Transcription
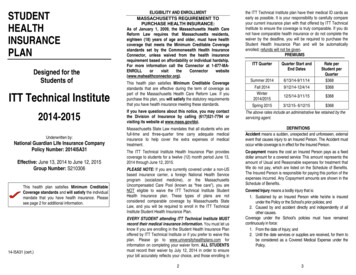
STUDENTHEALTHINSURANCEPLANDesigned for theStudents ofELIGIBILITY AND ENROLLMENTMASSACHUSETTS REQUIREMENT TOPURCHASE HEALTH INSURANCE:As of January 1, 2009, the Massachusetts Health CareReform Law requires that Massachusetts residents,eighteen (18) years of age and older, must have healthcoverage that meets the Minimum Creditable Coveragestandards set by the Commonwealth Health InsuranceConnector, unless waived from the health insurancerequirement based on affordability or individual hardship.For more information call the Connector at lthconnector.org).the ITT Technical Institute plan have their medical ID cards asearly as possible. It is your responsibility to carefully compareyour current insurance plan with that offered by ITT TechnicalInstitute to ensure the coverage is truly comparable. If you donot have comparable health insurance or do not complete thewaiver by the deadline, you will be required to purchase theStudent Health Insurance Plan and will be automaticallyenrolled; refunds will not be given.PREMIUMSITT QuarterQuarter Start andEnd DatesRate perStudent perQuarter 368Summer 20146/13/14-9/11/14Fall 2014Winter2014/20159/12/14-12/4/14 36812/5/14-3/11/15 368Spring 20153/12/15- 6/12/15 368ITT Technical InstituteThis health plan satisfies Minimum Creditable Coveragestandards that are effective during the term of coverage aspart of the Massachusetts Health Care Reform Law. If youpurchase this plan, you will satisfy the statutory requirementsthat you have health insurance meeting these standards.2014-2015If you have questions about this notice, you may contactthe Division of Insurance by calling (617)521-7794 orvisiting its website at www.mass.gov/doi.The above rates include an administrative fee retained by theservicing agent.Underwritten by:Massachusetts State Law mandates that all students who arefull-time and three-quarter time carry adequate medicalinsurance to help cover the extra expenses of medicaltreatment.DEFINITIONSAccident means a sudden, unexpected and unforeseen, externalevent that causes injury to an Insured Person. The Accident mustoccur while coverage is in effect for the Insured Person.The ITT Technical Institute Health Insurance Plan providescoverage to students for a twelve (12) month period June 13,2014 through June 12, 2015.Co-payment means the cost an Insured Person pays as a fixeddollar amount for a covered service This amount represents theamount of Usual and Reasonable expenses for treatment thatWe do not pay, which are listed on the Schedule of Benefits.The Insured Person is responsible for paying this portion of theexpenses incurred. Any Copayment amounts are shown in theSchedule of Benefits.National Guardian Life Insurance CompanyPolicy Number: 2014I5A31Effective: June 13, 2014 to June 12, 2015Group Number: S210306This health plan satisfies Minimum CreditableCoverage standards and will satisfy the individualmandate that you have health insurance. Pleasesee page 2 for additional information.14-I5A31 (cert.)PLEASE NOTE: If you are currently covered under a non-USbased insurance carrier, a foreign National Health Serviceprogram (socialized medicine), or the MassachusettsUncompensated Care Pool (known as “free care”), you areNOT eligible to waive the ITT Technical Institute StudentHealth Insurance plan. These types of plans are notconsidered comparable coverage by Massachusetts StateLaw, and you will be required to enroll in the ITT TechnicalInstitute Student Health Insurance Plan.EVERY STUDENT attending ITT Technical Institute MUSTrecord their medical insurance information. You must let usknow if you are enrolling in the Student Health Insurance Planoffered by ITT Technical Institute or if you prefer to waive thisplan. Please go to www.universityhealthplans.com forinformation on completing your waiver form. ALL STUDENTSmust record their waiver by July 12, 2014 in order to ensureyour bill accurately reflects your choice, and those enrolling in2Covered Injury means a bodily injury that is:1. Sustained by an Insured Person while he/she is insuredunder the Policy or the School’s prior policies; and2. Caused by and accident directly and independently of allother causes.Coverage under the School’s policies must have remainedcontinuously in force:1. From the date of Injury; and2. Until the date services or supplies are received, for them tobe considered as a Covered Medical Expense under thePolicy.3
