Transcription
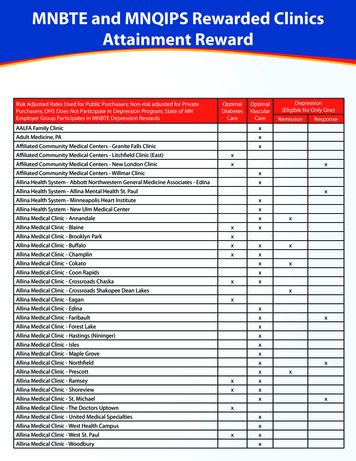
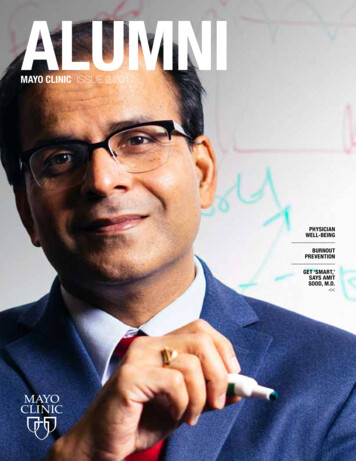
ALUMNIMAYO CLINIC ISSUE 2 2017PHYSICIANWELL-BEINGBURNOUTPREVENTIONGET ‘SMART,’SAYS AMITSOOD, M.D.
LETTER FROM THESECRETARY-TREASURERThe theme of this issue of Mayo Clinic Alumni is takingcare of the physician or scientist. Physician burnout is amajor national problem. Mayo Clinic leads the countryin research on this important matter and is a pioneerin taking organizational steps to reduce burnout.Research shows that finding meaning in your life’swork and having time to spend on the areas you findmost rewarding are vital to physician satisfaction andburnout prevention. Mayo Clinic’s Values Councilestablishes a foundation for our primary value — theneeds of the patient come first — and helps to remindus why we pursued careers in medicine.In addition to reading about our Values Councilin this issue, you’ll learn about Mayo EmployeeResource Groups (MERGs), which can help staffmembers feel more at home; our Physician HealthCenter, which helps to ensure the health and wellbeing of the physician workforce around the country;resiliency and its role in burnout prevention; and ourHealthy Living Program for Physicians, an immersiveCME program to improve physicians’ awareness ofthe relationships among lifestyle habits, diet, physicalactivity, resilience, stress management and health. Youalso will find information about steps organizations cantake to improve and prevent physician burnout as wellas how Mayo Clinic School of Medicine and the MayoFellows’ Association are combatting this problem.While we don’t have all the answers, we do puta high priority on the well-being of our staff and allthose who care for our patients.Also in this issue are profiles of our Balfour andKendall research award recipients. Both are risktakers — in the course of their careers, in the subjectsof their research and in other ways. We’re proud thatthey’ve chosen to be affiliated with Mayo Clinic. Wealso include a feature on alumnus Kofi Boahene, M.D.PETER AMADIO, M.D. (OR ‘83) Secretary-Treasurer, Mayo Clinic Alumni Association Lloyd A. and Barbara A. Amundson Professor of Orthopedics(ENT ’04), a head and neck surgeon at Johns Hopkins.His story, which was featured on CNN a few yearsago, is a study in determination.Finally, registration is open for the Alumni Association Biennial Meeting in Florida in October. Wehave a fantastic multidisciplinary scientific programprepared for you. Plus you’ll have a front-row seatto check out all the great things happening on ourFlorida campus. Contact someone you trained with,a current or former alumnus colleague, a mentoror a friend, and plan to attend together. You’ll haveopportunities to reconnect with fellow alumni andbecome reinvigorated in the Mayo spirit. You neverknow — attending might be a positive step in takingcare of yourself and keeping burnout on the backburner. I’ll be there, and I hope to see you there.
