Transcription
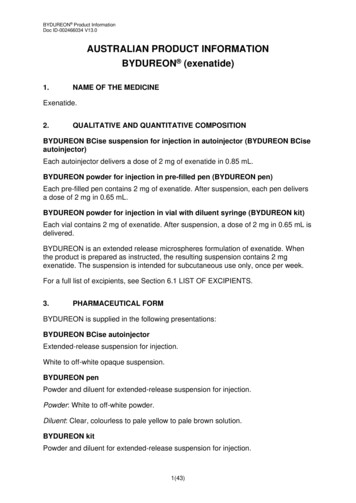
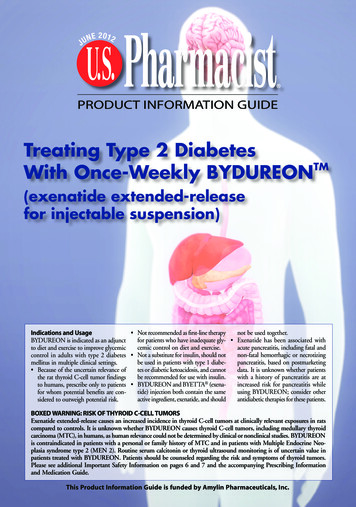
JUNE 2012 PRODUCT INFORMATION GUIDETreating Type 2 DiabetesWith Once-Weekly BYDUREONTM(exenatide extended-releasefor injectable suspension) Not recommended as first-line therapynot be used together.Indications and Usagefor patients who have inadequate gly- Exenatide has been associated withBYDUREON is indicated as an adjunctcemic control on diet and exercise.acute pancreatitis, including fatal andto diet and exercise to improve glycemicnon-fatal hemorrhagic or necrotizingcontrol in adults with type 2 diabetes Not a substitute for insulin, should notbe used in patients with type 1 diabepancreatitis, based on postmarketingmellitus in multiple clinical settings.tes or diabetic ketoacidosis, and cannotdata. It is unknown whether patients Because of the uncertain relevance ofbe recommended for use with insulin.with a history of pancreatitis are atthe rat thyroid C-cell tumor findingsincreased risk for pancreatitis whileto humans, prescribe only to patients BYDUREON and BYETTA (exenatide) injection both contain the sameusing BYDUREON; consider otherfor whom potential benefits are conactive ingredient, exenatide, and shouldantidiabetic therapies for these patients.sidered to outweigh potential risk.BOXED WARNING: RISK OF THYROID C-CELL TUMORSExenatide extended-release causes an increased incidence in thyroid C-cell tumors at clinically relevant exposures in ratscompared to controls. It is unknown whether BYDUREON causes thyroid C-cell tumors, including medullary thyroidcarcinoma (MTC), in humans, as human relevance could not be determined by clinical or nonclinical studies. BYDUREONis contraindicated in patients with a personal or family history of MTC and in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). Routine serum calcitonin or thyroid ultrasound monitoring is of uncertain value inpatients treated with BYDUREON. Patients should be counseled regarding the risk and symptoms of thyroid tumors.Please see additional Important Safety Information on pages 6 and 7 and the accompanying Prescribing Informationand Medication Guide.This Product Information Guide is funded by Amylin Pharmaceuticals, Inc.
