Transcription
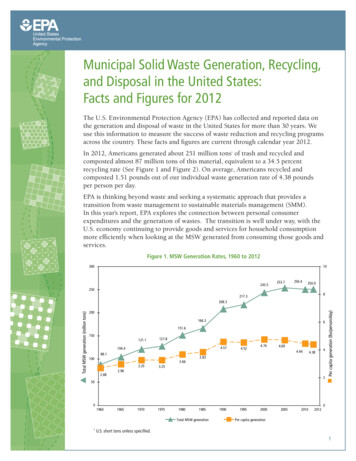
Environmental Science and Pollution CIRCULAR ECONOMY APPLICATION IN DESIGNING SUSTAINABLE MEDICAL WASTE MANAGEMENTSYSTEMSOptimization of medical waste recycling network consideringdisposal capacity bottlenecks under a novel coronaviruspneumonia outbreakXueyun Mei 1 & Hao Hao 1 & Yichen Sun 1 & Xinyang Wang 1 & Yanjun Zhou 1Received: 16 June 2021 / Accepted: 14 August 2021# The Author(s), under exclusive licence to Springer-Verlag GmbH Germany, part of Springer Nature 2021AbstractThe sudden outbreak and prolonged impact of the global novel coronavirus disease (COVID-19) epidemic has caused an increasein demand for medical products, such as masks and protective clothing, leading to an exponential increase in the generation ofmedical waste. As medical waste under the epidemic is highly infectious, it poses a great danger to human health. Therefore, withthe proliferation of medical waste, it has become crucial to construct a reverse logistics recycling network that can handle medicalwaste quickly and efficiently. In this study, we construct a multi-period medical waste emergency reverse logistics network sitingmodel with the objectives of minimum cost, minimum safety risk, and minimum time for the safe and quick disposal of medicalwaste. The model considers disposal capacity bottlenecks of existing facilities. Based on an empirical analysis using the COVID19 epidemic in New York City, USA, as a case study, we find that the use of a suitable number of synergistic facilities and theestablishment of temporary medical waste disposal centers are viable options for handling the dramatic increase in medical wasteduring the peak of the COVID-19 epidemic.Keywords Disposal capacity bottlenecks . COVID-19 . Mixed-integer nonlinear programming model . Emergency reverselogistics network . Third-order polynomial function . Safety riskIntroductionAccording to Johns Hopkins University, as of March 24, 2021,there are more than 124 million confirmed cases of coronavirusof novel disease (COVID-19) and more than 2.73 millionCOVID-19-related deaths worldwide. This unprecedented publichealth crisis has placed a high demand on the level of medicalcare worldwide. According to the WHO (2020), upgradinghealthcare delivery norms, large-scale research and developmentactivities, and continuous adaptation of public policies have become important initiatives in response to this crisis. It has beenaccompanied by an exponential increase in the amount of disposable masks, protective clothing, goggles, gloves, and manyResponsible Editor: Lotfi Aleya* Hao Haohehao8888@sina.com1School of Economics and Management, Shanghai PolytechnicUniversity, Shanghai 201209, Chinaother types of medical waste (Sharma et al. 2020). At the peak ofthe outbreak in China from February 15 to March 15, 2020,Wuhan generated nearly 247 tons of medical waste per day,nearly six times more than it generated before the outbreak(Singh et al. 2020). Novel coronaviruses can survive for dayson inanimate surfaces such as plastic, metal, and glass (Kampfet al. 2020). Failure to properly dispose of infectious medicalwaste not only poses a potential risk of environmental contamination to the government and the public (Hao et al. 2018a) butalso leads to the spread of infectious diseases such as AIDS,cholera, typhoid, and respiratory complications, as well as exacerbates the spread of COVID-19 (Sarkodie and Owusu 2021).The United Nations Basel Convention on TransboundaryMovements of Hazardous Wastes and their Disposal urges member states to treat medical waste generated during COVID-19 asan urgent and necessary public service event to minimize possible secondary effects on health and the environment (Singh et al.2020).In view of the dramatic increase in the amount of medicalwaste in a short period of time under the COVID-19 epidemic,
