*; Lee S. Schwartzberg, MD23; Amy Sitapati, MD4;Karen Lisa Smith, MD, MPH24; Mary Lou Smith, JD, MBA25; Hatem Soliman, MD26; George Somlo, MD27; Melinda Telli, MD28;John H. Ward, MD29; Dorothy A. Shead, MS30,*; and Rashmi Kumar, PhD30,*AbstractThese NCCN Guidelines Insights highlight the important updates/changes to the surgical axillary staging, radiation therapy, andsystemic therapy recommendations for hormone receptor–positive disease in the 1.2017 version of the NCCN Guidelines for BreastCancer. This report summarizes these updates and discusses the rationale behind them. Updates on new drug approvals, not availableat press time, can be found in the most recent version of these guidelines at NCCN.org.J Natl Compr Canc Netw 2017;15(4):433–451From 1Robert H. Lurie Comprehensive Cancer Center of Northwestern University; 2Fred Hutchinson Cancer Research Center/Seattle Cancer Care Alliance; 3UCSF Helen Diller Family Comprehensive Cancer Center; 4UC San Diego Moores Cancer Center; 5Dana-Farber/Brigham and Women’s Cancer Center; 6Siteman Cancer Center at Barnes-Jewish Hospital and WashingtonUniversity School of Medicine; 7University of Colorado CancerCenter; 8The Ohio State University Comprehensive CancerCenter - James Cancer Hospital and Solove Research Institute;9University of Alabama at Birmingham Comprehensive CancerCenter; 10The University of Texas MD Anderson Cancer Center;11Mayo Clinic Cancer Center; 12Fox Chase Cancer Center; 13Massachusetts General Hospital Cancer Center; 14Case Comprehensive Cancer Center/University Hospitals Seidman Cancer Centerand Cleveland Clinic Taussig Cancer Institute; 15Duke CancerInstitute; 16Vanderbilt-Ingram Cancer Center; 17Memorial SloanKettering Cancer Center; 18Yale Cancer Center/Smilow CancerHospital; 19University of Wisconsin Carbone Cancer Center;20University of Michigan Comprehensive Cancer Center; 21Fred& Pamela Buffett Cancer Center; 22Roswell Park Cancer Institute; 23St. Jude Children’s Research Hospital/The University ofTennessee Health Science Center; 24The Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins; 25Research Advocacy Network; 26Moffitt Cancer Center; 27City of Hope Comprehensive Cancer Center; 28Stanford Cancer Institute; 29HuntsmanCancer Institute at the University of Utah; and 30National Comprehensive Cancer Network.*Provided content development and/or authorship assistance.Please NoteThe NCCN Clinical Practice Guidelines in Oncology(NCCN Guidelines ) are a statement of consensus of theauthors regarding their views of currently accepted approaches to treatment. The NCCN Guidelines Insightshighlight important changes to the NCCN Guidelines recommendations from previous versions. Coloredmarkings in the algorithm show changes and the discussion aims to further the understanding of these changesby summarizing salient portions of the NCCN Guideline Panel discussion, including the literature reviewed.These NCCN Guidelines Insights do not representthe full NCCN Guidelines; further, the National Comprehensive Cancer Network (NCCN ) makes no representation or warranties of any kind regarding the content,use, or application of the NCCN Guidelines and NCCNGuidelines Insights and disclaims any responsibility fortheir applications or use in any way.The full and most current version of these NCCNGuidelines are available at NCCN.org. National Comprehensive Cancer Network, Inc.2017, All rights reserved. The NCCN Guidelines and theillustrations herein may not be reproduced in any formwithout the express written permission of NCCN. JNCCN—JournalJNCCN—Journal ofof thethe NationalNational ComprehensiveComprehensive CancerCancer NetworkNetwork VolumeVolume 1515 NumberNumber 44 AprilApril 20172017