Treating Type 2 DiabetesWith Once-WeeklyBYDUREONTM(exenatide extended-releasefor injectable suspension)BackgroundThe discovery of a group of guthormones called incretins hasspurred the development of a classof incretin-based medications forthe treatment of type 2 diabetesmellitus (T2DM). The pathogenesis of T2DM is complex and classically associated with progressivebeta-cell failure (relative insulindeficiency) and insulin resistancein fat and muscle cells.1 Glucosehomeostasis is known, however, tobe maintained by complex interactions involving insulin, glucagon,and the incretin hormones. Thelatter are released by enteroendocrinecells in the gut in response to mealingestion. Incretin dysfunction,along with a number of other important physiological defects, have beenimplicated in the pathogenesis ofT2DM. Incretin-based therapies,aimed at restoring incretin activityin people with T2DM, have beenshown to be effective therapies inthis population.Despite an increasing recognitionof the importance of reaching glycemic goals and a greater emphasison diabetes care, only 55% of adultswith T2DM achieved a glycosylatedhemoglobin (A1C) below 7.0%,according to the National Healthand Nutrition Examination Survey(NHANES).2 Furthermore, even inpatients that are compliant withtheir medications, the benefits oflifestyle interventions and oral hypoglycemic therapy may not be durable, which is likely due to the progressive nature of the disease.3 Asnoted above, traditional models ofT2DM disease progression haveemphasized the core defects ofperipheral insulin resistance,increased hepatic gluconeogenesis,and progressive loss of pancreaticbeta-cell function (resulting in insulin deficiency).4 These changes makethe pathophysiology of T2DM quitecomplex.4Incretin-Based MedicationsFirst identified in the 1960s, the“incretin effect” showed that insulin secretion is greater in responseto the oral intake of a meal whencompared to intravenous glucoseadministration.5,6 Subsequently, theincretin effect was shown to be dueprimarily to the secretion of twoincretin hormones: glucagon-likepeptide-1 (GLP-1) and glucosedependent insulinotropic polypeptide (GIP).7 Combined, these 2hormones account for 70% ofinsulin secretion following glucoseingestion.8 The effects of GLP-1are mediated by binding of thehormone to GLP-1 receptors. 9GLP-1 has been shown to stimulateglucose-dependent insulin secretion,suppress glucagon secretion, slowgastric emptying, and decreasecaloric intake.10 Insulin release inresponse to GLP-1 is glucose-dependent, meaning that insulin releaseis stimulated only when blood glucose levels are elevated, and insulinsecretion decreases as blood glucoselevels approach normal. CirculatingGLP-1 is short-lived, with a half-lifeof less than 2 minutes due to itsrapid degradation by the enzymedipeptidyl peptidase-4 (DPP-4).11The incretin response is disruptedin people with T2DM. Studies haveshown, however, that the administration of exogenous GLP-1 iscapable of correcting this defect.12In early clinical studies involvingpatients with T2DM, continuousexposure to GLP-1 demonstratedimproved glycemic control mimicking that of healthy subjects.13,14 Theclinical utility of natural GLP-1 isPlease see Important Safety Information on pages 6 and 7, and the accompanying Prescribing Information and Medication Guide.PHG1201U.S. PHARMACIST JUNE 20122
Treating Type 2 Diabetes With Once-Weekly BYDUREON (exenatide extended-release for injectable suspension)limited, however, by its rapid degradation by the DPP-4 enzyme.Two treatment approaches havethus far been developed to overcomethese limitations: GLP-1 receptoragonists, which provide a pharmacologic dose of GLP-1 analogdesigned to resist DPP-4 degradation, and DPP-4 inhibitors, whichslow the inactivation of endogenousincretin hormones by inhibitingthe DPP-4 enzyme. Clinically,DPP-4 inhibitors are oral therapiesthat can improve post-prandialinsulin secretion and are generallyweight neutral.15 The injectableGLP-1 receptor