Covered Medical Expense means those charges for anytreatment, service or supplies that are:1. Not in excess of the Usual and Reasonable charges;2. Not in excess of the charges that would have been madein the absence of this insurance; and3. Incurred while the Policy is in force as to the InsuredPerson, except with respect to any expenses payableunder the Extension of Benefits Provision.Covered Medical Expense includes those charges for treatment,services or supplies delivered in accordance with the healingpractices of Christian Science.Covered Sickness means Sickness, disease or trauma relateddisorder due to Injury which:1. Causes a loss while the Policy is in force; and2. Which results in Covered Medical Expenses.Elective Surgery or Elective Treatment means surgery ormedical treatment that is:1. Not necessitated by a pathological or traumatic change inthe function or structure of any part of the body; and2. Which occurs after the Insured Person’s effective date ofcoverage.Elective Treatment includes, but is not limited to, treatment foracne, warts and moles removed for cosmetic purposes, weightreduction, infertility, learning disabilities, routine physicalexaminations, fertility tests and pre-marital examinations,preventive medicines or vaccines except when required for thetreatment of Covered Injury or Covered Sickness to the extentcoverage is not required by state or federal law.Elective Surgery includes, but is not limited to, circumcision,vasectomy, breast reduction, sexual reassignment surgery,submucous resection and/or other surgical correction for adeviated nasal septum, other than for necessary treatment ofacute sinusitis to the extent coverage is not required by stateor federal law. Elective surgery does not include Plastic orCosmetic Surgery required to correct an abnormality causedby a Covered Injury or Covered Sickness.Emergency Medical Condition means a medical condition,which:1. Manifests itself by acute symptoms of sufficient severity(including severe pain); and2. Causes a prudent layperson, who possesses an averageknowledge of health and medicine, to reasonably expectthat the absence of immediate medical attention mightresult in:4a.Placing the health of the individual (or with respect toa pregnant woman, the health of the woman or herunborn child) in serious jeopardy;b. Serious impairment to bodily functions; orc. Serious dysfunction of any bodily organ or part.Essential Health Benefits mean benefits that are defined assuch by the Secretary of Labor and are to be provided in amanner that is equal to the scope of benefits provided under atypical employer plan. This applies to the following generalcategories and the items and services covered within thecategories:1. Ambulatory patient services;2. Emergency services;3. Hospitalization;4. Maternity and newborn care;5. Mental health and substance use disorder services,including behavioral health treatment;6. Prescription drugs;7. Rehabilitative and habilitative services and devices;8. Laboratory services;9. Preventive and wellness services and chronic diseasemanagement; and10. Pediatric services, including oral and vision care.Insured Person means a student of the Policyholder who iseligible and insured for coverage under the Policy.Loss means medical expense caused by Injury or Sickness andcovered by the Policy.Physician means a:1. Doctor of Medicine (M.D); or2. Doctor of Osteopathy (D.O); or3. Doctor of Dentistry (D.M.D. or D.D.S.); or4. Doctor of Chiropractic (D.C.); or5. Doctor of Optometry (O.D.); or6. Doctor of Podiatry (D.P.M.)Who is licensed to practice as such by the governmentalauthority having jurisdiction over the licensing of suchclassification of doctor in the state where the service isrendered.A Doctor of Psychology (Ph.D.) will also be considered aPhysician when he or she is similarly licensed or licensed as aHealth Care Provider. The services of a Doctor of Psychologymust be prescribed by a Doctor of Medicine.Physician will also mean any licensed practitioner of thehealing arts who We are required by law to recognize as a“Physician.” This includes an acupuncturist, a certified nursepractitioner, a certified nurse-midwife, a Physician’s assistant,5social workers and psychiatric nurses to the same extent thattheir services would be covered if performed by a Physician.Physician also includes Christian Science Practitioners listed inthe Christian Science Journal at the time the service is providedand who adheres to the rules and regulations of the First Churchof Christ, Scientist, Boston, Massachusetts.The term Physician does not mean any person who is anImmediate Family Member.Usual and Reasonable (U&R) means the normal charge, in theabsence of insurance, of the provider for a service or supply, butnot more than the prevailing charge in the area for a:1. Like service by a provider with similar training orexperience; or2. Supply that is identical or substantially equivalent.We, Our, or Us means National Guardian Life InsuranceCompany, or its authorized agents.You, Your, Yours means the insured student.SCHEDULE OF BENEFITSWhen initial medical treatment is received within 30 days of theoccurrence of a Covered Injury or the onset of a CoveredSickness the Policy will pay 80%, except as specifically stated,of Covered Medical Expenses incurred by an Insured Persondue to a Covered Sickness or Covered Injury for Domestic andInternational Students with J-1 visas. Covered MedicalExpenses are considered incurred on the date the treatment orservice is rendered or the supply is furnished. CoveredMedical Expenses are shown in the Schedule of Benefits.MANDATED