Environ Sci Pollut Resthis study establishes a medical waste recycling network considering bottlenecks in disposal capacity and aims to addressthe problem of siting medical waste recycling network facilities in an emergency situation. First, the network structure ofmedical waste recycling under the COVID-19 epidemic wasconstructed, including hospitals, sterilization transfer centers,domestic waste incineration centers (requisitioned), hazardouswaste incineration centers (requisitioned), newly constructedtemporary medical waste disposal centers, existing medicalwaste disposal centers, and harmless treatment centers.Second, based on the prediction of the number of patients inthe next 3 months using a third-order polynomial functionmodel, a multi-period medical waste emergency reverse logistics network siting model with the objectives of minimizingcost, minimizing safety risk, and minimizing time wasestablished. In this study, the network design takes into account the construction cost of new temporary medical wastedisposal centers set up to resolve disposal capacity bottlenecks, the acquisition cost of synergistic facilities such asincineration centers, the closure cost of new temporary medical waste disposal centers, and time urgency. It also regardstraditional economic cost indicators such as transportation,operation, disposal, and disinfection costs according to thehighly infectious nature of the medical waste. Taking intoconsideration all these costs and capacity bottlenecks, themodel determines the appropriate location and flow rate inthe medical waste recycling network.The contributions of this study are as follows: (1) a genericemergency reverse logistics recycling network model adaptedto infectious diseases is proposed. (2) The characteristics ofthe growth of medical waste amount during the COVID-19epidemic period are considered. The construction and closurecost of new temporary medical waste disposal centers andsterilization transfer centers, the cost of collaborative disposalsuch as the requisition of incineration centers, and time urgency are estimated. (3) Taking into consideration the actual situation, the requisition of domestic waste incineration centers,hazardous waste incineration centers, and other synergisticfacilities to dispose of medical waste reduces the constructionand closure costs of new temporary medical waste disposalcenters, while shortening the time to build new facilities andreducing the risk of infection. (4) Minimize safety risks including transportation and operation facility risks. (5)Through an empirical study of medical waste disposal underthe COVID-19 outbreak in New York City, USA, the validityof the model is verified, and some management insights areprovided to managers.The rest of the paper is organized as follows: Based onthe introduction of the literature review, the current statusof research on reverse logistics networks is presented.Next, the model construction of the article is presented.Then based on the model built, an empirical analysis aswell as a sensitivity analysis is conducted with New YorkCity, USA, as an example. Finally, the article issummarized.Literature reviewThis study focuses on four aspects: reverse logistics networkplanning, emergency response network, medical waste reverse logistics recycling network, and emergency medicalwaste reverse logistics network under the COVID-19 epidemic. We will review related research on these aspects.In terms of reverse logistics network planning, Stock(1992) first proposed the concept of reverse logistics, whichis broadly defined to include all logistics activities related toresource conservation, recycling, replacement, reuse of materials, and disposal. Due to the lack of natural resources, environmental factors, and government regulations related todiscarded products, recycling of products and materials is agrowing concern (Wang et al. 2019a). Fleischmann et al.(2001) summarized the commonalities of product recyclingreverse logistics and constructed a generalized facility sitingmodel; he suggested that product recycling is largelydependent on the environment. Hao et al. (2017) proposedthe concept of “fifth profit source,” pointing out that the development of reverse logistics should focus not only on theeconomic benefits, but also on the environmental and socialbenefits, so as to promote the sustainable development ofenterprises and realize circular economy. Sun and Da (2009)considered government subsidies, transportation discountproblems, fixed cost saving rates, and minimum recoveryrates, and used them to construct a mixed-integer nonlinearprogramming model. Choudhary et al. (2015) integrated thecarbon footprint throughout the integrated