agonists have demonstrated efficacy in terms of stimulating glucose-dependent insulinsecretion and are also capable ofinducing weight loss in people withT2DM.15 BYDUREON (exenatideextended-release for injectable suspension) is a GLP-1 receptor agonist that is indicated as an adjunctto diet and exercise to improve glycemic control in adults with T2DMin multiple clinical settings.BYDUREON carries a boxed warning for potential risk of thyroidC-cell tumors, including medullarythyroid carcinoma. Because of theuncertain relevance of the rat thyroid C-cell tumor findings tohumans, BYDUREON is not recommended as first-line therapy forpatients uncontrolled on diet andexercise alone.16deliver a controlled release of exenatide (FIGURE 1). The microspheresare composed of polylactide coglycolide acid polymer, which hasbeen used in other therapeutic applications to encapsulate small molecules, peptides, and proteins.17Immediately following subcutaneous injection, the BYDUREONmicrospheres aggregate, and exenatide at or near the surface of themicrospheres diffuses. Over time,as the microspheres degrade, exenatide is continuously released intothe circulation. The microspherepolymer is completely metabolizedand eliminated as carbon dioxideand water.17 This process results ina controlled release of exenatide fora continuous presence of GLP-1receptor activation. Once steadystate is achieved, therapeutic levelsof exenatide are maintained withonce-weekly dosing.Pharmacokinetic profile ofBYDUREON. Following initiationof once-weekly BYDUREON, plasmalevels gradually increase over 6 to 7weeks. Steady-state levels of exenatideare maintained thereafter with onceweekly dosing. After 2 weeks oftherapy, decreases in fasting plasmaglucose (FPG) are observed in patientswith T2DM, and by week 14 (theearliest time point at which it wasexamined), post-prandial glucose(PPG) levels also improve.18,19Clinical efficacy. Efficacy datafrom a 24-week, randomized, openlabel clinical trial compared theaddition of BYDUREON 2 mgQW (n 129) to BYETTA (exenatide) injection 10 mcg BID (n 123) in adults with T2DM inadequately controlled on lifestyleintervention and/or oral antidiabetictherapy (metformin, SFU, thiazolidinedione, or a combination of any2 of these agents).20 Study participants in the BYDUREON andBYETTA arms had an average baseline (BL) A1C of 8.5% and 8.4%,respectively, and weighed an averageof 213.8 lb and 207.9 lb, respectively.The average duration of T2DMwas 7 years for both treatmentgroups. Participants treated withBYDUREON experienced a meanA1C reduction of 1.6% comparedto a mean reduction of 0.9% forthose receiving BYETTA (P .001).Additionally, the proportion ofpatients reaching an A1C of 7%was 58% in the BYDUREONarm vs 30% in the BYETTA arm(P .001). BYDUREON treatment was also associated with a reduction in mean FPG of -25 mg/dL at24 weeks compared to a mean reduction of -5 mg/dL in the BYETTAgroup. And although BYDUREONis not indicated for weight loss,BYDUREON: A New ApproachTo T2DM TreatmentMicrosphere technology. BYDUREONis the first once-weekly GLP-1 receptor agonist approved in the UnitedStates for the treatment of T2DM.BYDUREON utilizes patentedbiodegradable microspheres toFigure 1. Mechanism of release usingMedisorb Technology (Alkermes, Inc.).Please see Important Safety Information on pages 6 and 7, and the accompanying Prescribing Information and Medication Guide.U.S. PHARMACIST JUNE 20123
