Transcription
Pressure Injury QualityImprovement StrategiesMARGARET WILBER, RN, BSNSHARON MOORE ANP-BC, WOCNBRIAN LEHMANOCTOBER 17, 2017
Pressure Injury Quality Improvement Strategies Catholic Health LIFE opened November 1, 2009Occurrence reporting-fallsFalls Performance Improvement Team2010 fall rate 19.51%2016 fall rate 12.34%
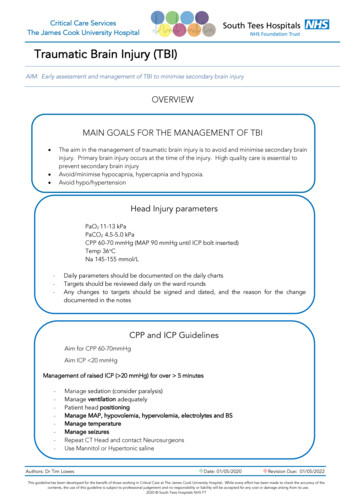
Pressure Injury With increasing enrollment there were increasedreported pressure injuries Factors driving LIFE to address this trend:1.Changes to Level II reporting in 2013, 2014 & 2015Level II Pressure Injuries LIFE Level II reports
2012 & 2014 CMS Survey Findings2. CMS audits resulted in findings for SDY04-ParticipantAssessment, which also drove the standardization of surveillanceand assessment CMS found that the Home Health Assessments werecompleted by the clinic nurse. CMS required the HomeHealth RN Assessment in the home after enrollmentincluding a skin check The corrective action plan included one assessment to becompleted by the community RN in the home and thesecond assessment to be completed by the Center RN This is in addition to the RN assessment completed atenrollment
Wound Performance Improvement TeamIn 2014 a Wound Performance Improvement Team was createdGOALS: Critically analyze the wound process and wound outcomesReview and analyze the rate of SNF vs. Communitypressure injuries for 2012 and 2013 to develop a reductionrate for 2014Nurse Practitioner to become wound certifiedDevelop a process to identify participants at risk uponadmission, when there is a decrease in mobility and upondischarge from a hospital or SNFDevelop interventions to address risk
Wound Performance Improvement TeamEarly Efforts Weekly Wound meeting Revise Skin Assessment & Pressure Injury PreventionPolicy & Procedure 2013 audit determined that the Braden Tool did notpredict risk, for those participants that developed apressure injury
Wound Performance Improvement TeamSystems and ProcessThe team: Developed a standardized nursing wound progress noteDeveloped standards of wound measurementDeveloped a consent form for wound photographyRevised the P & P:o All participants have a full RN assessment to include completion of theBraden Scale and PIPT at enrollment, 6 & 12 months or with a significantchange in conditiono Follow up home visits include a full skin examination, education, ensuring atreatment plan is in place including appropriate DMEo Once the participant has reached a 6 month reassessment without areoccurrence, the plan can be re-evaluated in concurrence with the PCP staffThese assessments enable the IDT to prioritize appropriatelyand aggressively care plan pressure injury risk and pressureinjury relieving interventions
Wound Performance Improvement TeamReintroduce Braden Risk assessment-validated risk assessmenttoolBraden tool reintroduced with educationand guidance from the LIFE WOCN NPDeveloped frequency of assessments basedupon Braden score:oooA score of 16 or greater-follow up visit every 6 monthsScore of 15 or 14-every 3 monthsScore of 13 or less and/or history of previous pressure injury-every month
Pressure Injury Prevention ToolThe Teamdeveloped aPressure InjuryPrevention Toolfor riskassessment andrecommendationsfor pressurerelief.
