Transcription
National Heart, Lung, and Blood InstituteEducation Strategy Development WorkshopChronic ObstructivePulmonary DiseaseU.S. DEPARTMENT OF HEALTH AND HUMAN SERVICESNational Institutes of HealthNational Heart, Lung, and Blood Institute
National Heart, Lung, and Blood InstituteEducation Strategy Development WorkshopChronic ObstructivePulmonary DiseaseU.S. DEPARTMENT OF HEALTH AND HUMAN SERVICESNational Institutes of HealthNational Heart, Lung, and Blood InstituteAdministrative Use OnlyDecember 2005
ContentsWorkshop Participants. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .vExecutive Summary . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .ixIntroduction. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .1Presentations—Wednesday, September 22, 2004 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .3How Strategy Development Workshops Have ShapedNHLBI’s National Education Programs? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .4Why a Strategy Development Workshop on COPD Is Needed? . . . . . . . . . . . . . . . . . . .4COPD Education and Awareness: What Is Needed? . . . . . . . . . . . . . . . . . . . . . . . . . . .5What Do Patients, Families, and At-Risk Individuals Need To Know? . . . . . . . . . . . . . . .8Moving Forward Through Translation and Communication . . . . . . . . . . . . . . . . . . . . . . .8The Current Environment: Management and Treatment . . . . . . . . . . . . . . . . . . . . . . . . .8The Current Environment: Early Detection and Diagnosis . . . . . . . . . . . . . . . . . . . . . . .10The Role of Patient Advocacy Organizations in COPD Awareness and Education . . . .11Risk Factors for COPD Other Than Tobacco . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .12Tobacco as a Risk Factor for COPD . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .13Panel Discussions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .15I. Living With COPD—Motivators and Barriers for Patients . . . . . . . . . . . . . . . . . . . . . .15II. Treating COPD—Facilitators and Barriers for Health Professionals . . . . . . . . . . . . . .16Presentations—Thursday, September 23, 2004 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .19Best Practices for Developing a National COPD Education Program . . . . . . . . . . . . . .20Defining Needs and Opportunities . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .21Small Group Breakout SessionsGroup 1: Target Audience:Group 2: Target Audience:Group 3: Target Audience:. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .22Health Care Professionals . . . . . . . . . . . . . . . . . . . . . . . . .22At-Risk and Early-Stage Patients . . . . . . . . . . . . . . . . . . .22Patients With Established and Advanced Disease . . . . . .23Appendices . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .25A. Agenda for Education Strategy Development Workshopon Chronic Obstructive Pulmonary Disease . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .26Wednesday, September 22, 2004 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .26Thursday, September 23, 2004 . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .28B. Questions for Small Group Discussions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .30For More Information . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .inside back coverContentsiii
Workshop ParticipantsWorkshop CochairsHomer A. Boushey, M.D.Immediate Past PresidentAmerican Thoracic SocietyProfessor of Medicine, Department of MedicineUniversity of California, San FranciscoSan Francisco, CAJohn W. WalshPresident, CEO, and CofounderAlpha-1 FoundationMiami, FLFacilitatorGeorge I. Balch, Ph.D.Balch AssociatesOak Park, ILParticipantsMichael Ader, M.D.Medical Director, Respiratory CareHanover HospitalHanover, PAWilliam Bailey, M.D.Professor of Medicine and DirectorLung Health CenterUniversity of Alabama at BirminghamBirmingham, ALSidney S. Braman, M.D.Professor of MedicineBrown Medical SchoolProvidence, RIA. Sonia Buist, M.D.Professor of MedicineOregon Health and Science UniversityPortland, ORRichard Casaburi, M.D., Ph.D.Director, Pulmonary Function, Respiratory, andCritical Care Physiology and MedicineLos Angeles County HarborUCLA Medical CenterTorrance, CADeborah ChaseChase CommunicationsNew York, NYRon CookEmphysema Foundationfor Our Right To SurviveMorrow, GAGerard J. Criner, M.D.Professor of MedicineTemple Lung CenterTemple UniversityPhiladelphia, PAPam DeNardoEmphysema Foundationfor Our Right To SurviveSt. Charles, ILDennis E. Doherty, M.D., F.C.C.P.Chief, Division of Pulmonaryand Critical Care MedicineMedical Director, Respiratory Care ServicesUniversity of KentuckyChandler Medical CenterLexington, KYJames E. DouglasCOPD InternationalLexington, KYJanet DouglasLexington, KYWorkshop Participantsv