Treating Type 2 Diabetes With Once-Weekly BYDUREON (exenatide extended-release for injectable suspension)BYDUREON patients lost an average of 5.1 lb, which was similar toBYETTA (exenatide) injection(3.1 lb).BYDUREON has also beenstudied in 2 separate 26-week clinical trials vs Januvia (sitagliptin), aDPP-4 inhibitor that is administeredas a once-daily oral agent. In thefirst trial, T2DM patients withinadequate glycemic control onmetformin alone were randomizedto receive BYDUREON 2 mg QW(n 160) or the maximum approveddose of Januvia (100 mg QD; n 166).21 Patients in the BYDUREONarm experienced a mean A1C reduction of 1.5% from a BL of 8.6%vs 0.9% for Januvia patients (BL 8.5%; P .0001). Patients in theBYDUREON arm lost a mean 5.1lb while the Januvia group lost amean 1.8 lb (P .0002). As a secondary endpoint, 62% ofBYDUREON patients achieved anA1C goal of 7% vs 35% for Januvia. In the second trial, patientswith T2DM who were drug-naïvewere randomized to receiveBYDUREON or Januvia.22 A meanA1C reduction of 1.5% was achievedin the BYDUREON arm, withparticipants in the Januvia armachieving a mean A1C reductionof 1.2% (P .001).22 Additionally,as secondary endpoints, patients inthe BYDUREON arm lost 4.4 lbwhile those receiving Januvia lost1.8 lb (P .001), and 64% ofpatients achieved an A1C goal of 7% vs 46% for Januvia.Collectively, clinical trial datawith BYDUREON demonstratedimprovements in glycemic control,and although not indicated forweight loss, participants receivingBYDUREON treatment realized adecrease in their weight on average.SafetyBoxed Warning. Exenatide extendedrelease causes thyroid C-cell tumorsat clinically relevant exposures inrats. Because of the uncertain relevance of the rat thyroid C-celltumor findings to humans,BYDUREON is not recommendedas first-line therapy for patientsinadequately controlled on dietand exercise.Contraindications. BYDUREONis contraindicated in patients witha personal or family history of medullary thyroid carcinoma (MTC)and in patients with Multiple Endocrine Neoplasia syndrome type 2(MEN 2). Additionally, BYDUREONis contraindicated for use in patientswith known hypersensitivity toexenatide or any components ofthe formulation.Warnings. Cases of pancreatitis in peopleusing exenatide have beenreported, including fatal and nonfatal hemorrhagic or necrotizingpancreatitis. BYDUREON shouldbe discontinued promptly if pancreatitis is suspected and shouldnot be restarted if a diagnosis ofpancreatitis is made. Likewise,other antidiabetic therapies shouldbe considered in individuals witha history of pancreatitis. There is an increased risk ofhypoglycemia when BYDUREONis used in combination with asulfonylurea. If initiatingBYDUREON in an individualon sulfonylurea therapy, considerreducing the sulfonylurea dose. Postmarketing reports of renalimpairment have been reportedwith exenatide. BYDUREONis not recommended in patientswith severe renal impairment orend-stage renal disease and shouldbe used with caution in thosewith renal transplantation ormoderate renal impairment. B YDUREON is not recommended in individuals with severegastrointestinal disease, such asgastroparesis. Postmarketing reports of serioushypersensitivity reactions withexenatide have been reported. Insuch cases, BYDUREON shouldbe discontinued in addition toany other suspected medicationsand medical advice should besought promptly. Clinical studies establishing conclusive evidence of macrovascular risk reduction have not beenperformed with BYDUREONor any other antidiabetic drug.Adverse ReactionsSome of the most frequently reportedadverse events associated withBYDUREON in clinical trials werenausea, diarrhea, headache, andvomiting. Nausea was generallymild and tended to decrease overtime. While nausea was the mostcommon side effect withBYDUREON therapy, the incidencewas less than was seen with twicedaily BYETTA. In the 24-weekclinical trial of BYDUREON vsBYETTA, the rates of nausea were14% and 35%, respectively.16 In aseparate 30-week clinical trial vsBYETTA, rates of nausea were 27%vs 34%.16 Injection-site reactions(itching, redness) are more commonin BYDUREON-treated patientsvs patients receiving comparatorinjections. In addition, small, asymptomatic, subcutaneous injection-sitePlease see Important Safety Information on pages 6 and 7, and the accompanying Prescribing Information and Medication Guide.U.S. PHARMACIST JUNE 20124