CE434NCCN Guidelines InsightsBreast Cancer, Version 1.2017NCCN: Continuing EducationTarget Audience: This activity is designed to meet the educational needs of physicians, nurses, and pharmacists involved inthe management of patients with cancer.NCCN designates this knowledge-based continuing educationactivity for 1.0 contact hour (0.1 CEUs) of continuing educationcredit. UAN: 0836-0000-17-004-H01-PAccreditation StatementAll clinicians completing this activity will be issued a certificateof participation. To participate in this journal CE activity: 1) review the educational content; 2) take the posttest with a 66%minimum passing score and complete the evaluation at http://education.nccn.org/node/80546; and 3) view/print certificate.Physicians: National Comprehensive Cancer Network is accreditedby the Accreditation Council for Continuing Medical Education(ACCME) to provide continuing medical education for physicians.NCCN designates this journal-based CE activity for a maximumof 1.0 AMA PRA Category 1 Credit . Physicians should claimonly the credit commensurate with the extent of their participation in the activity.Nurses: National Comprehensive Cancer Network is accreditedas a provider of continuing nursing education by the AmericanNurses Credentialing Center s Commission on Accreditation.Release date: April 10, 2017; Expiration date: April 10, 2018Learning Objectives:Upon completion of this activity, participants will be able to:NCCN designates this educational activity for a maximum of1.0 contact hour.Pharmacists: National Comprehensive Cancer Network isaccredited by the Accreditation Council for Pharmacy Education as a provider of continuing pharmacy education. Integrate into professional practice the updates to NCCNGuidelines for Breast Cancer Describe the rationale behind the decision-makingprocess for developing the NCCN Guidelines for BreastCancerDisclosure of Relevant Financial RelationshipsEditor:Kerrin M. Green, MA, Assistant Managing Editor, JNCCN—Journal of the National Comprehensive Cancer Network, has disclosed that she has no relevant financial relationships.JNCCN:Kimberly Callan, MS, Senior Director, Professional and Patient Publications, NCCN, has disclosed that she has no relevant financial relationships.Genevieve Emberger Hartzman, MA, Journal Production Specialist, NCCN, has disclosed that she has no relevant financial relationships.CE Authors:Deborah J. Moonan, RN, BSN, Director, Continuing Education, NCCN, has disclosed that she has no relevant financial relationships. (Employed by NCCNuntil 2/17/17.)Karen Kanefield, Manager, Continuing Education Accreditation and Program Operations, NCCN, has disclosed that she has no relevant financial relationships.Kathy Smith, Manager, CE Grant Writing & Project Management, NCCN, has disclosed that she has no relevant financial relationships.Kristina M. Gregory, RN, MSN, OCN, Vice President, Clinical Information Operations, NCCN, has disclosed that she has no relevant financial relationships.Rashmi Kumar, PhD, Director, Clinical Information Operations, NCCN, has disclosed that she has no relevant financial relationships.Individuals Who Provided Content Development and/or Authorship Assistance:William J. Gradishar, MD, Panel Chair, has disclosed that he has no relevant financial relationships.Amy Cyr, MD, Panel Member, has disclosed that she has no relevant financial relationships.Kilian E. Salerno, MD, Panel Member, has disclosed that she has no relevant financial relationships.Dorothy A. Shead, MS, Director, Patient & Clinical Information Operations, NCCN, has disclosed that she has no relevant financial relationships.This activity is supported by educational grants from Astellas, AstraZeneca, Celldex Therapeutics, Clovis Oncology, Genomic Health, Inc., Kyowa HakkoKirin, Jazz Pharmaceuticals, Novartis Pharmaceuticals Corporation, and NOVOCURE. This activity is supported by an independent educational grantfrom Merck Co., ehensiveComprehensiveCancerCancerNetworkNetwork VolumeVolume1515 NumberNumber44 AprilApril20172017 JNCCN—Journal
CENCCN Guidelines Insights435Breast Cancer, Version 1.2017LOCOREGIONAL TREATMENT OF CLINICAL STAGE I, IIA, OR IIB DISEASE OR T3, N1, M0kLumpectomy withsurgical axillary staging(category 1) l,m,nor 4 positiveqaxillary nodesRadiation therapy to whole breast with or without boost r to tumor bed(category 1), infraclavicular region, supraclavicular area, internal mammarynodes, and any part of the axillary bed at risk (category 1). It is common forradiation therapy to follow chemotherapy when chemotherapy is indicated.1–3 positiveaxillary nodesRadiation therapy to whole breast with or without boost r to tumor bed(category 1). Strongly