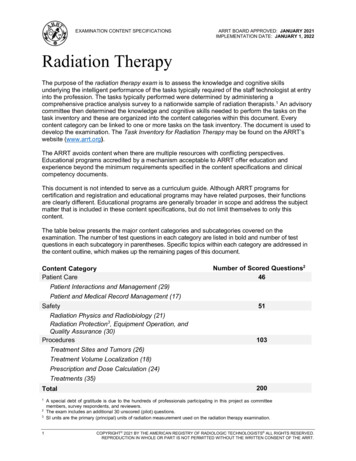
Transcription
CLINICAL GUIDELINESRadiation TherapyVersion 1.0.2019Effective March 1, 2019Clinical guidelines for medical necessity review of radiation therapy services. 2019 eviCore healthcare. All rights reserved.
Radiation Therapy CriteriaV1.0.2019Please note the following:CPT Copyright 2017 American Medical Association. All rights reserved.CPT is a registered trademark of the American Medical Association. 2019 eviCore healthcare. All Rights Reserved.Page 2 of 272400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924www.eviCore.com
Radiation Therapy CriteriaV1.0.2019Please note the following:All information provided by the NCCN is “Referenced with permission from the NCCNClinical Practice Guidelines in Oncology (NCCN Guidelines ) 2017/2018 NationalComprehensive Cancer Network. The NCCN Guidelines and illustrations herein maynot be reproduced in any form for any purpose without the express written permission ofthe NCCN. To view the most recent and complete version of the NCCN Guidelines, goonline to NCCN.org.” 2019 eviCore healthcare. All Rights Reserved.Page 3 of 272400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924www.eviCore.com
Radiation Therapy CriteriaV1.0.2019Dear Provider,This document provides detailed descriptions of eviCore’s basic criteria (also known asclinical guidelines) for radiation therapy arranged by diagnosis. They have beencarefully researched and are continually updated in order to be consistent with the mostcurrent evidence-based guidelines and recommendations for the provision of radiationtherapy from national medical societies and evidence-based medicine research centers.In addition, the criteria are supplemented by information published in peer-reviewedliterature.Our health plan clients review the development and application of these criteria. EveryeviCore health plan client develops a unique list of CPT codes or diagnoses that arepart of their radiation therapy utilization management programs. Health Plan medicalpolicy supersedes the eviCore criteria when there is conflict with the eviCore criteria andthe health plan medical policy. If you are unsure of whether or not a specific health planhas made modifications to these basic criteria in their medical policy for RadiationTherapy please contact the plan or access the plan’s website for additional information.While eviCore encourages participation in clinical trials when consistent with eachhealth plan’s policies, we want to clarify our position on the use of such standard armsoutside of the research setting. The use of a control arm or standard arm in a Phase IIIclinical trial does not necessarily mean that other standard treatment techniques are notequally effective. Examples of multiple “standard” arms can easily be found in thetreatment of prostate cancer where Intensity-Modulated Radiation Therapy (IMRT), 3Dimensional (3-D), low dose implant or High Dose Rate (HDR) can be equally effectiveor breast cancer where standard whole breast fractionation or hypo-fractionation can beused. Indeed, national criteria such as National Comprehensive Cancer Network(NCCN) and American College of Radiology (ACR) Appropriateness Criteria oftensuggest more than one radiation technique.It is eviCore’s process to apply evidence-based criteria to the particular clinicalcharacteristics in evaluating a case, and to certify the most appropriateregimen/modality. This regimen/modality may match one that is used as a “standardarm” in a federally funded clinical trial, or it may be one that is considered an “alternatestandard”. The alternate standard will be one supported by nationally publishedguidelines such as the NCCN, ACR Appropriateness Guidelines, or American Society 2019 eviCore healthcare. All Rights Reserved.Page 4 of 272400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924www.eviCore.com
Radiation Therapy CriteriaV1.0.2019for Radiation Oncology (ASTRO) Evidence-Based Guidelines, or supported by otheracceptable peer-reviewed publications.As such, eviCore will not automatically certify a case based solely on the fact that itmatches the standard (control) arm of a clinical trial. This concept applies also toregimens/modalities listed by the NCCN or ACR as “acceptable” treatments for specificdisease sites. Rather, we commit to working with the providing Radiation Oncologist tocertify the most appropriate regimen/modality for a particular case.eviCore healthcare works hard to make your clinical review experience a pleasant one.For that reason, we have peer reviewers available to assist you should you havespecific questions about a procedure.For your convenience, eviCore’s Customer Service support is available from 7 a.m. to 7p.m. Our toll free number is (800) 918-8924.Gregg P. Allen, M.D. FAAFPEVP and Chief Medical Officer 2019 eviCore healthcare. All Rights Reserved.Page 5 of 272400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924www.eviCore.com