Treating Type 2 Diabetes With Once-Weekly BYDUREON (exenatide extended-release for injectable suspension)nodules are seen with the use ofBYDUREON. These are consistentwith the known properties of themicrospheres used in BYDUREONand typically resolve within 3 to 6weeks. In clinical trials, there wereno reports of major hypoglycemia,although the risk of minor hypoglycemia was increased with concomitant SFU use.Administration & DosingBYDUREON is administered onceevery 7 days (weekly) at any timeof day, independent of meals.BYDUREON is administered asa subcutaneous injection in theabdomen, thigh, or upper armregions. Patients should be counseled to use a different injectionsite each week when injecting inthe same regions. The steps foradministration are straightforward(connect, shake, and inject; seeFIGURE 2), and BYDUREON isintended for patient self-administration. BYDUREON is providedin cartons containing 4 single-dosetrays; the trays should be storedunder refrigeration.BYDUREON inT2DM TreatmentA cornerstone of the ADA guidelines for pharmacologic treatmentof T2DM is the timely augmentation of therapy with additionalagents in order to achieve andmaintain individualized A1Cgoals.23 The 2012 Position Statement from the ADA and the European Association for the Study ofDiabetes (EASD) advocates for a“patient-centered” approach totreatment and emphasizes not onlyglucose-lowering efficacy, but alsopotential side effects, weight reduc-Figure 2. BYDUREON administration steps.tion, and cost as important considerations when choosing therapeutic agents. 24 Treatment withmetformin is recommended formost patients at or soon after diagnosis, followed by dual-therapy ifglyceimic goals are not being metafter 3 months. When progressing to dual-therapy, the ADA/EASDrecommends adding 1 of 5 secondline agents: SFU, TZD, a GLP-1receptor agonist like BYDUREON,DPP-4 inhibitor, or basal insulin.Choice is based on patient anddrug characteristics, with the overriding goal of improving glycemiccontrol while minimizing sideeffects. GLP-1 receptor agonistsare recommended as an option foradd-on therapy to metformin dueto their efficacy in terms of A1Creduction, potential for weightloss, and low risk of hypoglycemia.24The American Association ofClinical Endocrinologists/AmericanCollege of Endocrinology (AACE/ACE) recommends a GLP-1 receptor agonist, like BYDUREON, asa preferred agent for combinationtherapy (ie, add-on to metformin,or metformin plus an SFU or athiazolidinedione) in patients notmeeting glycemic goals with monotherapy due to its low risk of hypoglycemia when not used with anSFU and the potential to provideweight loss.25 The continuous glycemic control provided withBYDUREON, along with thepotential for weight loss and lowrisk of hypoglycemia, are meaningful considerations for achievingtreatment goals in patients withT2DM. Please see Important Safety Information on pages 6 and 7, and the accompanying Prescribing Information and Medication Guide.U.S. PHARMACIST JUNE 20125
IMPORTANT SAFETY INFORMATION for BYDUREON TM (exenatide extended-release for injectable suspension)BOXED WARNING: RISK OFTHYROID C-CELL TUMORSExenatide extended-release causesan increased incidence in thyroidC-cell tumors at clinically relevantexposures in rats compared to controls. It is unknown whetherBYDUREON (exenatide extendedrelease for injectable suspension)causes thyroid C-cell tumors, including medullary thyroid carcinoma(MTC), in humans, as human relevance could not be determinedby clinical or nonclinical studies.BYDUREON is contraindicatedin patients with a personal or family history of MTC and in patientswith Multiple Endocrine Neoplasiasyndrome type 2 (MEN 2). Routineserum calcitonin or thyroid ultrasound monitoring is of uncertainvalue in patients treated withBYDUREON. Patients should becounseled regarding the risk andsymptoms of thyroid tumors. Contraindications B YDUREON is contraindicatedin patients with known priorsevere hypersensitivity reactionsto exenatide or to any of theproduct components.Warnings and Precautions B ased on postmarketing data,exenatide has been associatedwith acute pancreatitis, including fatal and