forward and reverse logistics network, and established a mixed-integer programming model with the objective of minimizing the totalcost. Ene and Öztürk (2015) and Xiao et al. (2019) establisheda multi-period mixed-integer programming model with theobjectives of cost minimization and environmental impactminimization to solve the siting problem of end-of-life vehiclerecycling network facilities. Zhou et al. (2015) constructed amulti-period multi-objective dynamic mixed-integer programming model by considering the social and economic benefits.Amin and Baki (2017) constructed a multi-objective mixedinteger programming model considering environmental factors, consumer markets, and recycling quantity uncertaintyproblems. Hajiaghaei-Keshteli and Fathollahi Fard (2018)constructed a multi-objective mixed-integer nonlinear programming model considering price discounts and index evaluation of sustainability to achieve a balanced maximization ofeconomic, social, and environmental benefits. Most of thecurrent reverse logistics network designs use mixed-integerprogramming models and some focus on green and social
Environ Sci Pollut Resbenefits; however, few models consider the safety and riskaspects.With the frequent occurrence of natural disasters and publichealth events, emergency logistics networks have graduallybecome a focus of considerable research attention. However,there has been almost no research on emergency reverse logistics. Emergency logistics is mainly applied in various crisismitigation activities such as pre-disaster rescue facility siteselection, post-disaster material transportation distribution,and casualty transportation (Caunhye et al. 2012). RezaeiMalek et al. (2016) considered the storage time of predisaster perishable food and the uncertainty of demand quantity at each demand point, and constructed a new integratednetwork model to determine the location at which perishablecommodity is required and quantity of storage in the predisaster period. Zhang et al. (2019) constructed a three-stagestochastic programming model with the objectives of minimizing transportation cost, unmet demand, andtransportation time to solve the problems of facility locationand resource allocation caused by primary and secondarydisasters. Liu et al. (2020a) used influenza A (H1N1) in theJiangsu province as an example and established an epidemicemergency logistics network optimization model based onservice level. To design this model, they integrated themobility characteristics of the population of the epidemicarea, the population density characteristics of differentepidemic areas, the secondary ring prevention strategy ofgovernment departments, the service radius limitation ofemergency distribution, and other realistic factors.In terms of medical waste reverse logistics recycling networks, Budak and Ustundag (2017) constructed a multi-product, multi-period mixed-integer linear programming modelwith the objective of cost minimization based on differenttypes of medical waste. Alizadeh et al. (2020) developed aclosed-loop supply chain model with the objectives of profitmaximization, transport distance, and time minimizationbased on the infectious nature of medical waste and thecapacity limitation of sterilization centers. Kargar et al.(2020a) constructed a multi-period mixed-integer linear programming model with the objectives of minimizing cost,selecting the best processing technology, and minimizing thetotal amount of medical waste stored in hospitals. The modelwas designed considering the problem of siting and routing ofmedical waste recycling network facilities under uncertainconditions. Wang et al. (2019b) developed a multi-objectivemulti-period mixed-integer programming model to solve theproblem of siting medical waste recycling facilities by considering economic and environmental benefits. Huo and Guo(2020) constructed a sustainable medical waste recycling network with the objectives of minimizing cost, minimizing environmental impact, and maximizing social benefits in view ofthe uncertainty, multi-periodicity, and pollution of medicalwaste recycling. Expired drugs are also medical waste thatcan cause great harm to the human body and theenvironment. Wang and Huang (2015) considered the choicebehavior of residents and introduced the