consider radiation therapy to infraclavicular region,supraclavicular area, internal mammary nodes, and any part of the axillarybed at risk. It is common for radiation therapy to follow chemotherapy whenchemotherapy is indicated.Negativeaxillary nodesTotal mastectomy with surgical axillarystaging l,m,o (category 1) reconstructionporIf T2 or T3 and fulfills criteria for breastconserving therapy except for sizenSeeBINV-4Radiation therapy to whole breast with or without boost r to tumor bed, andconsider regional nodal radiation in patients with central/medial tumorsor tumors 2 cm with other high-risk features (young age or extensivelymphovascular invasion [LVSI]).orConsideration of accelerated partial breast irradiation (APBI) in selected lowrisk patients.r,sIt is common for radiation therapy to follow chemotherapy whenchemotherapy is indicated.tSee Locoregional Treatment (BINV-3)Consider Preoperative Systemic Therapy Guideline (BINV-10)kSee NCCN Guidelines for Older Adult Oncology for special treatment considerations.lSee Surgical Axillary Staging (BINV-D).mSee Axillary Lymph Node Staging (BINV-E) and Margin Status in InfiltratingCarcinoma (BINV-F).Special Considerations to Breast-Conserving Therapy Requiring RadiationTherapy (BINV-G).oExcept as outlined in the NCCN Guidelines for Genetic/Familial High-RiskAssessment: Breast and Ovarian and the NCCN Guidelines for Breast CancerRisk Reduction, prophylactic mastectomy of a breast contralateral to a knownunilateral breast cancer is discouraged. When considered, the small benefits fromcontralateral prophylactic mastectomy for women with unilateral breast cancer mustbe balanced with the risk of recurrent disease from the known ipsilateral breast cancer,nSeepsychological and social issues of bilateral mastectomy, and the risks of contralateralmastectomy. The use of a prophylactic mastectomy contralateral to a breast treatedwith breast-conserving therapy is very strongly discouraged.pSee Principles of Breast Reconstruction Following Surgery (BINV-H).qConsider imaging for systemic staging, including chest/abdominal pelvic diagnosticCT with contrast, bone scan, and optional FDG PET/CT (See BINV-1).rSee Principles of Radiation Therapy (BINV-I).sPBI may be administered prior to chemotherapy.tBreast irradiation may be omitted in patients 70 y of age with estrogen-receptorpositive, clinically node-negative, T1 tumors who receive adjuvant endocrine therapy(category 1).Version 1.2017 National Comprehensive Cancer Network, Inc. 2017, All rights reserved. The NCCN Guidelines and this illustration may not be reproduced in anyform without the express written permission of NCCN .BINV-2OverviewNCCN Categories of Evidence and ConsensusCategory 1: Based upon high-level evidence, thereis uniform NCCN consensus that the interventionis appropriate.Category 2A: Based upon lower-level evidence, thereis uniform NCCN consensus that the intervention isappropriate.Category 2B: Based upon lower-level evidence, thereis NCCN consensus that the intervention is appropriate.Category 3: Based upon any level of evidence, thereis major NCCN disagreement that the interventionis appropriate.All recommendations are category 2A unless otherwisenoted.Clinical trials: NCCN believes that the best managementfor any cancer patient is in a clinical trial. Participation inclinical trials is especially encouraged.Breast cancer is the most common malignancy inwomen in the United States and is second only tolung cancer as a cause of cancer death. The AmericanCancer Society estimates that 255,180 Americanswill be diagnosed with breast cancer and 41,070 willdie of the disease in the United States in 2017.1 Thetherapeutic options for patients with noninvasive orinvasive breast cancer are complex and varied. TheNCCN Clinical Practice Guidelines in Oncology(NCCN Guidelines) for Breast Cancer include upto-date guidelines for the clinical management of patients with carcinoma in situ, invasive breast cancer,Paget’s disease, phyllodes tumor, inflammatory breastcancer, and breast cancer during pregnancy. Theseguidelines are developed by a multidisciplinary panelof representatives from NCCN Member Institutionswith breast cancer–focused expertise in the fields ofmedical oncology, surgical oncology, radiation oncology, pathology, reconstructive surgery, and patient advocacy. JNCCN—Journal of the National Comprehensive Cancer Network Volume 15 Number 4 April 2017