Policy and Procedure Algorithm
Wound Certification Sharon Moore ANP-BC became wound certified, providing educationand leadershipoEducated staff RN’s on pressure injury risk, staging, treatments,interventions, and education for the participants/caregiversoEducated and recognized the HHA’s as the front line prevention staffoCoordinated DME vendors to in-service staff on pressure relievingdevices to include mattresses, wheel chair cushions, Broda chairsoUrinary/bowel incontinence products, moisture wicking mattresspadsoEducated surgeons, wound specialists and infectious diseaseproviders on the PACE model of careoNP, RN’s and social work often attend appointments
Continuum of Care Process Improvements LIFE RN completes a weekly visit to the SNF toassess the participant’s pressure injury and tocomplete a case communication Pressure Injury Prevention Tool Utilized for SNF nursing case communications Faxed to the hospital for all LIFE admissions LIFE supplies DME to the SNF
Continuum of Care Challenges SNF challenges: Culture of resistance from the SNF staff Nursing staff unavailable to participate in case communications Agency staff Unavailability of the medical recordLIFE has: Gained access to the Catholic Health SNF EMR Developed some trust LIFE RN’s have developed some good working relationships inthe SNFThe SNF’s have become educated about the LIFE program over theyears
Process Improvements Staging and documentation inconsistencies-LIFE & SNFLIFE WOCN NP confirms the staging for any reportedStage III, IV or unstageable pressure injury-Level IIUpon discharge from the hospital, SAR or a respite staylonger than 3 days, the participant is brought directly tothe clinic for assessment and a complete skin check isperformedAllows clinical staff to address any skin issues that maynot have been known during the hospital, subacute orrespite stay
Database Development Weekly Wound Meeting-Excel spreadsheetutilized to track the progress of all open wounds Access database was developed in 2014 Track all wounds across the continuum ofcare By 2015 LIFE was outgrowing Access Additional reporting couldn’t be supported
Database Development 2015 LIFE began discussions with Emergencetek Group Points for discussion included: Capital Expenditure and Cost ApprovalHosting SolutionsLicenses for Third Party ComponentsSecurity – Access Rights to SoftwareIT Liaison to facilitate access to vendor for development
Database Development Much work was undertaken to create the new database:oooo Creating standard wound typesCreating standard anatomical structures & directionCreating standard treatmentsCreating standard interventionsAll wounds were mapped from the Access database intothe new databaseLIFE QA staff manually reviewed, verified and editedany insufficient mapping of 2015 and 2016 wounds intothe database
Outcomes 2016 Quarter 4-the weekly wound reportwas operational This enabled the ability to determinepressure injury rates for 2015 and 2016!!! Data driven processes
Pressure InjuriesLIFE Yearly Acquired Pressure Injury Rate(Includes all alTotalResults: In 2015 pressure injury acquisition rate among community participants was 2.89%; in 2016, 2.12%. In the SNFs the 2015 rate was 5.34%; compared to 3.21% in 2016. The 2015 hospital rate was 0%; 2.22% in 2016. There was no significant difference (P .05) among care site comparisons but the total reduction from 3.41%in 2015 to 2.45% in 2016 was statistically significant (P .05). The prevalence of pressure injury present at enrollment increased from 0.17% in 2015 to 0.38% in 2016 wasstatistically significant (P .05).
Weekly Wound Report
Metrics Report
Pressure Injury Graphs July 2016-July 2017
Add Wound
Add Status
Add Intervention
Add Treatment
Next Steps Determine if 2017 Wound Performance Improvement Team Goals have been met:Decrease the rate of newly developed pressure injuries by 25%.Prevent Stage II pressure injuries from progressing to Stage III,IV or Unstageable.Review and consider implementing Pressure Ulcer Scale forHealing (PUSH) toolDevelop Care Plan problem that encompasses all skininterventionsThe Braden Score and Tissue Type have been added to thedatabase for future reporting and implementation of the PUSHtool.
Wound Performance Improvement Team Systems and Process The team: Developed a standardized nursing wound progress note Developed standards of wound measurement Developed a consent form for wound photography Revised the P & P: o All participants have a full RN assessment to include completion of the