Transcription
A publication for alumni, students, faculty and friends of Mayo Clinic School of Health SciencesAnnual Meetingpreview: Clarityon concussionsClaire Bender, MD,a Champion ofAllied HealthDELSINCARTERGlobe-trotter forMayo Medical Laboratories2 017 ConnectionsSPRINGMayo Clinic School of Health Sciences
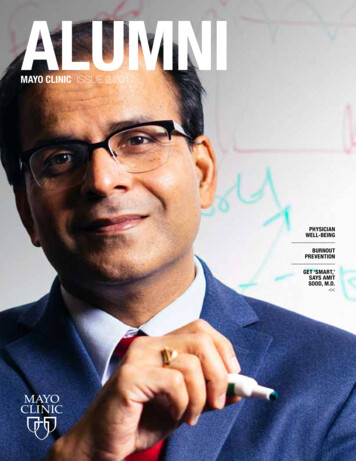
ALUMNI ASSOCIATION ANNUAL MEETING APRIL 21Hear and share fascinating storiesFascinating. Exciting. Funny.Sensitive. Dedicated. Smart.Those are just a few of thedescriptors that came to mindwhen I read the stories aboutalumni in this issue of Connections.Really, you have to read them. Nori Brice, a cardiology nursepractitioner, is on a mission toraise awareness about hearthealth in her Native Americancommunity. Delsin Carter, a graduate ofthe Phlebotomy Program, isbringing leading-edge medicaltesting to distant corners of theworld as a representative forMayo Medical Laboratories. Ryan Sura, a pediatricrespiratory therapist, breatheslife into the fragile bodies ofcritically ill and injured childrenduring medical transport. Joe Swicklik, CT technologist/magician, pulls out his tricks tomake medical care less scaryfor children. Claire Bender, MD, PhysicalTherapy Program alumna, isthe first recipient of the AlumniAssociation’s new Championof Allied Health Award.A radiologist, Dr. Benderdeveloped the Mayo ClinicSchool of Health Sciences(MCSHS) RadiographyProgram and was schooldean for 12 years. She playeda pivotal role in establishinga University of Minnesotacampus in Rochester andin developing a Bachelor ofScience in Health Professionsdegree at the university.Of course, this is just a handfulof alumni doing amazing things.There are thousands of examplesof MCSHS alumni who contributeand make a difference for ourpatients and our communitiesevery day.Here’s a way you can hearmore of these great stories — andshare yours! Join your fellowalums at the Alumni AssociationAnnual Meeting, Friday, April 21,2017, in Rochester. See details onpages 2-7. I guarantee you’ll haveconversations with fellow alumniwho are fascinating, exciting, funny,sensitive, dedicated and smart.During the past year, it’s beenmy pleasure to meet with andwork with many MCSHS alumnias association president. At theannual meeting, I pass the gavel toPresident-Elect Matthew Curran.Hope to see you there.Regards,Karen Sherk, NPPresident,MSHS Alumni AssociationNurse Practitioner ProgramClass of 2007ON THE COVER / Delsin Carter, alumnus of thePhlebotomy Technician ProgramC /// MAYO SCHOOL OF HEALTH SCIENCES
ContentsSEE YOU SOON / 4Alumni Association meeting April 21CHAMPION CLAIRE BENDER, MD / 5Former dean receives new awardGLOBAL TRAVELER / 8Mayo Medical Laboratories’traveling repBIG HEART / 10Providing needed care inher communityBABY ON BOARD / 12Caring for tiniest patientsduring transportABRACADABRA / 14CT technologist makesanxiety disappearMENTOR–MENTEEMATCHMAKING / 18Alumni Association launchesweb-based toolCARE IN A STORM / 20Pharmacy residents pitch inGREAT TEACHERS / 26 –28Preceptor and allied healtheducator honoredNori Brice,page 10.Mayo ClinicSchool of Health SciencesConnectionsA publication for alumni, students,faculty and friends of Mayo ClinicSchool of Health hsalumniSPRING 2017 /// 1
ALUMNI ASSOCIATION ANNUAL MEETING KEYNOTE PREVIEWClarity on concussionsConcussions should be taken seriously and treatedwith caution, but the benefits of youth sports faroutweigh the risks, according to a pair of Mayo Clinicspecialists in sports medicine.“Sports are extremely valuable to children, so don’tbe scared of letting them participate,” says DavidSoma, MD, a pediatric sports medicine physician.Dr. Soma and his colleague Cara Prideaux, MD, aphysiatrist, say that youth sports increase self-esteem,teamwork and graduation rates while loweringdepression rates.The physicians will share their expertise aboutconcussions as keynote speakers at the Mayo Schoolof Health Sciences Alumni Association AnnualMeeting, April 21, 2017, in Rochester.Both physicians are seeing an increase in thenumber of patients with possible concussions. Mostconcussions involve children because they comprisethe bulk of athletes competing in wrestling, icehockey, football and soccer — the sports with thehighest rates of concussion.David Soma, MD2 /// MAYO CLINIC SCHOOL OF HEALTH SCIENCESCara Prideaux, MDHowever, thanks to evolving protective equipmentand rules in sports, the physicians don’t necessarythink concussions are occurring more often. Instead,the reason for the increase may be heightenedawareness of concussions from news coverage ofprofessional athletes’ brain-rattling injuries.