BENEFITSState mandated benefits will be subject to all deductibles,Co-payments, co-insurance, limitations, or otherprovisions of the policy, unless specifically statedotherwise.Mandate Disclaimer: If any Preventive Services Benefit issubject to the mandated benefits required by state law, theywill be administered under the federal or state guideline,whichever is more favorable to the student.Autism Spectrum Disorder Benefit: We will providecoverage for the diagnosis and treatment of Autism SpectrumDisorder on the same basis as any other Covered Sickness.Treatment of Autism Spectrum Disorders includes thefollowing care prescribed, provided or ordered for an InsuredPerson diagnosed with one of the Autism Spectrum Disordersby a licensed Physician or a licensed psychologist: Habilitativeor Rehabilitative Care; Pharmacy Care, Psychiatric Care;6
Psychological Care and Therapeutic Care. For the purpose ofthis benefit:Autism Spectrum Disorders means any of the pervasivedevelopmental disorders as defined by the most recent editionof the Diagnostic and Statistical Manual of Mental Disorders,including autistic disorder, Asperger's disorder and pervasivedevelopmental disorders not otherwise specified.Applied Behavior Analysis means the design,implementation and evaluation of environmental modifications,using behavioral stimuli and consequences, to producesocially significant improvement in human behavior, includingthe use of direct observation, measurement and functionalanalysis of the relationship between environment andbehavior.Diagnosis of Autism Spectrum Disorders means theassessments, evaluations including neuropsychologicalevaluations, genetic testing or other tests to diagnose whetheran individual has one of the autism spectrum disorders.Habilitative or Rehabilitative Care means professionalcounseling and guidance services and treatment programs,including, but not limited to, Applied Behavior Analysissupervised by a board certified behavior analyst, that arenecessary to develop, maintain and restore, to the maximumextent practicable, the functioning of an individual. PharmacyCare means medications prescribed by a licensed Physicianand health-related services to determine the need oreffectiveness of the medications, to the same extent thatpharmacy care is provided by the policy for other medicalconditions.Therapeutic Care means services provided by licensed orcertified speech therapists, occupational therapists, physicaltherapists or social workers.Cancer Treatment Benefits: We will pay the Usual andReasonable expenses incurred for treatment of cancer asfollows:1. Bone Marrow Transplants for the Treatment of BreastCancer: We will pay the expenses incurred for a bonemarrow transplant or transplants for Insured Persons whohave been diagnosed for breast cancer that has progressedto metastatic disease, provided that the Insured Personmeets the criteria established by the MassachusettsDepartment of Public Health. These criteria will beconsistent with medical research protocols reviewed andapproved by the National Cancer Institute.2. Leukocyte Testing: We will pay the expenses incurred forthe cost of human leukocyte antigen testing or73.4.5.6.histocompatibility locus antigen testing that is necessary toestablish bone marrow transplant donor suitability. This willinclude the costs of testing for A, B, or DR antigens or anycombination thereof, consistent with rules, regulations andcriteria established by the Department of Public Health.Scalp Hair Prostheses: We will pay the expenses incurredfor scalp hair prostheses worn for hair loss suffered as aresult of the treatment of any form of cancer or leukemia. upto 500. Such coverage will be subject to a writtenprescription from the treating Physician and will be subject tothe same limitations and guidelines as any other prosthesisthat would be covered by the Policy.Clinical Trials for Cancer: We will pay the expensesincurred for Patient Care Services in connection with aqualified cancer clinical trial to the same extent as theywould be covered and reimbursed if the Insured Person didnot receive care in a Qualified Clinical Trial. Coverage for theservices required under this benefit are provided subject tothe terms and conditions generally applicable to otherbenefits provided under the Policy.Orally Administered Cancer Medications: We will pay theUsual and Reasonable expense incurred for prescribed,orally administered anticancer medications used to kill orslow the growth of cancerous cells on the same basis asintravenously administered or injected cancer medicationsthat are covered as medical benefits.Radiation Therapy and Chemotherapy – We will pay theUsual and Reasonable expenses incurred for prescribedx-ray therapy and chemotherapy. This coverageincludes: Radiation therapy using isotopes, radium, radon,or other ionizing radiation. X-ray therapy for cancer or when it is used inplace of surgery. Drug therapy for cancer (chemotherapy).For purposes of this benefit:Patient Care Service means a health care item or service