incentive of government subsidy to recycling enterprises and recycling enterprises to residential areas; they constructed a bi-level programming model for the reverse logistics network of expired drugs.Jing and Chen (2015) constructed a reverse logistics networkplanning model for expired drugs with the objective of minimizing the total cost. Cao et al. (2017) constructed a multiperiod pharmaceutical reverse logistics network linkage model considering carbon emissions to solve the problem ofrecycling expired drugs or used medical devices; they usedgenetic algorithms for case analysis. Ahlaqqach et al. (2020)developed a closed-loop supply chain model for pharmaceuticals with mixed-integer nonlinear programming with the objectives of maximizing economic benefits, creating the mostjobs, and minimizing transportation risks. From the aforementioned literature, it can be seen that most of the current studieson medical waste consider economic, environmental, multiproduct, and uncertainty factors and construct mixed-integerprogramming models. In this aspect too, it can be observedthat very few studies have considered the possible infectionrisk (safety risk) of transportation and operation facilitiesbased on the infectious characteristics of medical waste.In terms of the medical waste reverse logistics networkunder the COVID-19 epidemic, Tirkolaee et al. (2021) hypothesized that time windows play a key role in prioritizinghospital services in different risk ranges. They developed amixed-integer linear programming model with the objectivesof minimum transport time, minimum total number of peopleviolating the time windows, and minimum number of peoplein waste disposal facilities. Liu et al. (2020b) developed a twostage model considering environmental, traffic, and vehicleload factors for the problem of selecting temporary storagecenters for medical waste and actual transportation flow.Kargar et al. (2020b) considered all sites where medical wastemay be generated in Babol city and developed a model withthe objectives of minimizing cost, risk of transportation anddisposal facilities, and amount of uncollected waste. Yu et al.(2020) constructed a multi-period mixed-integer programming model with the objectives of minimizing cost, risk atsource, and risk at transportation and operation facilities usingthe Wuhan City COVID-19 epidemic as a study. The resultsshowed that the installation of temporary incinerators and other equipment could effectively handle the surge of medicalwaste.From a review of the aforementioned literature, it can beconcluded that the reverse logistics network optimization generally adopts a mixed-integer programming model; currentnetwork optimization models often adopt the multi-objectivemulti-period mixed-integer programming model. Over theyears, these models have gradually started considering theeconomic, environmental, and social benefits to achieve the
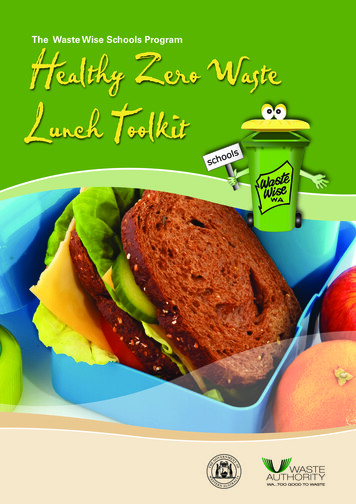
Environ Sci Pollut Reseffective unification of social, environmental, and economicbenefits (Hao et al. 2020). Owing to the outbreak of SARS,COVID-19, and other public health emergencies, the researchdirection has gradually turned to medical waste, but there isless research on the construction of medical waste networksunder the COVID-19 epidemic. Additionally, there is almostno network that considers the actual situation ofcommandeering existing domestic waste incineration centersand hazardous waste incineration centers as synergistic disposal facilities.In this study, with the objectives of minimizing cost, safetyrisk, and time, we consider the cost of disinfection of medicalwaste reverse logistics recycling and closure andrequisitioning synergistic facilities such as domestic wasteincineration centers and hazardous waste incineration centers.The construction cost of new temporary medical waste disposal centers, the probability of accidental risk during transportation, the probability of accidental risk at each facility, thepopulation of exposures, time urgency, and other various factors are also considered. A multi-objective multi-periodmixed-integer nonlinear programming model is constructedconsidering the bottlenecks of disposal capacity to determinethe location of each facility and the amount of medical wasteallocated to each facility. A case study of medical waste disposal in New York City, USA, is also presented.Model assumptionsThe assumptions made while designing this model are asfollows:(1) All waste generated by the hospital was transported tothe sterilization transfer center.