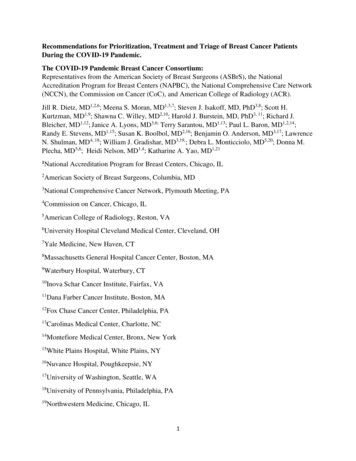
CE436NCCN Guidelines InsightsBreast Cancer, Version 1.2017LOCOREGIONAL TREATMENT OF CLINICAL STAGE I, IIA, OR IIB DISEASE OR T3, N1, M0kTotal mastectomywith surgical axillarystagingl,m (category 1) reconstructionp 4 positiveaxillary nodesqRadiation therapyr to chest wall infraclavicular region,supraclavicular area, internal mammary nodes, and anypart of the axillary bed at risk (category 1). It is commonfor radiation therapy to follow chemotherapy whenchemotherapy is indicated.1–3 positiveaxillary nodesStrongly consider radiation therapyr to chest wall infraclavicular region, supraclavicular area, internalmammary nodes, and any part of the axillary bed at risk. Itis common for radiation therapy to follow chemotherapywhen chemotherapy is indicated.Negative axillary nodesand tumor 5 cmormargins positiveConsider radiation therapyr to chest wall infraclavicularregion, supraclavicular area, internal mammary nodesand any part of the axillary bed at risk. It is commonfor radiation therapy to follow chemotherapy whenchemotherapy is indicated.Negative axillary nodes andtumor 5 cm and negativemargins but 1 mmConsider radiation therapyr to chest wall, regional nodalradiation in patients with central/medial tumors ortumors 2 cm with other high-risk features (young age orextensive LVSI).It is common for radiation therapy to follow chemotherapywhen chemotherapy is indicated.Negative axillary nodesand tumor 5 cm andmargins 1 mmNo radiation therapyukSeeNCCN Guidelines for Older Adult Oncology for special treatmentconsiderations.lSee Surgical Axillary Staging (BINV-D).mSee Axillary Lymph Node Staging (BINV-E)and Margin Status in InfiltratingCarcinoma (BINV-F).Principles of Breast Reconstruction Following Surgery (BINV-H).pSeeqConsiderimaging for systemic staging, including chest/abdominal pelvic diagnosticCT with contrast, bone scan, and optional FDG PET/CT (See BINV-1).rSee Principles of Radiation Therapy (BINV-I).uPostmastectomy radiation therapy may be considered for patients with multiple highrisk recurrence factors, including central/medial tumors or tumors 2 cm with otherhigh-risk features such as young age and/or extensive LVI.Version 1.2017 National Comprehensive Cancer Network, Inc. 2017, All rights reserved. The NCCN Guidelines and this illustration may not be reproduced in anyform without the express written permission of NCCN .In the most recent version of NCCN BreastCancer Guidelines, Version 1.2017, the NCCNpanel included updated recommendations for situations where axillary lymph node dissection (ALND)can be omitted in women with stages I, II, and IIIA(T3N1M0) breast cancer; for whole-breast radiation therapy (WBRT) using hypofractionation, updates regarding accelerated partial breast irradiation(APBI) and regional nodal irradiation (RNI) inwomen with early-stage breast cancer; and systemictherapy for women with hormone receptor–positivebreast cancer in the adjuvant and metastatic settings. The full version of these guidelines is availableonline (NCCN.org).Surgical Axillary Staging for StagesI, IIA, IIB, and IIIA (T3N1M0)ALND is the standard of care for patients withclinically positive nodes. However, ALND is associated with lymphedema and other significant mor-SeeBINV-4BINV-3bidities,2–4 and therefore sentinel lymph node biopsy(SLNB) has replaced axillary evaluation for patientswith clinically node-negative disease.Based on several randomized trials, it is now accepted that patients with a negative sentinel lymphnode (SLN) do not need an ALND.5–8The ACOSOG Z0011 trial randomized women 18 years of age with T1/T2 tumors, 3 positiveSLNs, undergoing lumpectomy and WBRT to either SLNB alone (n 436) or ALND (n 420). Inthis study, no difference was seen in local recurrence,disease-free survival (DFS), or overall survival (OS)between women with positive SLNs undergoing acompletion ALND versus no ALND. Only estrogenreceptor (ER)–negative status, age 50 years, andlack of adjuvant systemic therapy were associatedwith decreased OS.9 At a median follow-up of 6.3years, locoregional recurrences were noted in 4.1%of patients in the ALND group and 2.8% of thosein the SLNB group (P .11). Median OS was approximately 92% in each group.10 Long term follow- JNCCN—Journal of the National Comprehensive Cancer Network Volume 15 Number 4 April 2017