TABLE OFCONTENTSFEATURES2 Empowering the keepersof the flame36 Alumni Association Biennial MeetingThe future of medical education andcutting-edge innovationMayo Clinic Values Council6 MERGs can make youfeel at home38Mayo Employee Resource Groups8 Leader of the pack in remediatingphysician burnoutIf it’s broke, fix it2 017 Balfour Award recipientJohnathon Aho, M.D., Ph.D.40Challenge to the diabetes status quo2017 Kendall Award recipientRene Rodriguez Gutierrez, M.D.16 Strategies to prevent burnout innext generation of physicians18 Mayo Clinic Physician Health CenterCaring for the physician workforce,one physician at a timeMAYO CLINIC UPDATE43 Fortune ‘100 Best Companiesto Work For’22 Mayo gets SMART about resiliency Doctors Mayo Society celebrates40 years26 A place for physicians to focus44for burnout preventionon their own well-beingMayo Clinic Healthy Living Programfor Physicians30Online storiesObituariesWhere are they now?Kofi Derek Owusu Boahene, M.D.ISSUE 220171
EMPOWERINGTHE KEEPERSOF THE FLAMEMayo Clinic Values Council“It has been our desire to maintain at Rochester aninstitution in which medical and surgical treatmentmay be had by anyone, without regard to financialstatus, race, color, or creed — all meeting on acommon level.” – William J. Mayo, M.D.The Mayo Clinic Values Council is charged with promotingMayo’s institutional values throughout the organization,and promoting and perpetuating the Franciscan legacy inthe Mayo Clinic Hospital – Rochester, Saint Marys Campus.The Values Council was established in 2013 to replace theSponsorship Board when Saint Marys and Methodist hospitalsbecame a single licensed hospital entity. The Sponsorship Boardwas focused primarily on the Saint Marys Campus.‘NO SMALL CHARGE’Keeping intact the values of a large organization is no small charge.Robert Brown Jr., M.D. (MED ’87, N ’92), chair of the Division of Strokeand Cardiovascular Diseases, chair of the Values Council and the JohnT. and Lillian Mathews Professor of Neuroscience, says the group isn’tactually the keeper of Mayo’s institutional values. “All 65,000 of us atMayo are the keepers of our values and values-driven culture, alongwith our 30,000 alumni around the world. The Values Council providesresources and assists in the promotion and protection of our valuesacross all three shields.”2MAYO CLINIC ALUMNI
ROBERT BROWN JR., M.D.ISSUE 220173
‘UNYIELDING DEDICATION TO PRIMARYAND CORE VALUES’The Values Council reports administratively to theProgram in Professionalism and Values and to theMayo Clinic Board of Governors annually.That the Values Council reports to the Board ofGovernors is an indication of how seriously Mayotakes the perpetuation of its core beliefs, accordingto Dr. Brown. “Mayo Clinic’s primary value — theneeds of the patient come first — has been in placefor more than 100 years,” he says. “Our unyieldingdedication to our primary and core values helps todefine why we have a Values Council. This may bewhere we differ from some other medical institutions.If you ask Mayo employees what our primary value is,most of them will be able to tell you.”The council focuses on how to make the valuescome to life in the actions and behaviors of employees. The group makes presentations to departmentsand work units, and provides curriculum and toolsto empower work groups to understand andpromote the values.“You can’t teach values the way you would ascientific topic,” says Dr. Brown. “We provide theresources to get the discussion started regarding ourvalues and their importance to all of our behaviorsas individuals and as an institution. Mayo Clinic has3,000 to 5,000 new employees each year. How do weassist them in understanding our culture and valuesand integrating the values into our expectations ofthem? That’s where the Values Council comes in.”“We have an ongoing challengeto make sure our institution’sdecisions and behaviors arealigned with our professedvalues.” – Robert Brown Jr., M.D.Charge of the Values Council Promote Mayo Clinic values across all of Mayo Clinic. Assist in perpetuating the Franciscan legacy on theSaint Marys Campus. Foster aligned partnerships with related programs, officesand activities across Mayo Clinic. Continue and enhance the work of the former Sponsorshipcommittees — Education Committee, Research Committee,Values Review Committee and Pilgrimage Program.Primary value The needs of the patient come first.Core values Respect: Treat everyone in our diverse community includingpatients, their families and colleagues with dignity. Integrity: Adhere to the highest standards of professionalism,ethics and personal responsibility, worthy of the trust ourpatients place in us. Compassion: Provide the best care, treating patients andfamily members with sensitivity and empathy. Healing: Inspire hope and nurture the well-being of the wholeperson, respecting physical, emotional and spiritual needs.4‘ONGOING CHALLENGE’ TO ALIGN DECISIONSAND BEHAVIOR WITH VALUES “Medicine today is very complex, and Mayo is a muchlarger institution than it was in the past,” Dr. Browncontinues. “We have an ongoing challenge to makesure our institution’s decisions and behaviors arealigned with our professed values. I believe Mayo’svalues are evident to patients and visitors to ourlocations. If we can continue to have our primary andcore values be the guiding principles of what we doand help our employees find purpose in their work,we’ll continue to have the strong, values-drivenculture we’ve had for more than a century. Thisremains a key differentiator for Mayo Clinic.” MAYO CLINIC ALUMNITeamwork: Value the contributions of all, blending the skillsof individual staff members in unsurpassed collaboration.Innovation: Infuse and energize the organization, enhancingthe lives of those we serve, through the creative ideas andunique talents of each employee. Excellence: Deliver the best outcomes and the highest qualityservice through the dedicated effort of every team member. Stewardship: Sustain and reinvest in our mission andextended communities by wisely managing our human,natural and material resources.
FAST 5DR. BROWN1 Do other organizations have groupslike Mayo’s Values Council?No, this is unusual. Most organizations have corevalues. Unfortunately sometimes they’re not takenvery seriously and are not used to guide an organization’s actions and decisions. At Mayo we take ourvalues very seriously and have the Values Council inplace to make sure they’re promoted, perpetuated andprotected among all employees in practice, educationand research, in good times and in tough times.We’re intentional about our values-driven cultureand have maintained our values even as we’ve growntremendously and evolved over the last 150 years tobe a world-renowned medical center.I like to think this is what differentiates Mayo.It’s why patients say they feel something special herethey’ve never felt before at a medical institution —because we mean what we say and put action andcommitment behind the statement. When you’re atMayo, you see that dedication in colleagues acrossall three shields. The feeling is palpable.2 Is the Values Council associatedwith religion?No. We do perpetuate the Franciscan legacy at theSaint Marys Campus, given the extreme importanceof the Mayo-Franciscan partnership from the timeSaint Marys was built in the late 1880s to the currenttime. Also, importantly, through our healing corevalue, we respect that some of our patients have aspiritual connection, whether it’s religious or not, aspart of their lives.3 How did you become the first medicaldirector of the Values Council?4 How were Mayo’s valuesinculcated in you?5 How can Mayo’s values affect physiciansatisfaction and counter burnout?I’ve been at Mayo for 34 years. I had the opportunityto train here and previously served in several leadership roles, including chair of the Department ofNeurology. When the Values Council was forming,I was asked to become the medical director. It was atremendous honor to be asked because I’m passionateabout the importance of these values to Mayo Clinic— to our past, to the present and to our future.I learned a tremendous amount from the mentorswho educated me and who I observed throughoutmy training. As a medical student, I interacted withphysicians, scientists and allied health colleaguesand had the opportunity to see how they put theMayo values in action through their behaviors acrossall three shields. The impact of mentorship andlearning from colleagues across all disciplines in allthree shields cannot be overstated. Observing mycolleagues day in and day out during medical school,residency and beyond molded me as a clinician,educator and researcher and taught me the values.Our values are part of our culture and integralto our institutional DNA. There’s a feeling at Mayothat you succeed when you help your colleaguessucceed, and that could not be truer. I surelybenefited from that via tremendous mentorshipthroughout my training and career. I couldn’timagine having completed my training or havingmy career anywhere else.A key issue in reducing burnout is defining meaningin your work and enhancing engagement. For manyof us, meaning in our work is based on Mayo’sprimary value — the needs of the patient comefirst — and on our core values. Lessening burnoutis a multifaceted issue, including important institutional factors. We must provide an environment inwhich all Mayo colleagues feel they can live out theprimary and core values.ISSUE 220175