“We have a lot to learn about concussions,”Dr. Prideaux says. Research at Mayo Clinic is helpingto solve assorted mysteries.SusceptibilityCompared to adults, children may be slightly moresusceptible to concussions and might have a slightlylonger recovery, Dr. Soma says. It’s unclear yet whetherthe difference relates to a maturing brain, lack of neckstrength, head size, hormone levels or other factors.PreventionCoaches can help prevent concussions by avoidingunnecessary contact between athletes within andoutside of games. For example, Dr. Soma played footballfor a NCAA Division III national championship team.There was no contact between games.“My coach always said it made no sense to haveplayers getting injured during practice,” he recalls.In Rochester-area youth hockey, one innovativeapproach elevates the importance of safety byawarding a Fair Play point to teams that accumulatefew penalty minutes during a game. These Fair Playpoints can have an impact on tournament resultsand league standings.“This has been found to reduce the number ofall injuries, not just concussions,” Dr. Prideaux says,adding that researchers are looking to expand theconcept to other contact sports.
See you at theAlumni AssociationAnnual MeetingBrain needs to restafter concussionDavid Soma, MD, Community Pediatric andWhen someone has a possible concussion,Adolescent Medicine, and Cara Prideaux, MD,Dr. Prideaux and Dr. Soma say, rest is the bestPhysical Medicine and Rehabilitation, Mayomedicine. Their recommendations:Clinic in Rochester, will present “Confusionto Clarity: Helping to Create a BetterUnderstanding of Concussions” at theannual meeting of the Mayo School ofHealth Sciences Alumni Association.Friday, April 21, 2017Rochester Marriott Hotel101 First Ave. SWReception5:30 p.m.Program6:15 p.m.Dinner7:15 p.m.LEARN MOREThe evening is free for MCSHS alumni and aguest. Reserve your spot by April 14, 2017, athttps://2017mshsaadinner.eventbrite.com. Pull the player from the game. For the first one to three days, rest physicallyand mentally. That means limited or noschool and minimal other mental activitiesthat could worsen symptoms. Reintroduce activities gradually once givenpermission by a medical provider. Do not return to sports until fully recovered.The physical, cognitive, emotional andbehavioral symptoms typically clear upwithin one to two weeks. Follow a protocol of gradual return to play.Build from full-time school to non-contactpractice to full contact only in the absenceof symptoms. If the athlete has multiple concussions or hastrouble recovering, consider lower-risk sports.DiagnosisDiagnosis of a concussion today may be subjective,often based on parents observing a change inbehavior. “It’s not always, ‘My head hurts,’” Dr. Somasays. “A concussion often is manifested in the childacting differently. Parents know their kids best.”The search for objective diagnosis includesefforts to identify biomarkers in blood and the use ofelectroencephalography (EEG) to detect changes inbrain waves.TreatmentRest is standard treatment today. (See sidebar.)Researchers also are looking at ways to treatconcussions with medications.4 /// MAYO CLINIC SCHOOL OF HEALTH SCIENCESRecovery remains unpredictable. Some kids areable to return to contact sports in a week; others needa month or more. Factors that may prolong recoveryare younger age, a previous concussion, depression oranother mood disorder, a learning disorder, attentiondeficit hyperactivity disorder and headache disorders.Long-term effects“How much contact is too much?” Dr. Soma says.“We’re trying to predict who will go on to have along-term problem because of concussions, andwe’re looking at all the possible variables, includinggenetics. It’s probably different in each individual.”