CENCCN Guidelines Insights437Breast Cancer, Version 1.2017SYSTEMIC ADJUVANT TREATMENT - HORMONE RECEPTOR-POSITIVE - HER2-POSITIVE DISEASEbTumor 0.5 cmincludingmicroinvasivepT1, pT2, or pT3;and pN0 or pN1mi( 2 mm axillarynode metastasis)Histology:w Ductal Lobular Mixed MetaplasticConsider adjuvant endocrine therapyx,y adjuvant chemotherapyz,aa withtrastuzumabbb,cc (category 2B)pN0pN1miAdjuvant endocrine therapyx,yorAdjuvant chemotherapyz,aawith trastuzumabbb followedby endocrine therapyx,yTumor 0.6–1.0 cmTumor 1 cmAdjuvant chemotherapyz,aa,ddwith trastuzumabbb followed byendocrine therapyx,y (category 1)Node positive (one or moremetastases 2 mm to one or moreipsilateral axillary lymph nodes)bSee Principles of HER2 Testing (BINV-A).wMixed lobular and ductal carcinoma shouldbe graded based on the ductalcomponent and treated based on this grading. For metaplastic carcinoma, theprognostic value of the histologic grading is uncertain. However, when a specifichistologic subtype of metaplastic carcinoma is present and accounts for more than10% of the tumor, the subtype is an independent prognostic variable.xConsider adjuvant bisphosphonate therapy in postmenopausal (natural or induced)patients receiving adjuvant endocrine therapy.yEvidence supports that the magnitude of benefit from surgical or radiation ovarianablation in premenopausal women with hormone receptor-positive breast cancer issimilar to that achieved with CMF alone. See Adjuvant Endocrine Therapy (BINV-J).zChemotherapy and endocrine therapy used as adjuvant therapy should be givensequentially with endocrine therapy following chemotherapy. Available datasuggest that sequential or concurrent endocrine therapy with radiation therapy isacceptable. See Adjuvant Endocrine Therapy (BINV-J) and Preoperative/AdjuvantTherapy Regimens (BINV-K).See Follow-Up(BINV-16)aaThereare limited data to make chemotherapy recommendations for those 70 y ofage. See NCCN Clinical Practice Guidelines for Older Adult Oncology.prognosis of patients with T1a and T1b tumors that are node negative isuncertain even when HER2 is amplified or overexpressed. This is a population ofbreast cancer patients that was not studied in the available randomized trials. Thedecision for use of trastuzumab therapy in this cohort of patients must balance theknown toxicities of trastuzumab, such as cardiac toxicity, and the uncertain, absolutebenefits that may exist with trastuzumab therapy.ccAdjuvant chemotherapy with weekly paclitaxel and trastuzumab (Tolaney et al.NEJM 2015) can be considered for HER2-positive T1a N0 cancers, particularly ifthe primary cancer is ER negative, and the tumor size borders on T1b ( 5 mm).The absolute benefit of HER2-based systemic chemotherapy is likely negligiblein patients with ER-positive cancers and tumor size bordering on T1mic ( 1 mm),when the estimated recurrence risk is less than 5% and endocrine therapy remainsa viable option for systemic treatment.ddA pertuzumab-containing regimen can be administered to patients with T2 or N1,HER2-positive, early-stage breast cancer.bbTheVersion 1.2017 National Comprehensive Cancer Network, Inc. 2017, All rights reserved. The NCCN Guidelines and this illustration may not be reproduced in anyform without the express written permission of NCCN .up (median, 9.25 years) results of the ACOSOGZ0011 study showed no statistically significant difference in local recurrence-free survival betweenthe groups (P .13).11 The cumulative incidence ofipsilateral axillary recurrences at 10 years was 0.5%(2 patients) in those who underwent ALND and1.5% (5 patients) in those who underwent SLNBalone (P .28).11 The 10-year cumulative incidenceof local regional recurrences was 6.2% with ALNDand 5.3% with SLNB alone (P .36).11 Results ofthe ACOSOG Z0011 trial show that ALND is notneeded in women with early-stage breast