MERGS CAN MAKEYOU FEEL AT HOMEMayo Employee Resource GroupsThe India Mayo Employee Resource Grouptremendous opportunity to learn from others’(MERG) at Mayo Clinic in Rochester helps Ektaparenting experiences,” says Dr. Kapoor.Kapoor, M.B.B.S. (I ’08, ENDO ’12), Divisions“Belonging to the MERG also helps me stayof General Internal Medicine and Endocrinology,connected with the community outside of work andDiabetes, Metabolism, & Nutrition, stay connected tomanage work-life balance. Our MERG providesher culture. She and her husband, Prashant Kapoor,opportunities for community service, and membersM.D. (HEM ’09, HEMO ’12), Division of Hematology,share values, dreams, ambitions and a common mission,are from India, and they want to keep thatand we help each other achieve those missions.”perspective alive for their children.Dr. Kapoor says she’s gotten so much“I grew up in India and cameout of the India MERG that she’sto the U.S. in 2003,” she says.considering joining the Greater“I love working here, and ourLeadership Opportunities forfamily has embraced livingWomen (GLOW) MERG. “Ihere. But I want to stay convalue interacting with andnected to my roots and keeplearning from people in simmy cultural backgroundilar situations —professionand values alive in my mindal or personal. It provides— this is my identity. Thisa sense of solidarity, buildsis the information I want toself-confidence and helpspass along to my kids as well.”with problem-solving.”EKTA KAPOOR, M.B.B.S. (LEFT),Part of the Office ofAnjali Bhagra, M.D.AND ANJALI BHAGRA, M.D.Diversity and Inclusion, Mayo(I-1 ’05, I ’08), also is a member ofEmployee Resource Groups (MERGs)the India MERG and a departmentare groups of employees across locationsdiversity leader for the Division of Generalwho collectively and actively engage or gather aroundInternal Medicine. She’s presented to the MERGa unifying purpose, mission, background or activity.about stress management, resiliency and womenThe India MERG meets quarterly. The approximatelyin leadership. “I like contributing to my colleagues’135 members engage in professional developmentwellness and sense of belonging,” she says. “MERGsactivities and plan activities and get-togethers.are valuable resource groups outside of your regular“Many women in the group have childrenwork area, and provide opportunities to supportaround the same ages as mine, and there isothers and lean on others for support.”6MAYO CLINIC ALUMNI
Members of the India MERG gathered at Mayo’s annualFestival of Cultures. (From left) Aparna Velamala,Data Programming Services; Sneha Vivekanandhan,Mayo Clinic Graduate School of Biomedical Sciences;Poorval Joshi, Ph.D. (MPET ’16), Yale University Schoolof Medicine; Pavithra Bora; Sonu Kashyap, Ph.D.(LABM ’15), Department of Laboratory Medicine andPathology; Sumathi Jayakumar, Media Support Services;Nalini Krishnan, Management Engineering & InternalConsulting; and Sandhya Devarajan, M.B.B.S. (ONCL ’17),Division of Medical Oncology.About MERGs Employees, trainees and students from throughout the organi- Chinesezation can participate. Membership in a MERG is voluntary. disABILITYMERGs support Mayo’s diversity and inclusion strategies eMERGing Leadersand goals. FilipinoThe Mayo Clinic Office of Diversity and Inclusion approves FRESH (Family Resource, Event and Support Hub)and coordinates MERG programs and events, and provides Greater Leadership Opportunities for Women (GLOW)tactical, administrative and oversight support. IndiaMeetings take place outside of regular work hours or Influence, Inspiration, and Growth Professionalduring lunch.Development Group Iranian HeritageMayo Clinic MERGs include: Latinos y Latinos (Hispanic) African Descendants LGBTI (lesbian, gay, bisexual, transgender, intersex or allies) ALMA (Hispanic/Latino culture and heritage) Multicultural Nurses Arab Heritage Pan-Africa Asian Connection Somos Latinos Caribbean Heritage Transcultural Patient Care Celebrate Dakota! VeteransISSUE 220177
8MAYO CLINIC ALUMNI