Radiation Therapy CriteriaV1.0.2019Table of ContentsBrachytherapy of the Coronary Arteries . 7Hyperthermia . 16Image-Guided Radiation Therapy (IGRT) . 19Neutron Beam Therapy . 23Proton Beam Therapy . 25Radiation Therapy for Anal Canal Cancer. 68Radiation Therapy for Bladder Cancer . 71Radiation Therapy for Bone Metastases . 75Radiation Therapy for Brain Metastases . 80Radiation Therapy for Breast Cancer . 88Radiation Therapy for Cervical Cancer . 98Radiation Therapy for Endometrial Cancer . 105Radiation Therapy for Esophageal Cancer . 112Radiation Therapy for Gastric Cancer . 117Radiation Therapy for Head and Neck Cancer . 120Radiation Therapy for Hepatobiliary Cancer . 124Radiation Therapy for Hodgkin’s Lymphoma . 130Radiation Therapy for Kidney and Adrenal Cancer . 134Radiation Therapy for Lung Cancer . 136Radiation Therapy for Multiple Myeloma and Solitary Plasmacytomas . 149Radiation Therapy for Non-Hodgkin’s Lymphoma . 152Radiation Therapy for Non-malignant Disease. 158Radiation Therapy for Oligometastases. 185Radiation Therapy for Other Cancers . 191Radiation Therapy for Pancreatic Cancer . 192Radiation Therapy for Primary Craniospinal Tumors and Neurologic Conditions. 198Radiation Therapy for Prostate Cancer . 206Radiation Therapy for Rectal Cancer . 213Radiation Therapy for Skin Cancer . 216Radiation Therapy for Soft Tissue Sarcomas . 224Radiation Therapy for Testicular Cancer . 231Radiation Therapy for Thymoma and Thymic Cancer . 234Radiation Therapy for Urethral Cancer and Upper Genitourinary Tract Tumors 238Radiation Treatment with Azedra (iobenguane I-131) . 240Radiation Treatment with Lutathera (Lutetium; Lu 177 dotatate) . 243Radioimmunotherapy with Zevalin . 248Selective Internal Radiation Therapy (SIRT) . 261Revision History . 268 2019 eviCore healthcare. All Rights Reserved.Page 6 of 272400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924www.eviCore.com
Radiation Therapy CriteriaV1.0.2019Brachytherapy of the Coronary ArteriesPOLICYI.Coronary artery brachytherapyA. Is medically necessary when used as an adjunct to percutaneous coronaryintervention (PCI) for treatment of in-stent restenosis in a native coronary arterybare-metal stent or saphenous vein graft (SVG)B. Intravascular brachytherapy (VBT) is considered medically necessary forrecurrent drug-eluting stent in-stent restenosisC. All other indications are not covered because they are consideredexperimental, investigational, or unproven (EIU)Key Clinical PointsRevascularization of obstructed arteries due to coronary artery disease (CAD) may beaccomplished by PCI with balloon angioplasty, a minimally-invasive procedure in whicha catheter with an inflatable balloon at the tip is inserted into the lumen of the artery andinflated, dilating the area of blockage. Coronary stents are implanted in most patientsduring PCI, resulting in lower rates of restenosis compared to balloon angioplasty alone.Several drug-eluting stents (DES) have been developed to minimize the incidence ofrestenosis, and represent approximately 70 to 90% of stent implantations. The choice ofstent (bare-metal vs. drug-eluting) depends on various factors, including lesion locationand morphology, patient characteristics, and the patient’s ability to adhere to the extendedperiod of dual antiplatelet therapy required for DES. In-stent restenosis continues to be asignificant problem with bare-metal stents and is thought to be caused by neointimalhyperplasia within the stent. Several mechanical treatments of in-stent restenosis wereattempted, including balloon re-dilitation, removal of in-stent hyperplasia by atherectomy,and repeated bare-metal stenting. Brachytherapy was introduced as a method to treat instent restenosis by the delivery of gamma or beta radiotherapy via a catheter-basedsystem. Brachytherapy affects the proliferation of smooth muscle cells that areresponsible for restenosis, and may be used to treat in-stent restenosis of native coronaryarteries and SVGs. The role of brachytherapy has diminished, however, and DES haveemerged as the preferred method of treatment for in-stent restenosis. Brachytherapy mayplay a role in treatment of selected patients, however.Three brachytherapy devices received U.S. Food and Drug