non-fatal hemorrhagic or necrotizing pancreatitis. After initiation ofBYDUREON, observe patientscarefully for pancreatitis (persistent severe abdominal pain,sometimes radiating to theback, with or without vomiting). If pancreatitis is suspected, BYDUREON should be discontinued promptly andshould not be restarted if pancreatitis is confirmed. Increased risk of hypoglycemiawhen used in combination withglucose-independent insulinsecretagogues (eg, sulfonylureas).Clinicians may consider reducing the sulfonylurea (SFU) dose. Should not be used in patientswith severe renal impairmentor end-stage renal disease. Usewith caution in patients withrenal transplantation or moderate renal failure. Postmarketingreports of altered renal functionwith exenatide, includingincreased serum creatinine, renalimpairment, worsened chronicrenal failure, and acute renal failure, sometimes requiring hemodialysis and kidney transplantation. Not recommended in patientswith severe gastrointestinal disease (eg, gastroparesis). Patients may develop antibodiesto exenatide. In 5 registrationtrials, attenuated glycemicresponse was associated in 6%of BYDUREON-treated patientswith antibody formation. Ifworsening of or failure to achieveadequate glycemic controloccurs, consider alternative antidiabetic therapy. Postmarketing reports of serioushypersensitivity reactions (eg,anaphylaxis and angioedema).If this occurs, patients shoulddiscontinue BYDUREON andother suspect medications andpromptly seek medical advice. No clinical studies establishingconclusive evidence of macrovascular risk reduction withBYDUREON or any other antidiabetic drug.U.S. PHARMACIST JUNE 20126Withdrawals I n 5 comparator-controlled, 24to 30-week BYDUREON trials,the incidence of withdrawal dueto adverse events was 4.9% forBYDUREON, 4.9% forBYETTA (exenatide) injection,and 2.0% for other comparators.The most common adverse reactions leading to withdrawal forBYDUREON, BYETTA, andcomparators respectively were:nausea (0.5%,1.5%, 0.3%);injection-site nodule (0.5%,0.0%, 0.0%); diarrhea (0.3%,0.4%, 0.3%); injection-site reaction (0.2%, 0.0%, 0.0%); andheadache (0.2%, 0.0%, 0.0%).One percent of BYDUREONpatients withdrew due to injection-site adverse reactions.Adverse Reactions ( 5%) B YDUREON vs BYETTA:24-week trial, nausea (14% vs35%), diarrhea (9.3% vs 4.1%),injection-site erythema (5.4%vs 2.4%); 30-week trial, nausea(27% vs 33.8%), diarrhea(16.2% vs 12.4%), vomiting(10.8% vs 18.6%), injection-sitepruritus (18.2% vs 1.4%), constipation (10.1% vs 6.2%),gastroenteritis viral (8.8% vs5.5%), gastroesophageal refluxdisease (7.4% vs 4.1%), dyspepsia (7.4% vs 2.1%), injectionsite erythema (7.4% vs 0.0%),fatigue (6.1% vs 3.4%), headache (6.1% vs 4.8%), injectionsite hematoma (5.4% vs 11.0%). BYDUREON vs titrated insulin glargine: nausea (12.9% vs1.3%), headache (9.9% vs7.6%), diarrhea (9.4% vs 4.0%),injection-site nodule (6.0% vs0.0%).
IMPORTANT SAFETY INFORMATION for BYDUREON TM (exenatide extended-release for injectable suspension) C ombination trial vs sitagliptinand pioglitazone: nausea (24.4%vs 9.6% and 4.8%), diarrhea(20.0% vs 9.6% and 7.3%),vomiting (11.3% vs 2.4% and3.0%), headache (9.4% vs 9.0%and 5.5%), constipation (6.3%vs 3.6% and 1.2%), fatigue(5.6% vs 0.6% and 3.0%),dyspepsia (5.0% vs 3.6% and2.4%), decreased appetite (5.0%vs 1.2% and 0.0%), injectionsite pruritus (5.0% vs 4.8%and 1.2%). Monotherapy trial vs sitagliptin,pioglitazone, and metformin:nausea (11.3% vs 3.7%, 4.3%,and 6.9%), diarrhea (10.9% vs5.5%, 3.7%, and 12.6%),injection-site nodule (10.5%vs 6.7%, 3.7%, and 10.2%),constipation (8.5% vs 2.5%,1.8%, and 3.3%), headache(8.1% vs 9.2%, 8.0%, and12.2%), dyspepsia (7.3% vs1.8%, 4.9%, and 3.3%). Injection-site reactions wereobserved more frequently inBYDUREON-treated patients(17.1%) vs patients treated withBYETTA (12.7%), titrated insulin glargine (1.8%), or placeboinjection (6.4%-13.0%). Injection-site reactions were observedin 14.2% of antibody-positivepatients vs 3.1% of antibodynegative