(2) Because the risk of the waste residues after treatment atthe disposal centers or incineration centers is minimizedand can be safely stored, transported, and disposed, therisk of storage, transportation, and disposal to the harmless treatment centers is not taken into account in themixed-integer nonlinear programming model.(3) In the case of an emergency, medical waste can betransported to the domestic waste incineration centerfor treatment; its treatment volume will not exceed 5%of the disposal capacity of the domestic waste incineration center. The maximum disposal capacity of medicalwaste in a hazardous waste incineration center is determined according to the spare capacity that can be deployed in the facility.(4) The medical waste recycling treatment regarded in thisstudy mainly considers medical waste generated by medical institutions; it does not consider hospital waste isolated at home.ModelModel buildingProblem definitionFacility pointsThe objective of this study is to design a medical wasterecycling network that resolves the bottlenecks of disposalcapacity during the COVID-19 epidemic. The main infrastructures of this network are hospitals, sterilization transfercenters, existing medical waste disposal centers, domesticwaste incineration centers (requisitioned), hazardous wasteincineration centers (requisitioned), newly constructed temporary medical waste disposal centers, and harmless disposalcenters as shown in Figure 1. The hospital sends the medicalwaste generated under the COVID-19 epidemic to the hospital’s storage room for temporary storage after specializedtreatment. The waste will then be transported by special vehicles to the medical waste disposal center for correspondingtreatment. At the beginning of the COVID-19 epidemic, allmedical waste were sent to existing medical waste disposalcenters for treatment because of the small amount of medicalwaste. When the amount of medical waste generated increaseddramatically, priority was given to the requisition of emergency co-disposal facilities such as domestic waste incinerationcenters and hazardous waste incineration centers (Yang et al.2021), after which a newly constructed temporary medicalwaste disposal center was considered.i—set of hospitals i {1, 2 . . I}j—set of sterilization transfer centers j {1, 2 . . J}d—set of domestic waste incineration centers(requisitioned) d {1, 2 . . D}h—set of hazardous waste incineration centers(requisitioned) h {1, 2 . . H}t—set of newly constructed temporary medical waste disposal centers t {1, 2 . . T}e—set of existing medical waste disposal centers e {1,2 . . E}l—set of harmless disposal centers l {1, 2 . . L}p—set of periods p {1, 2 . . P}Model parametersFC pj —fixed cost of establishing sterilization transfer centers jduring period pFC pd —fixed cost of domestic waste incineration centers drequisitioned during period p
Environ Sci Pollut ResDomestic waste incineration center(requisitioned)Hazardous Waste Incineration Center(requisitioned)HospitalHarmless Treatment CenterSterilization transfer centerNewly constructed temporary medical wastedisposal centerExisting medical waste disposal centerFig. 1 Medical waste reverse logistics recycling and treatment network under the COVID-19 epidemicFC ph —fixed cost of hazardous waste incineration centers hrequisitioned during period pFC pt —fixed costs of newly constructed temporary medicalwaste disposal centers t during period pfcpj —fixed costs of closure of sterilization transfer centers jin period pfcpt —fixed costs of closure of newly constructed temporarymedical waste disposal centers t during period pOC pj —operating costs of sterilization transfer centers jduring period pOC pd —operating costs of domestic waste incineration centers (requisitioned) d during period pOC ph —operating costs of hazardous waste incinerationcenters (requisitioned) h during period pOC pt —operating costs of newly constructed temporarymedical waste disposal centers t during period pOC pe —operating cost of existing medical waste