Administration (FDA)premarket approval (PMA). The Novoste Beta-Cath System (Novoste Corp., Norcross,GA) and the GALILEO Intravascular Radiotherapy System (Guidant Corp., Houston, TX)deliver beta radiation, while the Cordis Checkmate System (Cordis Corp., Miami, FL)delivers gamma radiation. Each operates in a similar fashion. A delivery catheter is placedin the coronary artery at the site of in-stent restenosis and a transfer device is connectedto the catheter, delivering the radioactive seeds to administer radiation to the artery. Aftera specified period of time, the radioactive seeds are returned to the transfer device and 2019 eviCore healthcare. All Rights Reserved.Page 7 of 272400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924www.eviCore.com
Radiation Therapy CriteriaV1.0.2019removed. Although significant data was collected through the use of all of these devices,both the Checkmate and GALILEO systems have been discontinued by theirrespective manufacturers (2007) as DES are now most frequently used. The Beta-Cath System is now distributed by Best Vascular, Inc.Literature ReviewI.In-stent restenosis of native coronary arteries and SVGsA. Several early multicenter trials of brachytherapy demonstrated the treatmentbenefits of intracoronary radiation for the treatment of in-stent restenosis:1. INitial Hyperplasia Inhibition with Beta In-stent Trial [INHIBIT], Waksman etal. (2002)2. STents And Radiation Therapy [START], Popma et al. (2002)3. GAMMA-1 trial, Leon, et al. (2001)4. Coronary Radiation to Inhibit Proliferation Post Stenting [SCRIPPS],Teirstein, et al. (1997)B. Ellis et al., for the TAXUS V ISR Investigators (2008), conducted a randomizedstudy to evaluate two-year outcomes of treatment with a paclitaxel-eluting stent(PES) (n 195) or brachytherapy (n 201) in patients referred for PCI for baremetal stent in-stent restenosis. Between 9 and 24 months, ischemia-driventarget lesion revascularization (TLR) tended to be required less in the PESgroup compared to the brachytherapy group (5.3. vs. 10.3%, p 0.07). At 24months, ischemia-driven TLR and ischemia-driven target vesselrevascularization (TVR) were significantly reduced in the PES group comparedto the brachytherapy group (10.1 vs. 21.6%, p 0.003, and 18.1 vs. 27.5%,p 0.03, respectively).There were no significant differences between the twogroups in death, myocardial infarction, or target vessel thrombosis between 12and 24 months, or cumulative to 24 months.C. Holmes et al., for the SISR Investigators (2008) conducted a randomized trialto evaluate the safety and efficacy of sirolimus-eluting stents (SES) (n 259)compared to vascular brachytherapy (VBT) (n 125) for treatment of in-stentrestenosis in a bare-metal stent. At three years, survival free from TLR or TVRwas significantly improved with SES; freedom from TLR was 81.0% for SESvs. 71.6% for brachytherapy, p 0.018; TVR was 78.2% for SES vs. 68.8% forbrachytherapy, p 0.022. Target vessel failure and major adverse cardiacevents (MACE) were improved with SES but did not reach statisticalsignificance. There was no statistically significant difference in definite orprobable stent thrombosis between the two groups. Five-year follow-up of theSISR trial was published by Alli et al. in 2012. There were no differences insafety or efficacy outcomes for treatment of BMS restenosis with SES vs. VBT. 2019 eviCore healthcare. All Rights Reserved.Page 8 of 272400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924www.eviCore.comBrachytherapy of the Coronary Arteries5. Washington Radiation for In-Stent Restenosis Trial [WRIST], Ajani et al.(2002)
Radiation Therapy CriteriaV1.0.2019There were no significant differences in survival free from TLR, TVR, or majoradverse cardiac events between the two groups.E. The three devices described above received FDA approval for in-stentrestenosis in native coronary arteries, and most published studies havefocused on this indication. Brachytherapy has also been used to successfullytreat in-stent restenosis in SVGs. The SVG-WRIST trial (Waksman, et al.,2002), a randomized, double-blind, placebo-controlled trial, evaluated theeffect of intravascular gamma radiation in 120 patients with in-stent restenosisin saphenous vein grafts. Patients underwent balloon angioplasty,atherectomy, additional stenting or a combination of these procedures. If theintervention was successful, patients were randomly assigned in a double-blindfashion to intravascular treatment with a ribbon containing iridium-192 (n 60)or nonradioactive seeds (n 60). Revascularization and radiation therapy weresuccessful