patients, with higherincidence in those with highertiter antibodies. BYETTA-treatedpatients had similar incidencebetween antibody-positive andantibody-negative patients (5.8%vs 7.0%). Small, asymptomatic,subcutaneous injection-site nodules are seen with the use ofBYDUREON.Hypoglycemia N o major hypoglycemia wasreported for BYDUREON- orcomparator-treated patients infive 24- to 30-week trials.Minor hypoglycemia incidencesfor BYDUREON vs comparator-treated patients were asfollows: 24-week trial vsBYETTA: with SFU, 12.5%vs 11.8%; without SFU, 0.0%for both; 30-week trial vsBYETTA: with SFU, 14.5%vs 15.4%; without SFU, 0.0%vs 1.1%; monotherapy trial vssitagliptin, pioglitazone, andmetformin: 2.0% vs 0.0% (allcomparators); combination trialvs sitagliptin and pioglitazone:1.3% vs 3.0% and 1.2%; vstitrated insulin glargine, withSFU, 20.0% vs 43.9%; without SFU, 3.7% vs 19.1%.U.S. PHARMACIST JUNE 20127Drug Interactions B YDUREON slows gastric emptying and can reduce the rateof absorption of orally administered drugs. Use with cautionwith oral medications. P ostmarketing repor ts ofincreased international normalized ratio (INR) sometimesassociated with bleeding withconcomitant use of warfarin.Monitor INR frequently untilstable upon initiation or alteration of BYDUREON.Use in Specific Populations B ased on animal data,BYDUREON may cause fetalharm and should be used duringpregnancy only if the potentialbenefit justifies the potentialrisk to the fetus. C aution should be exercisedwhen administered to a nursingwoman. Use in pediatric patients is notrecommended as safety andeffectiveness have not beenestablished.For complete safety profile andother important prescribingconsiderations, see the accompanying Prescribing Informationand Medication Guide.
REFERENCES1. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care.2010;33(suppl 1):S62-S69.2. Ford ES. Trends in the control of risk factors for cardiovascular disease among adults with diagnosed diabetes: findings from the National Health and NutritionExamination Survey 1999-2008. J Diabetes. In press.3. Campbell RK, White JR Jr. More choices than everbefore: emerging therapies for type 2 diabetes. Diabetes Educ. 2008;34(3):518-534.4. DeFronzo RA. Banting Lecture. From the triumvirate to the ominous octet: a new paradigm for thetreatment of type 2 diabetes mellitus. Diabetes.2009;58(4):773-795.5. Elrick H, Stimmler L, Hlad CJ Jr, Arai Y. Plasmainsulin response to oral and intravenous glucoseadministration. J Clin Endocrinol Metab.1964;24:1076-1082.6. Nauck MA, Homberger E, Siegel EG, et al. Incretin effects of increasing glucose loads in man calculated from venous insulin and C-peptide responses. JClin Endocrinol Metab. 1986;63(2):492-498.7. Drucker DJ, Nauck MA. The incretin system: glucagon-like peptide-1 receptor agonists and dipeptidylpeptidase-4 inhibitors in type 2 diabetes. Lancet.2006;368(9548):1696-1705.8. Vilsbøll T, Holst JJ. Incretins, insulin secretion andtype 2 diabetes mellitus. Diabetologia.2004;47(3):357-366.9. Mayo KE, Miller LJ, Bataille D, et al. InternationalUnion of Pharmacology. XXXV. The glucagon receptor family. Pharmacol Rev. 2003;55(1):167-194.10. Holst JJ, Vilsbøll T, Deacon CF. The incretin sys-tem and its role in type 2 diabetes mellitus. Mol CellEndocrinol. 2009;297(1-2):127-136.11. Ahrén B. DPP-4 inhibitors. Best Pract Res ClinEndocrinol Metab. 2007;21(4):517-533.12. Amori RE, Lau J, Pittas AG. Efficacy and safety ofincretin therapy in type 2 diabetes: systematic reviewand meta-analysis. JAMA. 2007;298(2):194-206.13. Rachman J, Barrow BA, Levy JC, Turner RC.Near-normalisation of diurnal glucose concentrationsby continuous administration of glucagon-like peptide-1 (GLP-1) in subjects with NIDDM. Diabetologia. 1997;40(2):205-211.14. Zander M, Madsbad S, Madsen JL, Holst JJ.Effect of 6-week course of glucagon-like peptide 1 onglycaemic control, insulin sensitivity, and beta-cellfunction in type 2 diabetes: a parallel-group study.Lancet. 