cancer whohave only 1 or 2 SLN metastases who will receiveWBRT as part of breast-conserving therapy.Another randomized trial (IBCSG 23-01) wasspecifically designed to compare outcomes in patientswith sentinel micrometastases ( 2 mm) treated withALND versus no ALND.12 Although the ACOSOGZ0011 trial was limited to those undergoing breastconserving therapy, this trial included patients undergoing mastectomy (9%).12 No differences were seen inBINV-5the group treated with ALND versus those not treated with ALND in 5-year DFS rate (84.4% [95% CI,80.7%–88.1%] vs 87.8% [95% CI, 84.4%–91.2%]);cumulative incidence of breast cancer events, including local, regional, contralateral breast, and distantrecurrence (10.8% [95% CI, 7.6–14.0] vs 10.6% [95%CI, 7.5–13.8]); or OS rate (97.6% [95% CI, 96.0%–99.2%] vs 97.5% [95% CI, 95.8%–99.1%]).12 Regional recurrence was 1% for those who underwentALND and 1% for those who did not.12 Results of thistrial show that in patients with only micrometastasesin the SLNs, ALND is not needed.The results of a trial by the European EORTCgroup (AMAROS) assessed whether axillary radiation therapy (RT) provides regional control withfewer side effects compared with ALND.13 Thistrial included patients (n 4,823) with T1 or T2breast cancer and positive SLNs (micrometastaticor macrometastatic), and included a small fractionof patients (n 248) treated with mastectomy.13 Theresults reported no difference in 5-year OS or DFS for JNCCN—Journal of the National Comprehensive Cancer Network Volume 15 Number 4 April 2017
CE438NCCN Guidelines InsightsBreast Cancer, Version 1.2017SYSTEMIC ADJUVANT TREATMENT - HORMONE RECEPTOR-POSITIVE - HER2-NEGATIVE DISEASEbTumor 0.5 cmincludingmicroinvasiveConsider adjuvant endocrine therapyx,y (category 2B)Adjuvant endocrine therapyx,y (category 2B) orAdjuvant chemotherapyz,aa followed by endocrinetherapyx,y (category 2B)pN0pN1mipT1, pT2, or pT3;and pN0 or pN1mi( 2 mm axillarynode metastasis)Histology:w Ductal Lobular Mixed MetaplasticNot done Tumor 0.5 cmNode positive (one or moremetastases 2 mm to one or moreipsilateral axillary lymph nodes)eeAdjuvant endocrine therapy orAdjuvant chemotherapyz,aa followedby endocrine therapyx,y (category 1)Lowrecurrencescore ( ncescore (18–30)Highrecurrencescore ( 31)Adjuvant endocrine therapyx,ySeeFollow-Up(BINV-16)Adjuvant endocrine therapy orAdjuvant chemotherapyz,aafollowed by endocrinetherapyx,yAdjuvant endocrine therapyx,y adjuvant chemotherapyz,aaAdjuvant endocrine therapyx,y adjuvant chemotherapyz,aa (category 1)zChemotherapybSee Principles of HER2 Testing (BINV-A).wMixed lobular and ductal carcinoma, shouldbe graded based on the ductalcomponent and treated based on this grading. For metaplastic carcinoma, theprognostic value of the histologic grading is uncertain. However, when a specifichistologic subtype of metaplastic carcinoma is present and accounts for more than10% of the tumor, the subtype is an independent prognostic variable.xConsider adjuvant bisphosphonate therapy in postmenopausal (natural or induced)patients receiving adjuvant endocrine therapy.yEvidence supports that the magnitude of benefit from surgical or radiation ovarianablation in premenopausal women with hormone receptor-positive breast cancer issimilar to that achieved with CMF alone. See Adjuvant Endocrine Therapy (BINV-J).and endocrine therapy used as adjuvant therapy should be givensequentially with endocrine therapy following chemotherapy. Available datasuggest that sequential or concurrent endocrine therapy with radiation therapy isacceptable. See Adjuvant Endocrine Therapy (BINV-J) and Preoperative/AdjuvantTherapy Regimens (BINV-K).aaThere are limited data to make chemotherapy recommendations for those 70 yof age. See NCCN Clinical Practice Guidelines for Older Adult Oncology.eeThe 21-gene RT-PCR assay recurrence score can be considered in selectpatients with 1–3 involved ipsilateral axillary lymph nodes to guide the additionof combination chemotherapy to standard hormone therapy. A retrospectiveanalysis of a prospective randomized trial suggests that the test is predictive inthis group similar to its performance in node-negative disease.ffOther prognostic multigene assays