Gary Ferguson, M.D.DirectorPulmonary Research Instituteof Southeast MichiganLivonia, MIChip GatchellNashua, NHBarbara M. Kaplan, M.P.H., C.H.E.S.Manager, Adult Lung Disease ProgramsAmerican Lung AssociationWashington, DCSuzanne Lareau, R.N., M.S.Pulmonary Clinic Nurse SpecialistNew Mexico VA Health Care SystemAlbuquerque, NMAudrey G. Gift, Ph.D., R.N., F.A.A.N.Professor and Associate DeanCollege of NursingMichigan State UniversityEast Lansing, MIGretchen Lawrence, R.R.T.AssociateNational Lung Health Education ProgramDallas, TXPhyllis Greenberger, M.S.W.President and CEOSociety for Women’s Health ResearchWashington, DCMargaret Lester, R.N., M.S.N., F.N.P.Director of Educational ProgramsNational Respiratory Training CenterRaleigh, NCLawrence Grouse, M.D., Ph.D.Executive DirectorU.S. COPD CoalitionGig Harbor, WAAmy Maggio, M.S.Managing Editor, COPD DigestCOPD FoundationChicago, ILLeslie A. Hoffman, Ph.D., R.N., F.A.A.N.Professor and Chair,Department of Acute/Tertiary CareUniversity of Pittsburgh School of NursingPittsburgh, PABarry Make, M.D.Director, Pulmonary RehabilitationNational Jewish Medical and Research CenterDenver, COAnne M. HolbrookSenior Educational Learning SpecialistSPRY FoundationWashington, DCSuzanne S. Hurd, Ph.D.Scientific DirectorGlobal Initiative for Chronic ObstructiveLung Disease (GOLD)Gaithersburg, MDFernando J. Martinez, M.D., M.S.Professor of MedicinePulmonary and Critical Care MedicineUniversity of MichiganAnn Arbor, MIRay Masferrer, R.R.T.Associate Executive DirectorAmerican Association for Respiratory CareIrving, TXRonald Moolenaar, M.D., M.P.H.EpidemiologistCenters for Disease Control and PreventionAtlanta, GAviChronic Obstructive Pulmonary Disease
Sydney Parker, Ph.D.Vice President, Development and OutreachAmerican College of Chest PhysiciansNorthbrook, ILKatherine PruittAssistant Vice President, Program ServicesAmerican Lung AssociationWashington, DCJohn J. Reilly, M.D.Associate Professor of MedicineClinical DirectorPulmonary and Critical Care MedicineBrigham and Women’s HospitalHarvard Medical SchoolBoston, MAKen RichmondFairfax Station, VAVlady Rozenbaum, Ph.D.COPD AlertSilver Spring, MDRobert Sandhaus, M.D., Ph.D.Professor of MedicineNational Jewish Medical and Research CenterDenver, COE. Neil Schachter, M.D.Professor of MedicineMount Sinai Medical CenterNew York, NYFrank Sciurba, M.D.Associate Professor of MedicineDivision of Pulmonary, Allergy,and Critical Care MedicineUniversity of Pittsburgh School of MedicinePittsburgh, PAEdwin K. Silverman, M.D., Ph.D.Assistant Professor of MedicineBrigham and Women’s HospitalHarvard Medical SchoolBoston, MAStuart Stoloff, M.D.Clinical ProfessorFamily and Clinical MedicineUniversity of Nevada School of MedicineCarson City, NVByron Thomashow, M.D.Clinical Professor of MedicineColumbia UniversityNew York, NYNorbert Voelkel, M.D.ProfessorUniversity of Colorado Health Sciences CenterDenver, COBarbara P. Yawn, M.D., M.Sc., F.A.A.F.P.NHLBI LiaisonAmerican Academy of Family PhysiciansAssistant Editor, Patient Centered Care for COPDDirector of ResearchOlmstead Medical CenterRochester, MNWorkshop Participantsvii
NHLBI Staff MembersDouglas BoydInternational Program OfficerOffice of International ProgramsNational Heart, Lung, and Blood InstituteThomas L. Croxton, M.D.Medical OfficerDivision of Lung DiseasesNational Heart, Lung, and Blood InstituteLawrence Friedman, M.D.Acting Deputy DirectorNational Heart, Lung, and Blood InstituteRobinson Fulwood, Ph.D., M.S.P.H.Senior Manager for Public HealthProgram DevelopmentOffice of Prevention, Education, and ControlNational Heart, Lung, and Blood InstituteJames P. Kiley, Ph.D.DirectorDivision of Lung DiseasesNational Heart, Lung, and Blood InstituteGregory J. Morosco, Ph.D., M.P.H.Associate Director for Prevention, Education,and ControlNational Heart, Lung, and Blood InstituteviiiChronic Obstructive Pulmonary DiseaseNancy J. Poole, M.B.A.Senior Manager for Program OperationsOffice of Prevention, Education, and ControlNational Heart, Lung, and Blood InstituteSusan T. Shero, R.N., M.S.Public Health AdvisorOffice of Prevention, Education, and ControlNational Heart, Lung, and Blood InstituteLenee N. Simon, M.P.H.Community Health SpecialistOffice of Prevention, Education, and ControlNational Heart, Lung, and Blood InstituteEllen K. Sommer, M.B.A.Public Health AdvisorOffice of Prevention, Education, and ControlNational Heart, Lung, and Blood InstituteJuliana J. Tu, M.S.Community Health SpecialistOffice of Prevention, Education, and ControlNational Heart, Lung, and Blood InstituteGail G. Weinmann, M.D.Program DirectorDivision of Lung DiseasesNational Heart, Lung, and Blood Institute