ASSOCIATION NEWSClaire Bender, MD,recognized withinaugural Championof Allied Health AwardClaire Bender, MD, former dean of MayoClinic School of Health Sciences (MCSHS),seems a natural choice to be the firstrecipient of alumni association’s newChampion of Allied Health Award. But toDr. Bender, the award came as a surprise.SPRING 2017 /// 5
About the Champion ofAllied Health AwardThe Mayo School of Health Sciences AlumniAssociation Champion of Allied Health Awardwill be presented annually to recipientsnominated for their contributions towardpromotion, advocacy and advancementassociated with allied health professions.LEARN MOREtake care of patients. She expected us to take ourlast patients back to their rooms every morningand afternoon, which was something the orderliesusually did. That helped us get to know the patientsand their families, but also the desk attendants,the orderlies and others working in the hospitals.She taught us teamwork, and I never forgot thoseformative experiences.”Experiences like those solidified Dr. Bender’sappreciation for all members of the health care team.That attitude has been a hallmark of her career anda key element of her leadership contributions.Find the nomination form athttps://mshsalumni.mayo.edu/people/awards/“I was shocked,” she says. “I was humbled andhonored to hear that I’d received the award.”But Dr. Bender didn’t just receive the award.She inspired it.She was initially nominated for the alumniassociation’s Recognition of OutstandingContribution award, which honors alumni whohave made exceptional contributions in clinical care,research, mentoring and education, or humanitarianendeavors. But that didn’t seem like quite the rightrecognition for someone who had contributed somuch to the school and allied health.“We felt she deserved something more,” saysDeborah Oscarson, alumni relations businessanalyst. “That’s what inspired the alumni associationto create this award.”Early influencesDr. Bender’s appreciation for allied health workersdates back to her childhood.“My mom and my grandmother were nurses, andI saw how they helped people and how grateful peoplewere for that help,” she says. Those examples stuckwith her and influenced her decision to pursue anallied health career. She earned a bachelor’s degree atNebraska Wesleyan University and then enrolled inthe MCSHS Physical Therapy Program — where shereceived her first education in the Mayo Model of Care.She remembers clinical instructor Ruth Ryan.“She was a role model and mentor to me in how to6 /// MAYO CLINIC SCHOOL OF HEALTH SCIENCESNew Radiography ProgramAfter graduating from MCSHS, Dr. Bender wenton to medical school at the University of NebraskaCollege of Medicine. She returned to Mayo Clinicfor her residency in radiology and then joinedthe staff. One of her assignments was to developa new radiography program for MCSHS. Thatexperience led to leadership roles with state andnational certification and accreditation groups, andeventually, to her role as dean of MCSHS.It was a role that in many ways seemed tailormade for her, enabling her to live out the valuesinstilled in her by her parents.“My parents valued education and helping others,”she says. “I’ve always tried my best to help others andto help others pursue opportunities for education. Thebest part of my job was watching people grow.”Over 12 years as dean, Dr. Bender watched people— as well as programs — grow. She led a remarkableseries of changes that helped professionalize both theschool and allied health careers, including playingpivotal roles in establishing a University of Minnesotacampus in Rochester and in developing a Bachelorof Science in Health Professions degree at theuniversity. She also led the development of blendedlearning, which combines online and in-classroominstruction, and interprofessional education. And sheencouraged allied health faculty to pursue researchand publication opportunities.Dr. Bender says she’s grateful to alumni forrecognizing her own professional growth andcontributions.“It’s such an honor to be recognized,” she says.“This award means a great deal to me.”