thatis furnished to an Insured Person enrolled in a QualifiedClinical Trial, which is consistent with the standard of care forsomeone with the Insured Person’s diagnosis, is consistentwith the study protocol for the clinical trial, and would becovered if the Insured Person did not participate in the clinicaltrial. Patient Care Services does NOT include:1. An investigational drug or device but a drug or device thathas been approved for use in the Qualified Clinical Trial,whether or not the Food and Drug Administration has8approved the drug or device for use in treating the InsuredPerson's particular condition will be a patient care serviceto the extent that the drug or device is not paid for by themanufacturer, distributor or provider of the drug or device.2. Non-health care services that an Insured Person may berequired to receive as a result of being enrolled in theclinical trial.3. Costs associated with managing the research associatedwith the clinical trial.4. Costs that would not be covered for non-investigationaltreatments.5. Any item, service or cost that is reimbursed or otherwisefurnished by the sponsor of the clinical trial.6. The costs of services that are inconsistent with widelyaccepted and established national or regional standards ofcare.7. The costs of services that are provided primarily to meet theneeds of the trial, including, but not limited to, tests,measurements and other services that are typically coveredbut which are being provided at a greater frequency,intensity or duration.8. Services or costs that are not otherwise covered under thePolicy.Qualified Clinical Trial means a trial that meets the followingconditions:1. The clinical trial is intended to treat cancer in an InsuredPerson who has been so diagnosed.2. The clinical trial has been peer reviewed and is approvedby one of the United States National Institutes of Health, aqualified non-governmental research entity identified inguidelines issued by the National Institute of Health forcenter support grants, the United States Food and DrugAdministration pursuant to an investigational new drugexemption, the United States Department of Defense orVeterans Affairs, or with respect to Phase 11, III or IVclinical trials only, a qualified institutional review board.3. The facility and personnel conducting the trial are capableof doing so by virtue of their experience and training andtreat a sufficient volume of patients to maintain thatexpertise.4. With respect to Phase I clinical trials, the facility will be anacademic medical center or an affiliated facility and theclinicians conducting the trial will have staff privileges atsaid academic medical center.5. The Insured Person meets the patient selection criteriaenunciated in the study protocol for participation in theclinical trial.9
6.7.8.9.The Insured Person has provided informed consent forparticipation in the clinical trial in a manner that isconsistent with current legal and ethical standards.The available clinical or pre-clinical data provide areasonable expectation that the Insured Person’sparticipation in the clinical trial will provide a medical benefitthat is commensurate with the risks of participation in theclinical trial.The clinical trial does not unjustifiably duplicate existingstudies.The clinical trial must have a therapeutic intent and must ,to some extent, assess the effect of the intervention on theInsured Person.Cardiac Rehabilitation: We will pay the Usual andReasonable expenses incurred for cardiac rehabilitation.Cardiac rehabilitation shall mean multidisciplinary treatment ofan Insured Person with documented cardiovascular disease,which shall be provided in either a Hospital or other settingand which shall meet standards promulgated by theCommissioner of public health Benefits will include, but is notbe limited to, outpatient treatment which is to be initiated withintwenty-six (26) weeks after the diagnosis of such disease.Chiropractic Care Benefit: We cover chiropractic care whenperformed by a Doctor of Chiropractic (“Chiropractor”) or aPhysician in connection with the detection or correction bymanual or mechanical means of structural imbalance,distortion or subluxation in the human body for the purpose ofremoving nerve interference and the effects thereof, wheresuch interference is the result of or related to distortion,misalignment or subluxation of the vertebral column. Thisincludes assessment, manipulation and any modalities. Anynecessary laboratory tests will be covered in accordance withthe terms and conditions of the Policy. This coverage is limitedto 12 visits per Policy Year and only available to InsuredPersons over the age of 16.3.4.Orthodontic treatment and management;Preventative and restorative dentistry to ensure goodhealth;5. Adequate dental structures for orthodontic treatment orprosthetic management therapy, speech therapy,audiology and nutrition services.This benefit does not include payment for dental ororthodontic treatment not related to the management of thecongenital conditions of cleft