in all patients. At six months, the restenosis rate was lower in theiridium-192 group (21%) than in the placebo group (44%). At 12 months,revascularization of the target lesion was lower in the iridium-192 group (17%)than in the placebo group (57%). The rate of major cardiac events at 12 monthswas also lower in the iridium-192 group (32%) than the placebo group (63%).F. Rha et al. (2005) published a follow-up to the SVG-WRIST trial to determinewhether the safety and efficacy of brachytherapy is durable. At 36 months, TLR,repeat percutaneous transluminal coronary angioplasty (PTCA) and TLR-majoradverse cardiac events (MACE) remained significantly lower in the irradiatedgroup, although TVR and TVR-MACE did not. The beneficial effect and efficacyof irradiation declined with time and manifested with late recurrences. Theauthors stated that saphenous vein grafts are known to degenerate over time,and when PCI is required, the clinical outcome of these patients is markedlyimpaired. The outcomes of patients in the SVG-WRIST trial are driven,therefore, by the restenotic process, with a high likelihood that graft failure wasa result of progression of degenerative disease within the graft or within thenative coronary arteries distal to the graft. The authors concluded that patientsin the SVG-WRIST trial treated with brachytherapy had a marked reduction in 2019 eviCore healthcare. All Rights Reserved.Page 9 of 272400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924www.eviCore.comBrachytherapy of the Coronary ArteriesD. Drug-eluting stents were compared to beta-radiation for the treatment of instent restenosis in a case series conducted by Zavalloni et al. (2006). The first68 patients (group I) were treated with brachytherapy using the Novoste BetaCath system. The latter 73 patients (group II) were treated with a Cypher sirolimus-eluting stent or a Taxus paclitaxel-eluting stent. Nine monthsfollowing treatment, restenosis rates were 37.8% (28/74) for patients in group Iand 14.9% (11/74) for patients in group II (p 0.0028). A diffuse pattern ofrecurrence was more frequently seen after brachytherapy (20/74 vs. 6/74,p 0.005). The “edge effect” following brachytherapy was associated withworse outcomes and accounted for most failures. Recurrence within theoriginal restenotic stent was similar in both groups (12.9% vs. 14.9%, p .8).Patients treated with drug-eluting stents for diffuse in-stent restenosisexperienced more favorable clinical and angiographic outcomes compared toa similar cohort of patients treated with beta-brachytherapy.
Radiation Therapy CriteriaV1.0.2019the need for repeat TLR at 36 months, with sustained clinical benefit at threeyears despite late recurrences, which were more pronounced in the irradiatedgroup.II.Meta-analysesB. Oliver et al. (2008) conducted a meta-analysis of randomized trials assessingthe outcome of brachytherapy or DES for the treatment of in-stent restenosis.The analysis included 14 studies/3103 patients. Neither treatment had anyeffect on mortality or rate of myocardial infarction. At intermediate follow-up,brachytherapy reduced the rate of revascularization, binary restenosis, and lateloss compared to balloon angioplasty and selective bare-metal stents alone.MACE rates were lower in patients treated with brachytherapy at bothintermediate and long-term follow-up. DES reduced the rate ofrevascularization, MACE, and binary restenosis compared to brachytherapy,but follow-up was limited to nine months. The authors concluded that vascularbrachytherapy improves the long-term outcome of angioplasty compared withbare-metal stents alone in the treatment of in-stent restenosis, and DES appearto provide similar results during short-term follow-up.C. Uchida et al. (2006) conducted a meta-analysis of randomized controlled trialscomparing intracoronary gamma- and beta-radiation therapy to placebo for instent restenosis. The authors assessed the comparative effectiveness ofbrachytherapy and the two radiation sources. They also evaluated theperformance of the procedure in native coronary arteries and SVG. Fiverandomized controlled trials that compared brachytherapy to placebo in 1310patients were reviewed. There was considerable between-study variance, anddiabetes was found to be a significant factor in this variance. In multivariatemeta-regression analyses adjusted for diabetes and lesion length, neithergamma radiation source nor SVG was a significant factor for the between-studyvariance (p 0.675 and 0.433, respectively). Neither gamma radiation in SVGnor difference in radiation source (beta or