Career highlightsChampion for afour-year degreeDr. Bender, who continues to care for patientsThe opportunity to earn a Bachelor of Science in Healthas a radiologist at Mayo Clinic in Rochester, hasProfessions — Respiratory Care from the University ofhad a career spanning Mayo’s three shields ofMinnesota Rochester almost didn’t happen.patient care, education and research. CareerThat’s according to Vanessa King, director, MCSHShighlights include:Respiratory Care Program. In 2008, discussions were Dean, Mayo Clinic School of Health Sciences,2002–2014progressing between the University of Minnesota Professor of Radiology, Mayo Clinic Collegeof Medicine Distinguished Educator Award, Mayo Clinic A leader in establishing University of Minnesotacampus in Rochester and its Bachelor ofScience in Health Professions degreeRochester and MCSHS to develop a bachelor’s degree.At first, it didn’t appear the prerequisites and theproposed curriculum would mesh into the four-yeardegree for respiratory therapists.“Dr. Bender was a champion for our students andthis degree,” says King. Respiratory Care did becomethe first MCSHS program to be part of the Bachelor ofHealth Sciences degree.“We were one program with a small number of Karis Award, Saint Marys HospitalSponsorship Boardstudents,” says King. “Even so, Dr. Bender said, ‘We are Prolific author, with more than 60 peer-reviewedpublications and 30 book chapterssure it would have happened.”going to advocate for the students.’ Without her, I’m notNow, Echocardiography, Radiography andSonography program students also can earn thebachelor’s degree.“ Dr. Bender was a champion for ourstudents and this degree.” VANESSA KINGSPRING 2017 /// 7
ALUMNUS PROFILEFirst Phlebotomy, then the worldDelsin Carter brings leading-edgemedical testing to distant cornersof the world as an internationalregional service representativefor Mayo Medical Laboratories.Carter trains staff at hospitals,clinics and laboratories in Canada,Europe, Asia, Africa and Australiato prepare and ship samples toRochester for testing. He graduatedfrom the Mayo Clinic Schoolof Health Sciences PhlebotomyTechnician Program four years ago.“Mayo Medical Laboratoriesprovides testing that even manyhospitals in developed countriesdon’t have,” Carter says. “Theresults we generate enablephysicians to treat patients inthe most effective way.”Carter indoctrinatesinternational clients in properprocedures for Mayo’s everexpanding testing capabilities.Language barriers don’tusually get in the way. “I speakGerman and English fluently andenough Swahili and Spanish toget fed and get home,” he says.“I usually learn a few basiccourtesies in other languages forthe sake of politeness,” he says.“Between the client's familiaritywith English, Mayo Clinictranslation services and GoogleTranslate, I can get it figured out.”8 /// MAYO CLINIC SCHOOL OF HEALTH SCIENCESCustomers generally use MayoMedical Laboratories to fill gaps inthe testing they offer. Some can’tafford to build a lab, and some can’tafford to buy the latest specialtyequipment. However, most canafford to send a sample to Mayowhen they need an answer.In many cases, a client as faraway as Asia can ship a specimento Mayo Clinic and get results inas little as three or four days.Carter sees lab services as anexcellent form of outreach fromMayo Clinic to distant patientsand providers. “We make a pieceof modern health care availableto the world,” he says.Before entering the PhlebotomyProgram, Carter worked as ahuman tissue culture specialist ata St. Louis, Missouri, biotech firm,but he hoped to work at MayoClinic. “It is a mecca of medicalinnovation and quality patientcare,” says Carter. “The PhlebotomyProgram was a wonderful stepping stone to where I am now.”Mayo Clinic in Rochesterhired Carter after he completedthe 10-week program. With abachelor’s degree in cell andmolecular biology from MissouriState University, an emergencymedical technician certificate andtwo years of experience in a lab,he started with the hospital clinicallaboratory code team. Rushingto any unit where a patient wasunresponsive or had no pulse, hedrew blood and conducted quicklab work at the bedside.“We supplied critical information to physicians so they couldreact in real time,” says Carter,who enjoyed the opportunityto use his emergency medicine,phlebotomy and lab skills.Nine months later, Carterwas promoted to technicalspecialist and put in charge ofgeneral coagulation testing for theRochester campus. He had thatposition for two years — untilJuly 2016, when Mayo MedicalLaboratories offered him the world.His job, he says, “is really aunique spot at Mayo Clinic and inhealth care, with a direct impacton global patient care.”Carter describes visits toother countries as eye-openingexperiences that allow him toshare Mayo Clinic’s expertise.“What they don’t have is oftenmost striking,” he says. “Abroad,you try to be as gracious as youcan and make suggestions for saferpractices. You learn to recognizethe limitations but, in the end, alittle bit of Mayo rubs off on allwith whom we interact.”