lip and cleft palate.Cytologic Screening (pap smear) and MammographicExamination: We will pay the Usual and Reasonableexpenses incurred for cytologic screening and mammographicexamination. In the case of benefits for cytologic screening,benefits shall provide for an annual cytologic screening forwomen eighteen years of age and older; and in the case ofbenefits for mammographic examination benefits shall providefor a baseline mammogram for women between the ages ofthirty-five and forty and for a mammogram on an annual basisfor women forty years of age and older. If benefits are alsoprovided under the Preventive Services Benefit, We will payonly under one benefit. That will be the greater of the twobenefits.Cleft Palate and Cleft Lip Benefit: We will pay the Usualand Reasonable expenses incurred for an Insured Personunder the age of eighteen (18) for the cost of treatingcongenital conditions of cleft lip and cleft palate if suchservices are prescribed by the treating Physician or surgeon.Benefits are payable on the same basis as any other CoveredSickness.The coverage shall include benefits for:1. Medical, dental, oral and facial surgery;2. Surgical management and follow-up care by oral andplastic surgeons;Diabetes Equipment, Supplies and Service Benefit: We willpay the Usual and Reasonable expenses incurred for thefollowing equipment, supplies and services in the treatment ofdiabetes on the same basis as for any other CoveredSickness. Such equipment, supplies or service must beprescribed by a health care professional legally authorized toprescribe such items for the diagnosis or treatment of insulindependent, insulin-using, gestational and non-insulindependent diabetes.1. Equipment and supplies for the treatment of diabetesinclude, but are not limited to the following. We will pay theUsual and Reasonable charges incurred for such supplies:a. Lancets and automatic lancing devicesb. Glucose test stripsc. Blood glucose monitorsd. Blood glucose monitors for visually impairede. Control solutions used in blood glucose monitors;f. Diabetes data management systems formanagement of blood glucoseg. Urine testing products for glucose and ketonesh. Oral anti-diabetic agents used to reduce bloodsugar levelsi. Alcohol swabsj. Syringes1011k.Injection aids including insulin drawing up devicesfor the visually impairedl. Cartridges for the visually impairedm. Disposable insulin cartridges and pen cartridgesn. Insulin pumps and equipment for the use of thepump including batterieso. Insulin infusion devicesp. Oral agents for treating hypoglycemia such asglucose tablets and gelsq. Glucagon for injection to increase blood glucoseconcentrationr. Visual magnifying aids for use by the legally blinds. Voice synthesizers for blood glucose monitors foruse by the legally blindt. Other diabetes equipment and related supplies tothe treatment of diabetes2. We will pay the Usual and Reasonable charges for thefollowing:a. Insulin and prescribed oral diabetes medicationsthat influence blood sugar levels, on the samebasis as other Prescription Drugs;b. Laboratorytests,includingglycosylatedhemoglobin, or HbAlc, tests; anc. Therapeutic molded shoes and shoe inserts forpeople who have severe diabetic foot diseasewhen the need for therapeutic shoes and insertshas been certified by the treating Physician andprescribed by a podiatrist or other qualifiedPhysician and furnished by a podiatrist, orthotist,prosthetist or pedorthist.3. We will also pay Reasonable and Customary charges fordiabetes outpatient self-management education to ensurethat persons with diabetes are educated as to the properself-management and treatment of their diabetic condition,including medical nutrition therapy when provided by acertified diabetes health care provider. This benefit will belimited to visits where a Physician diagnoses a significantchange in the Insured Person's symptoms or conditionsthat necessitate changes in an Insured Person's selfmanagement or where reeducation or refresher educationis necessary.Coverage also includes home visits. Such education may beprovided by certified diabetes health care provider, whichmeans:a. A licensed health care professional with expertisein diabetes;b. A registered dietician; or12
c.A health care provider certified by the NationalCertification Board of Diabetes Educators as acertified diabetes educator.Early Intervention Services - We will pay the Usual andReasonable expenses incurred for the following treatment:1. The necessary care and treatment of medicallydiagnosed congenital defects and birth abnormalities, orpremature birth. Such coverage shall also include thosespecial medical formulas which are approved by thecommissioner of the Department of Public Health,prescribed by a Physician, and are provided inuria, maple syrup urine disease, propionicacidemia, or methylmalonic acidemia in infants andchildren or to protect the unborn fetuses of pregnantwomen with phenylketonuria. Such coverage will alsoinclude screening for lead poisoning as required by thecommonwealth of