gamma) in native coronary arterieswas a significant factor in brachytherapy effectiveness compared to placebo.Intracoronary brachytherapy was effective compared to placebo at mid-termfollow up. 2019 eviCore healthcare. All Rights Reserved.Page 10 of 272400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924www.eviCore.comBrachytherapy of the Coronary ArteriesA. A meta-analysis by Lu et al. (2012) was conducted to determine whether DESimplantation remains favorable in large sample size and long-term follow-upwhen compared to intracoronary brachytherapy (ICBT) in patients with in-stentrestenosis. The analysis included 1942 patients in twelve controlled trials (fourrandomized controlled and eight nonrandomized controlled trials). DES weresignificantly more effective in reducing TVR (p 0.009) and binary restenosis(p 0.00001) compared to ICBT at a midterm follow-up of six to twelve months.There were no significant differences in cardiac death, MI, and late stentthrombosis at midterm follow-up. At a follow-up of 24 to 36 months, therecontinued to be no significant difference in cardiac death (p 0.59) or MI(p 0.65), although a statistically significant difference was found in TVR(p 0.005) in favor of DES.
Radiation Therapy CriteriaV1.0.2019D. Additional proposed indications include:1. Intracoronary brachytherapy has been proposed as a treatment for newstenosis of native coronary arteries and SVG, as well as restenosis of nativecoronary arteries and SVG at the unstented site of a previous PCI2. Brachytherapy has also been evaluated as a method of primary preventionof restenosis after stent implantation for de novo lesionsE. In the BetAce randomized trial, Ribichini et al. (2006) evaluated brachytherapyfor prevention of in-stent restenosis after angioplasty of de novo lesions inpatients with high plasma angiotensin converting enzyme (ACE). Elevatedplasma ACE levels have been proposed to increase the risk of in-stentrestenosis. Thirty-one patients (33 stenoses) were randomized to stentimplantation (control group), and 30 patients (31 stenoses) were randomizedto brachytherapy and stented angioplasty. Following angioplasty, in-stentminimal lumen diameter (MLD) was similar in both groups. At 6 months, MLDhad decreased in the control group to 1.74 0.8 mm, compared to 2.25 1.05mm in the brachytherapy group. The mean in-stent diameter was 2.3 0.8 mmin the control group vs. 2.9 1.05 mm in the brachytherapy group, and therestenosis rate was 37.5% in the control group vs. 17.9% in the brachytherapygroup. At six months, a higher need for TVR was seen in the control group(35.5%) than in the brachytherapy group (13.3%). The authors concluded thatthis study confirms that patients with high plasma ACE levels are exposed toan increased risk for in-stent restenosis and that the preventive use ofbrachytherapy in these patients reduced neointimal formation and increasedMLD.F. Ferrero et al. (2007) reported five-year follow-up of the BetAce trial, analyzingthe incidence of death, MI, and ischemia-driven TVR. The incidence of stentthrombosis was slightly higher in the brachytherapy group (10%) than in thecontrol group (6.5%). This difference was not statistically significant. Althoughthere was a significantly higher need for TVR in the control group at six months,the difference lost its significance at 12 months and five years because of a latecatch-up phenomenon in the brachytherapy group, with a higher incidence ofedge stenosis and stent occlusion. Five-year event-free survival rank for death,MI and TVR was 43% in the brachytherapy group compared to 45% in the 2019 eviCore healthcare. All Rights Reserved.Page 11 of 272400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924www.eviCore.comBrachytherapy of the Coronary Arteries3. VBT may be used for recurrent DES in-stent restenosis. Recent studieshave shown that VBT is safe with low recurrence rates at one year postprocedure. It is considered to be a safe short-term method of restoringpatency although repeat intervention will be eventually medicallynecessary. In a study of 186 patients with 283 lesions, Negi et al (2016),unstable angina was treated with balloon angioplasty followed by VBT. In99% of cases treatment was delivered without adverse effects. Similarly,Ohri et al. (2016), reported on 134 patients with 141 treated lesions as wellas a control group of 37 patients. This study confirmed the safety andusefulness of the procedure in a high risk population. Additionalinvestigation was recommended