About thePhlebotomyTechnicianProgramFive times a year, MCSHS startsa new 10-week PhlebotomyTechnician Program inRochester, Minnesota.Phlebotomy technicianscollect and prepare bloodsamples for laboratory testing.Students complete about 160clinical training hours in 10weeks. A high school diplomaor equivalent is required beforestarting the program.“Being a phlebotomytechnician is a great place tostart a health care career,” saysMary Kaye Peterson, M Ed,director, Phlebotomy TechnicianProgram. “This program canlead to a first career job in justtwo and a half months. Forsome, it’s a first step to otherallied health or medical careers.”Nearly all programgraduates are offered positionsat Mayo Clinic.LEARN MOREIn his first months onwww.mayo.edu/mayo-clinic-the job, Delsin Carter,school-of-health-sciences/international regionalservice representativefor Mayo MedicalLaboratories, traveledto Canada, Romania,Germany, Taiwanand Hong Kong.
ALUMNA PROFILEMeeting the heart healthneeds of her communityNori Brice, DNP, RN, ACNP, acardiology nurse practitioner, ison a mission to raise awarenessabout heart health in NativeAmerican communities. Amember of the Navajo Nation,she spreads the word as aprivate practice cardiology nursepractitioner, nurse educator andresearcher in and around herhome in Flagstaff, Arizona.Brice, the oldest of sevensiblings, grew up on a reservationin New Mexico. “I was the firstin our family to get a collegedegree. I wanted to model thatfor my family.”Brice says she also wanted toserve as a model for the NativeAmerican community. “It’s reallyimportant to me that our peoplecontinue their education and bethe best they can be,” she says.And, she says, as healthy asthey can be.Brice focused her educationon health, earning a bachelor’sdegree in nursing. She laterpursued her master’s anddoctorate degrees as well. Shecompleted the Mayo Clinic Schoolof Health Sciences (MCSHS)Cardiology Nurse PractitionerFellowship in 2012.She says the fellowshipallowed her to “hit the groundrunning” when she beganpracticing independently, caringfor patients with both acute andchronic heart conditions.“Heart disease amongNative Americans is going up,and awareness is low,” shesays. “Our population has a lotof cardiovascular risk factors,including high rates of diabetes,high blood pressure and highcholesterol. But many people don’trealize the link between thoserisk factors and heart disease.”Since August 2016, Brice hasbeen helping to increase awarenessof heart health as an assistantclinical professor of nursing atNorthern Arizona University inFlagstaff. She spends two daysa week in Fort Defiance on theNavajo reservation, teachingnursing fundamentals to firstyear students in the university’sAmerican Indian NursingProgram.Brice also is a co-investigatoron a project at the university’sCenter for American IndianResiliency, working to raiseawareness of heart health amongNative Americans. “The goal isto increase knowledge of riskfactors associated with heartdisease and provide education ofthe signs and symptoms of acutecoronary syndrome. We will beproviding educational activitiesat community swap meets andsocial gatherings on the NavajoReservation.”Brice says that the cardiologynurse practitioner fellowshipprovided a great foundationfor her multifaceted career. “Iloved Mayo’s multidisciplinaryapproach, and its focus on thepatient’s needs,” says Brice.And she’s happy to helpmeet those needs in her owncommunity. “A good two-thirdsof the patients I see are NativeAmericans,” she says. “They seemto open up when I come into theroom. I feel patients are morereceptive to receiving informationthan they would from a nonnative person. It feels good to beable to meet those needs.”SPRING 2017 /// 11
ALUMNUS PROFILEEmergency: Baby on boardRyan Sura, RRT-NPS, breatheslife into the fragile bodies ofcritically ill and injured childrenwhen they’re en route toMinnesota’s only Level I pediatrictrauma center in a dedicatedchildren’s hospital.He’s a respiratory therapist forChildren’s Hospital and Clinics– Minneapolis and a member ofneonatal transport team. Hispatients range from 23-weekpreemies to full-term babies witha previously undiagnosed heartconditions.“When transporting patientsin critical condition, you need tothink critically and work as a teamwith your co-workers to get yourpatient to the hospital safely,” hesays. He works side by side with anurse practitioner and a paramedic.