Massachusetts.2. Preventive and primary care services for children. Forthe purposes of this paragraph Preventive CareServices means services rendered to a dependent childof an Insured from the date of birth through theattainment of six years of age and shall include physicalexamination, history, measurements, sensory screening,neuropsychiatric evaluation and development screening,and assessment at the following intervals: six timesduring the child's first year after birth, three times duringthe next year, annually until age six. Such services shallalso include hereditary and metabolic screening at birth,appropriate immunizations, and tuberculin tests,hematocrit, hemoglobin or other appropriate blood tests,and urinalysis as recommended by the Physician.3. Early intervention services delivered by certified earlyintervention specialists, as defined in the earlyintervention operational standards by the Department ofPublic Health and in accordance with applicablecertification requirements. Such services shall beprovided by early intervention specialists who areworking in early intervention programs certified by theDepartment of Public Health, for children from birth untiltheir third birthday. [Reimbursement of costs for suchservices shall be part of a basic benefits packageoffered by Us or a third party, with a maximum benefit of 5,200 per year per child.4. Coverage for the cost of a newborn hearing screeningtest to be performed before the newborn infant is13discharged from the hospital or birthing center to thecare of the parent or guardian or as provided byregulations of the Department of Public Health.If the expense is also covered under the Preventive ServicesBenefit, We will pay only under one benefit. That will be thegreater of the two benefits.Fitness Benefit – We will reimburse an Insured Student up toa fixed amount in each Policy Year for each membership feepaid to a health club membership or for fitness classes at ahealth club. The total fitness benefit for a Policy Year is 150,which can represent any combination of fitness fees incurredduring the calendar year. The fitness benefit applies to feespaid for: privately-owned or privately-sponsored health clubsor fitness facilities, including individual health clubs and fitnesscenters; YMCAs; YWCAs; Jewish Community Centers; andmunicipal fitness centers. No fitness benefit is provided for anyfees or costs that pay for: country clubs; social clubs (such asski or hiking clubs); sports teams or leagues; spas;instructional dance studios; and martial arts schools.Hormone Replacement Therapy Services; OutpatientContraceptive Services: We will pay the Usual andReasonable expenses incurred for hormone replacementtherapy services for peri- and post-menopausal women andOutpatient Contraceptive Services under the same terms andconditions as for such other outpatient services.Outpatient Contraceptive Services: means consultations,examinations, procedures and medical services provided onan outpatient basis and related to the use of all contraceptivemethods to prevent pregnancy that have been approved bythe United States Food and Drug Administration.We will provide benefits for hormone replacement therapy forperi and post menopausal women and for outpatientprescription contraceptive drugs or devices which have beenapproved by the United States Food and Drug Administrationunder the same terms and conditions as for such otherprescription drugs or devices, provided that in covering all FDAapproved prescription contraceptive methods, nothing in thisbenefit precludes the use of closed or restricted formulary.Human Leukocyte Testing: We will pay the Usual andReasonable expenses incurred for the cost of humanleukocyte antigen testing or histo compatibility locus antigentesting that is necessary to establish bone marrow transplantdonor suitability. The coverage will include the costs of testingfor A, B or DR antigens, or any combination thereof, consistentwith rules, regulations and criteria established by theCommonwealth of Massachusetts.14Infertility Benefit: We will pay the Usual and Reasonableexpenses incurred for the diagnosis and treatment of infertilityto the same extent that benefits are provided for otherpregnancy-related procedures, We will pay the expensesincurred for:1. Artificial insemination (AI);2. In vitro fertilization and embryo placement (IVF-EP);3. Gamete intra fallopian transfer (GIFT);4. Sperm, egg and / or inseminated egg procurement andprocessing and banking of sperm or5. Inseminated eggs, to the extent such costs are not coveredby the donor’s insurer, if any;6. Intracytoplasmic sperm injection (ICSI) for the treatment ofmale factor infertility; or7. Zygote intrafallop
ITT Technical Institute . 2014-2015 . Underwritten by: National Guardian Life Insurance Company . Policy Number: 2014I5A31 . Effective: June 13, 2014 to June 12, 2015 . Group Number: S210306 . This health plan satisfies Minimum Creditable Coverage standardsand will satisfy the individual mandate that you have health insurance. Please