disposalcenters e during period pTC pj —unit disposal cost of sterilization transfer centers jduring period pTC pd —unit disposal cost of domestic waste incinerationcenters (requisitioned) d during period pTC ph —unit disposal cost of hazardous waste incinerationcenters (requisitioned) h during period pTC pt —unit disposal cost of newly constructed temporarymedical waste disposal centers t during period pTC pe —unit disposal cost of existing medical waste disposalcenters e during period pDC pj —disinfection cost of sterilization transfer centers jduring period pCApj —maximum processing capacity of sterilization transfer centers j during period pCApd —maximum processing capacity of domestic wasteincineration centers (requisitioned) d during period pCAph —maximum processing capacity of hazardous wasteincineration centers (requisitioned) h during period pCApt —maximum processing capacity of newly constructed temporary medical waste disposal centers t during period pCApe —maximum processing capacity of existing medicalwaste disposal centers e during period pTDij—distance from hospital i to sterilization transfer center jTDjd—distance from the sterilization transfer center j to thedomestic waste incineration center (requisitioned) dTDjh—distance from the sterilization transfer center j tohazardous waste incineration center (requisitioned) hTDjt—distance from the sterilization transfer center j tonewly constructed temporary medical waste disposal center tTDje—distance from the sterilization transfer center j toexisting medical waste disposal center eCCij—unit transportation cost from hospital i to sterilization transfer center jCCjd—unit transportation cost from sterilization transfercenter j to domestic waste incineration center (requisitioned) dCCjh—unit transportation cost from sterilization transfercenter j to hazardous waste incineration center(requisitioned) h
Environ Sci Pollut ResCCjt—unit transportation cost from sterilization transfercenter j to newly constructed temporary medical waste disposal center tCCje—unit transportation cost from sterilization transfercenter j to existing medical waste disposal center eMPj—maximum number of sterilization transfer centers jconstructedMPd—maximum number of domestic waste incinerationcenters (requisitioned) dMPh—maximum number of hazardous waste incinerationcenters (requisitioned) hMPt—maximum number of newly constructed temporarymedical waste disposal centers tARj—probability of accidental risk in sterilization transfercenter jARd—probability of accidental risk in domestic waste incineration center (requisitioned) dARh—probability of accidental risk in hazardous waste incineration center (requisitioned) hARt—probability of accidental risk in newly constructedtemporary medical waste disposal center tARe—probability of accidental risk in existing medicalwaste disposal center eWRij—probability of accidental risk during transportationfrom hospital i to sterilization transfer center jWRjd—probability of accidental risk during transportationfrom sterilization transfer center j to domestic waste incineration center (requisitioned) dWRjh—probability of accidental risk during transportationfrom sterilization transfer center j to hazardous waste incineration center (requisitioned) hWRjt—probability of accidental risk during transportationfrom sterilization transfer center j to newly constructed temporary medical waste disposal center tWRje—probability of accidental risk during transportationfrom sterilization transfer center j to existing medical wastedisposal center ePPj—number of sterilization transfer centers j populationexposedPPd—number of domestic waste incineration centers(requisitioned) d population exposedPPh—number of hazardous waste incineration centers(requisitioned) h population exposedPPt—number of newly constructed temporary medicalwaste disposal centers t population exposedPPe—number of existing medical waste disposal centers epopulation exposedWPij—population exposure in transit from hospitali to sterilization transfer center jWPjd—population exposure in transit from the sterilizationtransfer center j to domestic waste incineration center(requisitioned) dWPjh—population exposure in transit from sterilizationtransfer center j to hazardous waste incineration