“It’s different than workingin the hospital. We have limitedresources and no immediatebackup.”Sura is one of 15 respiratorytherapists who work on theneonatal transport teams. Theybring babies from the Twin Cities12 /// MAYO CLINIC SCHOOL OF HEALTH SCIENCESmetro area, northern Minnesota,western Wisconsin, South Dakotaand North Dakota to the hospital.Last year, 600 infants came to thehospital via ambulance, helicopteror fixed-wing aircraft.How it startedAfter starting college at theUniversity of Minnesota in theTwin Cities, Sura enrolled in theMayo Clinic School of HealthSciences Respiratory Careprogram in Rochester because ofhis fascination with critical care.“I liked the idea of taking careof some of the sickest patients inthe hospital and working in allareas of the hospital instead of asingle unit,” he explains.During a semester of specialtyrotations, Sura found his nichein the neonatal intensive careunit and pediatric intensive careunit. After graduating in 2009,he joined Children’s Hospitalsand Clinics of Minnesota as arespiratory therapist in both ICUs,where he still works when notdoing transports.“The education I receivedin Rochester really preparedme to do the job,” he says.“I appreciated the clinicalexperience and the expertise ofthe staff and instructors. I sawhow the transport teams workedand wanted to be part of that.”A year after he joinedChildren’s, he achieved his goal:transport respiratory therapist. Heis certified as a neonatal pediatricspecialist, which authorizeshim to perform proceduresincluding endotracheal intubationand delivery of intravenousmedication.Sura offers this advice tostudents considering a career asa transport respiratory therapist.“Always continue to improve yourskills. Watch what the nurses do.Learn things outside the scopeof your normal practice.“When you provide critical carein an ambulance, you have to treatthe patient as whole and not justfocus on the heart and lungs.”
ALUMNUS PROFILEAbracadabra! Magic makesmedical care less scaryWhen Joe Swicklik, RT (R)(CT),radiologic technologist at MayoClinic in Arizona, startedworking with pediatric patients,something didn’t feel right.“I was performing examsthat were uncomfortable orscary for them,” says Swicklik,a 2005 graduate of the MayoClinic School of Health SciencesRadiography Program. “I askedmyself, ‘What can I do to make itbetter for them and for me?’”MAGIC!“Magic is wonderful for buildingrapport and engaging. It’ssomething kids absolutelylove,” says Swicklik, who hasbeen studying and practicingprestidigitation — sleight ofhands tricks — since he was 8years old.So he brought magic to MayoClinic and turned anxiety intogiggles, by making objects appearor disappear, by transforming aCT scanner into a toy-makingmachine and by making funnysounds come from intimidatingmedical equipment.14 /// MAYO CLINIC SCHOOL OF HEALTH SCIENCESIf magic helps childrenhold still, there’s less need forimmobilization tools or sedation,he says. The experience is betterfor the child and the parents.“The results are quite amazing,”Swicklik says. “Earlier this week,a young child was in for a cardiacstudy. The mom was so happyto see her child laughing andgiggling. The stress level wentfrom 10 to 2. And I was able toget better images because therewas less motion.”After becoming a CT technologist, Swicklik transferred to theRochester campus in 2009. Forthe past five years he has beensharing how magic can be usedas a tool in the medical setting. Inpresentations to departments andconferences, he explains how tomake patients’ anxiety vanish:Be aware of your audience. Heperforms magic only when hesenses that it might benefit thepatient. For example, if the patientsees people in scrubs as paingivers, turning a tissue into a rosesuddenly makes him fun andinteresting.Set the stage. Theater uses music,lighting, color and images tocontrol how the audience feelsand reacts. “We can use the sameideas in a medical setting to helppatients relax,” Swicklik says.Build rapport quickly. “I need tobe a likable person in the first 10seconds,” he says.Use the power of suggestion. Byinvolving patients in the story andgiving simple, playful instructions,you can get them to do what isneeded to complete their care.Swicklik advocates more magicbecause he’s seen sleight of handbring comfort to patients of allages. Mayo Clinic has recordedvideos of Swicklik teaching simplemagic tricks for staff learningmodules.“We have music therapy,” hesays. “Why not magic therapy? Ithink it could benefit patient care.”LEARN MOREWatch and learn patient-focusedmagic from Swicklikyoutube.com/watch?v jgGDQXSSoT8
Poof! Anxiety disappearswhen CT TechnologistJoe Swicklik brings out amagic trick.