LEADER OF THE PACKIN REMEDIATINGPHYSICIANBURNOUTA health care organization’s health is profoundlyaffected by the well-being of its physicians. In the lasttwo decades Mayo Clinic has taken a leadership positionin studying physician burnout and crafting and testingstrategies to halt its encroachment on physician health.In the spirit of the maxim “Physician, heal thyself,”Mayo has made demonstrable, sustained progress inimproving burnout among its physician corps.ISSUE 220179
Earlier this year Tait Shanafelt, M.D. (HEMO ’05),Division of Hematology at Mayo Clinic inRochester and director of the Mayo ClinicProgram on Physician Well-being, and JohnNoseworthy, M.D. (N ’90), Mayo Clinic presidentand CEO, co-authored “Executive Leadership andPhysician Well-being: Nine Organizational Strategiesto Promote Engagement and Reduce Burnout,”which was published in Mayo Clinic Proceedings.Here, Mayo Clinic Alumni synopsizes that article.“When you look at the nationalphysician burnout problem, it’slike the shoemaker’s childrengoing barefoot. In addition tocaring for our patients, we needto devote attention to caringfor our caregivers.”– John Noseworthy, M.D.SCOPE OF THE PROBLEMPhysicians are under constant pressure to increaseproductivity — caring for more patients withunchanging time and resources, and expectationsto improve efficiency and reduce expenses.“Do more with less” is the mantra. National studies indicate that at least 50 percent ofU.S. physicians experience professional burnout,which is characterized by exhaustion, cynicismand reduced effectiveness at work. Physician burnout has increased during the lastdecade and is dramatically higher than burnoutin other professions. Specialties with the highest rates of burnoutinclude family medicine, general internal medicineand emergency medicine. TAITSHANAFELT,M.D.10MAYO CLINIC ALUMNIEFFECTS OF BURNOUTPhysician burnout affects quality of care, patientsafety, physician turnover, physician work effortand patient satisfaction. Burnout also affectsphysician prescribing habits and test ordering, riskof malpractice suits and patient compliance withphysician recommendations. Regarding work effort, a Mayo Clinic studyshowed that every 1-point decrease in physiciansatisfaction (on a 5-point scale) was associatedwith a 30 to 40 percent increase in the likelihoodthe physician would reduce his or her work effortduring the next 24 months. The cost of replacing aphysician is estimated to be two to three times thephysician’s annual salary. Burnout also has personal repercussionsincluding broken relationships, alcoholism andphysician suicide. These significant negative effects make the casefor health care organizations to monitor and try toimprove physician burnout.“If you knew your organization had an issuethat threatened patient care quality and satisfaction,not to mention physicians’ lives and livelihood,you would quickly deploy resources to address theproblem,” says Dr. Noseworthy. “We exist to providemedical care to our patients — to try to improvetheir overall health. When you look at the nationalphysician burnout problem, it’s like the shoemaker’schildren going barefoot. In addition to caring forour patients, we need to devote attention to caring
for our caregivers. Promoting physician well-beingis central to the wellness of our entire organization.Healthy, engaged physicians are necessary toachieve our objectives.”Dr. Noseworthy says most institutions put theburden of improving burnout and professional satisfaction on the individual physician, expecting them totake self-help steps to address the problem. In reality,however, the burnout problem has organizational,personal and national aspects, and the responsibilityto fix it should be shared by health care organizationsand their employees.Organizational factors that play a role in burnoutare workload, efficiency, flexibility and control overwork, work-life integration, alignment of individualand organizational values, social support andcommunity at work, and degree of meaning derivedfrom work.Rather than simply reduce burnout, Mayo strivesto cultivate physician engagement, characterized byvigor, dedication and absorption in work.“Small investments in physician engagementcan have a large impact,” says Dr. Noseworthy.“Leadership and sustained attention from thehighest level of the organization are the keys tomaking progress.”CASE IN POINTBetween 2011 and 2013 Mayo’s physician burnoutrate ticked up from lower than average to similar tothe national rate. Improvement efforts implementedbetween 2013 and 2015 resulted in a decrease of7 percent while the national rate increased byJOHNNOSEWORTHY,M.D.11 percent. Today Mayo’s physician burnout rate is32.9 percent compared to 48.8 percent nationally.While pleased with the improvement,Dr. Noseworthy isn’t content. “With one-third ofour physicians affected, we have more work to do,”he says. “Dr. Shanafelt and his colleagues in ourProgram on Physician Well-being continue theirdogged pursuit of research and trials of strategies toeffectively stem the tide of burnout. We embrace ourorganizational responsibility to continue to evolvein an effort to improve the well-being of both ourphysicians and Mayo Clinic.”PHYSICIAN BURNOUT RATEMAYO CLINICNATIONALLY32.9%48.8%ISSUE 2201711