center(requisitioned) hWPjt—population exposure in transit from the sterilizationtransfer center j to the newly constructed temporary medicalwaste disposal center tWPje—population exposure in transit from sterilizationtransfer center j to existing medical waste disposal center eCQpi —amount of medical waste generated by hospital iduring period pPT pi —number of patients accepted by hospital i duringperiod pq—amount of medical waste generated per capita in hospital iObjective functionsHere, the construction of a medical waste recycling networkmodel is presented considering disposal capacity bottlenecksunder the COVID-19 epidemic with the objectives of minimizing cost, safety risk, and time.minF ¼ C þ Z þ Wð1ÞC ¼ C1 þ C2 þ C3 þ C4 þ C5 þ C6ð2ÞZ ¼ Z1 þ Z2ð3ÞW ¼ p P i I j J X pj TDij þ p P j J d D X pd :TDjd þ p P j J h H X ph :TDjh þ p P j J t T X pt :TDjtð4Þþ p P j J e E TDje :X peC1 ¼þX pj X p 1þ1j2 j J p P FC pj : d D p P FC pd :!X pd X p 1d þ12!!X ph X p 1h þ1þ2!X pt X p 1þ1ptþ t T p P FC t :2ð5Þ h H p P FC ph :C2 ¼ j J p P fcpj :jþ!X pj X p 1j 1j2 t T p P fcpt :j!X pt X p 1t 1j2ð6Þ
Environ Sci Pollut ResC 3 ¼ j J p P OC pj X pj þ j J p P TC pj HQpj þ d D p P OC pd X pd þ d D p P TC pd HQpd þ h H p P OC ph X ph þ h H p P TC ph HQph þ t T p P OC pt X pt þ t T p P TC pt HQpt þ e E p P OC pe X pe þ e E p P TC pe HQpeð7ÞC4 ¼C5 ¼ i I j J p P DC pj TQpij i I j J p P TDij TQpij CC pijþð8Þ j J d D p P TDjd TQpjd CC pjdþ j J h H p P TDjh TQpjh CC pjh þ j J t T p P TDjt TQpjt CC pjtð9Þþ j J e E p P TDje TQpje CC pjeZ 1 ¼ i I j J p P WRij WPij TQpij þ j J d D p P WR jd WPjd TQpjdþ j J h H p P WRjh WPjh TQpjh þ j J t T p P WRjt WPjt TQpjtð10Þþ j J e E p P WRje WPje TQpjeZ 2 ¼ j J p P AR j PP j HQpj þ d D p P ARd PPd HQpdþ h H p P ARh PPh HQph þ t T p P ARt PPt HQptð11Þþ e E p P ARe PPe HQpeObjective function (1) represents the overall objective ofthis study, which is to achieve the minimum cost, safety risk,and time. Objective function (2) represents the minimum costof medical waste in each period. Equation (5) represents thesum of the fixed costs of construction and requisition of facil p p 1 X X þ1ity sites in each period. Here, j J p P FC pj : j 2jrepresents the fixed costs of the sterilization transfer centers, p p 1 X X þ1represents the fixed costs of the d D p P FC pd : d 2ddomestic waste incineration centers (requisitioned), h H p P p p 1 X X þ1FC ph : h 2hrepresents the fixed costs of the hazardouswaste incineration centers (requisitioned), and t T p P FC pt : p p 1 X t X t þ1represents the fixed cost of the newly constructed2temporary medical waste disposal centers t.Equation (6) represents the sum of the fixed costs of closingthe facility sites in each period, where j J p P fcpj :j p p 1 X j X j 1j represents the closing costs of the sterilization2 p p 1 X X 1transfer centers and t T p P fcpt :j t 2tj represents theclosing costs of newly constructed temporary medical wastedisposal centers.Equation (7) represents the sum of operating and disposalcosts for each period. Here, j J p P OC pj X pj represents theoperating costs of the sterilization transfer centers, j J p PTC pj HQpj represents the disposal costs of the sterilization transfer centers, d D p P OC pd X pd represents the operating costs ofthe domestic waste incineration centers (requisitioned), d D p P TC pd HQpd represents the disposal costs of the domesticwaste incineration centers (requisitioned), h H p P OC ph X phrepresents the operating costs of the hazardous waste incineration centers (requisitioned), h H p P TC ph HQph representsthe disposal costs of the hazardous waste incineration centers(requisitioned), t T p P OC pt X pt represents the operatingcosts of the newly constructed temporary medical waste disposal center, t T p P TC pt HQpt represents the disposal costsof the newly constructed temporary medical waste disposalcenter, e E p P OC pe X pe represents the operating costs ofthe existing medical waste disposal centers, and e E p P TC peHQpe represents the disposal cost of the existi
tics network siting model with the objectives of minimizing cost, minimizing safety risk, and minimizing time was established. In this study, the network design takes into ac-count the construction cost of new temporary medical waste disposal centers set up to resolve disposal capacity bottle-