Pam Lovett strollswith her menteeJeannie Yen, whonow works as abusiness analystfor Florida Blue,Jacksonville, Florida.
LET’S TALKWhy we all could benefitfrom a mentorBy Jeannie YenWhen I started graduate schoolfor health administration in 2014,I was one of the few students inmy cohort who did not have anyexperience in health care.Though I valued everything Ilearned throughout the program,I did not know what area of healthcare I was interested in until thesemester before graduation. That’swhen I started the AdministrativeInternship Program throughMayo Clinic School of HealthSciences (MCSHS). One of myprojects was assessing patientexperience data for transplantpatients, and I quickly learnedthat my passion was data analysis.Looking back, I wish I had amentor who might have helpedme discover my passion earlierin my graduate studies.During my time at MayoClinic, I worked closely with PamLovett, DNP, CRNA, ARNP.She’s a MCSHS alumna, programdirector for the MCSHS Doctorateof Nursing Practice AcademicSupport Program and my mentor.She is part of the team thatdeveloped the new mentorshipprogram for MCSHS alumni.(See story page 18.)As my mentor, Pam providedme insight on the importanceand need for mentorship. I seementorship as a professionaldevelopment tool that allowedme to gain knowledge andskill from someone who hassuccessfully mastered skills I’minterested in developing.Although we comefrom different professionalbackgrounds, our mentorshiprelationship worked. Pam’sacademic and professionalachievements showed me herdetermination. That inspired meto learn how I could become aleader early in my career. Duringmy internship, I expressed interestin learning more about otherareas within Mayo Clinic. Pamconnected me with contacts inthose departments, somethingthat would have been moredifficult without her help.Pam also showed me thata mentorship relationship ismutually beneficial. Abouthalfway into my summerinternship, Pam asked me toconduct a mock job interviewfor her as a fun exercise. I didn’timmediately understand thepurpose. She told me this mockinterview was to both helpher prepare for an upcominginterview and give me practice forfuture interviews I will conductas a health care administrator.It was an opportunity for me tohelp Pam.As I grow in my career,I would definitely love to bea mentor. I’m excited to seehow I could share my skillsand knowledge and encouragemy protégé’s academic orprofessional career.I encourage both students andalumni to participate in the newmentorship program. We couldall use a little advice and help toachieve our goals sooner!Jeannie Yen is a 2016graduate of the MCSHSAdministrative InternshipProgram. The program allows studentsenrolled in health administration orbusiness administration baccalaureateor master’s program at MCSHSaffiliated education institutions tocomplete an administrative internshipas part of their required education.SPRING 2017 /// 17
SIGN UP NOW TO BE A MENTORAlumni Association launches webtool for students to find mentorsThe Mayo School of HealthSciences Alumni Association haslaunched a web-based tool formatching students and alumnimentors.Called Alumni Connect, itoffers a simple way for Mayo ClinicSchool of Health Scie
annual meeting of the Mayo School of Health Sciences Alumni Association. Friday, April 21, 2017 Rochester Marriott Hotel 101 First Ave. SW Reception 5:30 p.m. Program 6:15 p.m. Dinner 7:15 p.m. LEARN MORE The evening is free for MCSHS alumni and a guest. Reserve your spot by April 14, 2017, at