2002;359(9309):824-830.15. Campbell RK, Miller S. New therapeutic horizons:mapping the future of glycemic control with incretinbased therapy. Diabetes Educ. 2009;35(5):731-747.16. BYDUREON [package insert]. San Diego, CA:Amylin Pharmaceuticals, Inc; 2012.17. Medisorb microspheres technology. BiotechInvestWeb site. http://www.biotechinvest.net/uploads/Medisorb.pdf. Accessed November 17, 2011.18. Kim D, MacConell L, Zhuang D, et al. Effects ofonce-weekly dosing of a long-acting release formulation of exenatide on glucose control and body weightin subjects with type 2 diabetes. Diabetes Care.2007;30(6):1487-1493.19. Drucker DJ, Buse JB, Taylor K, et al. Exenatideonce weekly versus twice daily for the treatment oftype 2 diabetes: a randomised, open-label, non-inferiority study. Lancet. 2008;372(9645):1240-1250.20. Blevins T, Pullman J, Malloy J, et al. DURATION-5: exenatide once weekly resulted ingreater improvements in glycemic control compared with exenatide twice daily in patients withtype 2 diabetes. J Clin Endocrinol Metab.2011;96(5):1301-1310.21. Bergenstal RM, Wysham C, MacConell L, et al;for DURATION-2 Study Group. Efficacy and safetyof exenatide once weekly versus sitagliptin or pioglitazone as an adjunct to metformin for treatment oftype 2 diabetes (DURATION-2): a randomised trial.Lancet. 2010;376(9739):431-439.22. Russell-Jones D, Cuddihy RM, Hanefeld M, et al;for DURATION-4 Study Group. Efficacy and safetyof exenatide once weekly versus metformin, pioglitazone, and sitagliptin used as monotherapy in drugnaive patients with type 2 diabetes (DURATION-4):a 26-week double-blind study. Diabetes Care.2012;35(2):252-258.23. American Diabetes Association. Standards ofmedical care in diabetes—2012. Diabetes Care.2012;35(suppl 1):S11-S63.24. Inzucchi SE, Bergenstal RM, Buse JB et al. Position Statement of the American Diabetes Associationand the European Association for the Study of Diabetes. Management of hyperglycemia in type 2 diabetes:a patient-centered approach [published online aheadof print April 19, 2012]. Diabetes Care.25. Rodbard HW, Jellinger PS, Davidson JA, et al.Statement by an American Association of ClinicalEndocrinologists/American College of Endocrinologyconsensus panel on type 2 diabetes mellitus: an algorithm for glycemic control. Endocr Pract.2009;15(6):540-559.COUNSELING CORNERThe following series of questions and answers serves as a patienteducation aid to assist healthcare professionals in counseling patientswith type 2 diabetes who have been prescribed BYDUREON(exenatide extended-release for injectable suspension).Q. How does BYDUREONwork all week? Medicine is contained inmicrospheres Microspheres release medicinecontinuously over time Medicine works only when bloodsugar levels are highQ. When do I take BYDUREON? Once every 7 days on the sameday each week Any time of the day, with orwithout foodQ. If I have to change myDosing Day, how do I do that? New Dosing Day must be atleast 3 days after your last dose Do not take 2 doses ofBYDUREON less than 3 days apartQ. What are the most commonside effects? Nausea is most common;usually occurs at the start oftreatment and should decreaseover time for most patients Diarrhea, vomiting, andconstipation Itching or redness at injection site Small, raised bump within 2 to 4weeks of injecting BYDUREON,which may not be visible to thenaked eye and should go away onits own within 3 to 6 weeksQ. What are some of theserious side effects? Potential increased risk ofthyroid tumors I nflammation of the pancreas(pancreatitis) Low blood sugar (hypoglycemia) Kidney problems (renalimpairment) Stomach problems (gastrointestinaldisease) Allergic reaction (hypersensitivity)Q. What cha
be recommended for use with insulin. BYDUREON and BYETTA (exena-tide) injection both contain the same active ingredient, exenatide, and should not be used together. Exenatide has been associated with acute pancreatitis, including fatal and non-fatal hemorrhagic or necrotizing pancreatitis, based on postmarketing data.