may be considered to help assess risk ofrecurrence but have not been validated to predict response to chemotherapy.Version 1.2017 National Comprehensive Cancer Network, Inc. 2017, All rights reserved. The NCCN Guidelines and this illustration may not be reproduced in anyform without the express written permission of NCCN .patients randomized to ALND versus axillary RT.13The 5-year DFS was 86.9% (95% CI, 84.1–89.3) inthe ALND group and 82.7% (95% CI, 79.3–85.5)in the axillary RT group. The 5-year OS was 93.3%(95% CI, 91.0–95.0) in the ALND group and 92.5%(95% CI, 90.0–94.4) in the axillary RT group.13 Atthe end of 5 years, lymphedema was less frequent inthe group treated with axillary RT versus ALND (11%vs 23%).13 The results of this trial show that axillaryRT is an acceptable alternative to ALND for axillarycontrol in patients found to have positive SLNs, withsignificantly less lymphedema-related morbidity.NCCN RecommendationsIn patients with clinically positive nodes, to determine whether ALND is needed, the panel recommends pathologic confirmation of malignancy usingultrasound-guided fine-needle aspiration (FNA)14 orcore biopsy of suspicious nodes. According to theNCCN panel, the recommendation for axillary dissection of level I and II nodes is limited to patientsBINV-6with biopsy-proven axillary metastases. Traditionallevel I and II ALND requires that 10 lymph nodesbe provided for pathologic evaluation to accuratelystage the axilla.15,16 ALND should be extended toinclude level III nodes only if gross disease is apparent in the level II and III nodes. In the absence ofgross disease in level II nodes, lymph node dissection should include tissue inferior to the axillaryvein from the latissimus dorsi muscle laterally to themedial border of the pectoralis minor muscle (level Iand II) (see BINV-D; page 440).If axillary lymph nodes are clinically negativeat diagnosis or if FNA/core biopsy results of suspicious nodes are negative, the panel recommendsSLN mapping and excision. SLNs can be assessedfor the presence of metastases by both hematoxylineosin (H&E) staining and cytokeratin immunohistochemistry (IHC). The clinical significance of alymph node that is negative on H&E staining butpositive on cytokeratin IHC is not clear. Because thehistorical and clinical trial data on which treatment JNCCN—Journal of the National Comprehensive Cancer Network Volume 15 Number 4 April 2017
CENCCN Guidelines Insights439Breast Cancer, Version 1.2017SYSTEMIC ADJUVANT TREATMENT - FAVORABLE HISTOLOGIESpT1, pT2, or pT3;and pN0 or pN1mi( 2 mm axillarynode metastasis)ER-positiveand/orPR-positive 1 cmConsider adjuvant endocrinetherapyx for risk reduction1–2.9 cmConsider adjuvant endocrinetherapyx,y 3 cmAdjuvant endocrine therapyx,yNode positive (one or moremetastases 2 mm to one or moreipsilateral axillary lymph nodes)Histology: Tubular MucinousER-negativeandPR-negativeAdjuvant endocrine therapyx,y See Follow-Up adjuvant chemotherapyz,aa (BINV-16)ER-positiveand/orPR-positiveFollow appropriatepathway aboveER-negativeandPR-negativeTreat as usual breast cancerhistology(See BINV-7 and BINV-8)Repeat determinationof ER/PR statusxConsideradjuvant bisphosphonate therapy in postmenopausal (natural or induced)patients receiving adjuvant endocrine therapy.supports that the magnitude of benefit from surgical or radiation ovarianablation in premenopausal women with hormone receptor-positive breast cancer issimilar to that achieved with CMF alone. See Adjuvant Endocrine Therapy (BINV-J).zChemotherapy and endocrine therapy used as adjuvant therapy should be givensequentially with endocrine therapy following chemotherapy. Available datayEvidencesuggest that sequential or concurrent endocrine therapy with radiation therapy isacceptable. See Adjuvant Endocrine Therapy (BINV-J) and Preoperative/AdjuvantTherapy Regimens (BINV-K).aaThere are limited data to make chemotherapy
tute; 23St. Jude Children's Research Hospital/The University of Tennessee Health Science Center; 24The Sidney Kimmel Com-prehensive Cancer Center at Johns Hopkins; 25Research Advo-cacy Network; 26Moffitt Cancer Center; 27City of Hope Compre-hensive Cancer Center; 28Stanford Cancer Institute; 29Huntsman