Radiation Therapy CriteriaV1.0.2019control group (p 0.95). The occurrence of additional ischemic events in bothgroups equalized the long-term clinical outcomes. The authors stated thatintracoronary beta radiation at the time of stent implantation only transientlyprevents excessive neointimal proliferation that leads to stenosis recurrence inthe first year after treatment. The late catch-up phenomenon, along with thenatural progression of the atherosclerotic disease in other segments, isresponsible for the loss of the clinical benefit of brachytherapy in the long term.III.Professional societies/organizationsA. A guideline update for PCI published by the American College of Cardiology(ACC), American Heart Association (AHA) and the Society for CardiovascularAngiography and Interventions (SCAI) (Smith et al., 2005) states that vascularbrachytherapy has been successful in treating restenosis occurring withinstents, while other adjunctive therapies, such as the cutting balloon, rotaryablation, excimer laser and restenting have shown mixed results. TheACC/AHA/SCAI guideline states that brachytherapy can be useful as a safeand effective treatment for in stent restenosis (Class IIa recommendation). AClass IIa recommendation indicates that there is conflicting evidence and/or adivergence of opinion about the usefulness/efficacy of a procedure or treatmentbut that the weight of evidence is in favor of usefulness/efficacy. No changesto this recommendation were made in focused updates to the PCI guidelinepublished in 2007 and 2009.B. A 2011 American College of Cardiology Foundation (ACCF)/American HeartAssociation (AHA)/Society for Cardiovascular Angiography and Interventions(SCAI) PCI guideline (Wijns et al.) does not include recommendations forbrachytherapy. The background of the guideline references studiesdemonstrating superiority of DES over brachytherapy. 2019 eviCore healthcare. All Rights Reserved.Page 12 of 272400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924www.eviCore.comBrachytherapy of the Coronary ArteriesG. Syeda et al. (2006) conducted a double-blind, randomized trial of betabrachytherapy for prevention of restenosis after stent implantation in nativecoronary de novo lesions. Eighty-nine diabetic patients (106 lesions) wererandomly assigned to treatment with beta radiation or placebo treatment.Angiographic analysis at nine months demonstrated a late lumen loss of 0.7 0.9 mm in the brachytherapy group vs. 1.2 0.8 mm in the control group at theinjured segment, 0.9 1.0 vs. 1.3 0.7 mm at the radiated segment, and 0.9 1.0 vs. 1.3 0.7 mm at the target segment. Binary restenosis rates weresignificantly lower in the brachytherapy group in all subsegments. TVR forrestenosis was necessary in nine lesions (17.6%) in the brachytherapy groupvs. 18 (34%) in the placebo group. Late thrombosis occurred in fourbrachytherapy patients after premature discontinuation of antiplatelet therapy,resulting in a MACE rate of 37.2%, compared to 38.6% in the placebo group.The authors concluded that, in diabetic patients with de novo coronary lesions,intracoronary radiation after stent implantation significantly reduced restenosis.This clinical benefit was reduced, however, by the frequent occurrence of newthrombosis.
Radiation Therapy CriteriaV1.0.2019C. Guidelines for PCI issued by the European Society of Cardiology (ESC) statethat brachytherapy proved to be the only evidence-based nonsurgicaltreatment for in-stent restenosis. The guideline also states that a prolongedintake of clopidogrel for one year after radiation is necessary. The ESCguideline recommends brachytherapy for the treatment of in-stent restenosis innative coronary arteries as a Class 1A recommendation. Brachytherapy fortreatment of in-stent restenosis of a saphenous vein bypass graft is consideredas a Class 1B recommendation. Class I indicates evidence and/or generalagreement that a given diagnostic procedure/treatment is beneficial, useful andeffective. Level of evidence A indicates that data is derived from multiplerandomized clinical trials or meta-analyses, while level of evidence B indicatesdata is derived from a single randomized clinical trial or large non-randomizedstudies (Silber et al., 2005).D. Guidelines on Myocardial Revascularization developed by The Task Force onMyocardial Revascularization of the European Society of Cardiology (ESC) andthe European Association for Cardio-Thoracic Surgery (EACTS) state thatcurrently, intracoronary brachytherapy is of very limited us
Please note the following: All information provided by the NCCN is "Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines ) 2017/2018 National Comprehensive Cancer Network.