Research indicates that physicians who spend atleast 20 percent of their professional effort focusedon the aspect of work most meaningful to them areat a dramatically lower risk for burnout.ORGANIZATIONAL STRATEGIES1 Acknowledge and assess the problemIt’s important for the highest level of leadershipto acknowledge physician burnout. CEOs can engagewith physicians through face-to-face meetings,video interviews, town halls and radio broadcasts.Physician well-being must be measured as a routineinstitutional performance metric.“Organizations measure what they consider mostimportant to their success,” says Dr. Shanafelt. “Physician well-being should be one of those measures.”Mayo Clinic has measured physicians’ professional satisfaction since 1998 and has measuredburnout since 2010. Other aspects of well-being Mayomeasures annually and compares to national datainclude engagement and satisfaction with work-homeintegration. Division and department heads receiveaggregated results to know where to deploy attentionand resources.In addition to developing physician leaders withthe skills necessary to lead, organizations mustmeasure leader performance.Mayo Clinic physicians have the opportunityto evaluate the leadership of their immediatesupervisors annually, a measure that is used inleaders’ performance reviews. Mayo research showsthat each 1-point increase in the leadership scoreof a physician’s immediate supervisor is associatedwith a 3.3 percent decrease in the likelihood of thephysician’s burnout.2 Harness the power of leadershipDesirable qualities in physician leaders includethe ability to listen, engage, develop, motivate andorganize fellow physicians. Physician leaders areresponsible for identifying the talents and motivatorsof the physicians on their teams. Research indicatesthat physicians who spend at least 20 percent of theirprofessional effort focused on the aspect of work mostmeaningful to them — caring for a specific type ofpatient or a particular health condition, or activitiessuch as patient education, community outreach,mentorship or teaching — are at a dramatically lowerrisk for burnout.12MAYO CLINIC ALUMNICOLIN WEST,M.D., PH.D.
3 Develop and implement targetedinterventionsMany of the contributors to burnout and solutionsare work unit-specific rather than institution-wide.Mayo Clinic identified divisions and departmentswith satisfaction rates lower than the nationalaverage and burnout rates higher than the nationalaverage, and engaged those units to determineareas for improvement. Of seven units involved inthis process in 2013, all seven had improvement inburnout and satisfaction. The interventions werelocal, based on the units’ specific needs.4 Cultivate community at workPhysicians’ sense of community has beeneroded by rising productivity expectations,increased clerical and documentation burdens,and the elimination of physician-dedicated spacessuch as lounges and dining rooms. Those spacesallowed for interpersonal connections and organicpeer support, and getting rid of them contributedto many physicians feeling more isolated.Organizational strategies are necessary to unitephysicians and create opportunities for support.In 2001 Mayo Clinic in Rochester introduced adedicated meeting area for physicians, scientistsand senior administrators, complete with free fruitand beverages, lunch tables, food for purchase andcomputer stations. The space was so well receivedthat similar areas were added on the Florida andArizona campuses, and a second room was addedon the Rochester campus.Mayo also added a physician-support program,COMPASS (Colleagues Meeting to Promote andSustain Satisfaction). In COMPASS groups, alsoknown as Physician Engagement Groups, physiciansspend one hour every other week meeting withcolleagues. These groups of six to 10 physiciansmeet for a meal paid for by Mayo Clinic and discussspecific subjects related to being physicians.Studies led by Colin West, M.D., Ph.D. (I ’03,CMR ‘04), associate director of the Mayo ClinicProgram on Physician Well-being, indicate themeetings have led to improvement in meaning-inwork measures and burnout. As a result, Mayo madeCOMPASS groups available to all physicians andPotential impact of burnout onU.S. physician workforce The U.S. Department of Health and Human Servicespredicts a shortfall of 45,000 to 90,000 physicians by 2025. The Association of American Medical Colleges predictsthat in less than 10 years the U.S. will have 90,000 fewerphysicians than it needs. The shortage may be more acute in specialties such asprimary care and general surgery. Higher emotional exhaustion (a dimension of burnout)is associated with increased likelihood that physicianswill reduce their professional work effort. The prevalence of burnout is increasing among The increase in burnout between 2011 and 2014 likelyU.S. physicians.translated into an approximate 1 percent reduction in theprofessional effort of the U.S. physician workforce dueto physicians reducing work hours — the equivalent ofeliminating the graduating class of seven U.S. medicalschools. That estimate doesn’t account for physicians leavingthe profession altogether or retiring early due to burnout. Reducing professional work effort appears to be an effectivestrategy for individual physicians to reduce burnout but couldexacerbate the pending physician workforce shortage.ISSUE 2201713
scientists across the enterprise. In the first 10 monthsabout one-third of physicians and scientists acrossthe organization joined a COMPASS group.5 Use rewards and incentives wiselyPhysicians who are incented to be more productive may spend less time with each patient, order moretests or procedures, and work longer hours. Evidencesuggests the behaviors associated with these incentivesworsen quality of care and increase the risk of burnout.Mayo Clinic uses a salaried compensation modelto counter this issue although other approaches alsomay be effective. Rather than offer extra financialcompensation for productivity, rewards to considerinclude schedule flexibility or protected time forpursuits including research and education that addmeaning to work.6 Online storyIn fall 2012 we profiled then-residents Cadman Leggett, M.D.(I ’12, CI ’13, GI ’15), and Jane Njeru, M.B., Ch.B. (I ’12,PCIR ’13), in a story about physician burnout. Five yearslater we check in with these Mayo Clinic faculty membersto learn how their stresses have changed and how theymanage work-home life MAYO CLINIC ALUMNIAlign values and strengthen cultureMayo Clinic regularly asks physicians and staffto evaluate how well it meets its mission — the needsof the patient come first. This appraisal helps to makesure the organization’s culture, values and principlesare aligned with its mission.A 2011 staff survey revealed that Mayo physiciansperceived organizational erosion in commitment tostaff. Mayo convened a task force of physicians andscientists to study the problem and pinpoint the areasthat needed the most improvement. Over 18 monthsthe task force led activities that articulated Mayo’svalues in surveys and focus groups.This process of value alignment affirmed that theorganization and its physicians were working towarda common goal, and created a touchstone documentthat delineates the principles of that partnership.7 Promote flexibility and work-life integrationU.S. physicians are twice as likely to be dissatisfied with work-life integration as workers in otherindustries. Full-time medical practice can be prohibitiveto the integration of personal and professional life.Organizations can offer reduced work hours, inexchange for reduced compensation, and scheduleflexibility to allow physicians to better meet theobligations in both parts of their lives. These can beimportant recruitment and retention strategies as wellas contributors to physician well-being and satisfaction.
8 Provide resources to promoteresilience and self-careOpportunities and resources for physicians to practicewell-being must be accompanied by organizationalefforts to improve systemic problems that contributeto burnout. This helps to ensure that the issue isn’tphysicians themselves but, rather, a multiface
Mayo Clinic Board of Governors annually. That the Values Council reports to the Board of Governors is an indication of how seriously Mayo takes the perpetuation of its core beliefs, according to Dr. Brown. "Mayo Clinic's primary value — the needs of the patient come first — has been in place for more than 100 years," he says.