Executive SummaryBackgroundIn September 2004, the National Heart, Lung,and Blood Institute (NHLBI) convened a 2-daymeeting to develop a national education strategyfor chronic obstructive pulmonary disease(COPD), a progressive obstruction of the airpassages of the lung that is not fully reversibleby treatment. (See appendix A for the meeting’sagenda.) COPD is the fourth leading cause ofdeath in the United States and is growing inprevalence around the globe. From 1965 to1998, the death rate from COPD grew 163percent while death rates from all other majordiseases fell. Approximately 15 million peoplein the United States have COPD, leading to 15 billion in annual direct medical costs.Symptoms include shortness of breath,persistent coughing, and excess mucousproduction. Patients are generally diagnosedin their 40s or later, sometimes after yearsof symptoms.Smoking causes about 85 percent of COPDcases, but other environmental factors—such asfumes, gases, and dust—also play a role. Someoccupations and certain industries, especiallymining and manufacturing, raise a person’s riskof COPD, as does the genetic predispositionof alpha-1 antitrypsin deficiency.Some theories suggest that bacterial and viralinfections help trigger COPD. It is likely thatgenetic factors also shape the risk for the disease,but researchers are just beginning to identify thegenes involved.Overview of the ProblemDespite the prevalence of COPD, the publicand those at greatest risk for the disease arelargely unaware of it. Most people do not realizethat COPD is a serious consequence ofcigarette, cigar, and pipe smoking that canprofoundly affect quality of life and lead topremature death.Diagnosis of COPD can be made byspirometry, a simple test of lung function.Spirometry is underused, however, especiallyamong primary care physicians. Treatmentsthat relieve symptoms and improve qualityof life, such as short- and long-actingbronchodilators and pulmonary rehabilitation,are available but are also underused.Unfortunately, no current treatments reversethe progressive loss of lung function in COPD,although smoking cessation has been provento slow its course.The myths and stigma that surround COPDhinder its diagnosis and treatment. Manyphysicians do not recognize the symptomsof COPD until late in its course, and thenregard the condition as untreatable, progressive,and ultimately terminal. Attitudes of “blameand shame” too often accompany a diagnosisof COPD. Physicians and caregivers may blamepatients for bringing the disease on themselves.The shame felt by patients fosters denial anddelays seeking care. These negative attitudescontribute to underdiagnosis, undertreatment,and a general lack of awareness about COPD.It is true that no known treatment reversesor “cures” COPD, but now that it is knownthat smoking cessation slows progression andthat treatments can relieve symptoms, preventexacerbations, improve functional capacity,and enhance quality of life, the time is rightto increase awareness about COPD and itsrisk factors, treatment, and prevention.Goals and RecommendationsThe primary recommendation that emergedfrom the workshop deliberations was thatNHLBI develop and implement an awarenesscampaign on COPD that simultaneouslyreaches those with the disease, those at risk,and health care providers. Additional workshopconclusions about the campaign includedrecommendations to:Executive Summaryix
Communicate to patients, those at risk, andhealthcare providers that COPD is a chronic,treatable disease.x Encourage the use of spirometry testing inthe primary care setting. Aim to diffuse negative attitudes aboutCOPD held by all audiences. Encourage those diagnosed with COPDto take action to slow the progressionof the disease. Raise awareness about COPD signs andsymptoms among those at risk as wellas patients. Encourage patients with severe COPDto take an active role in managing theirtreatment.Chronic Obstructive Pulmonary Disease
IntroductionThe National Heart, Lung, and Blood Institute(NHLBI) convened a 2-day Education StrategyDevelopment Workshop on ChronicObstructive Pulmonary Disease (COPD)on September 22-23, 2004, in Alexandria,Virginia. The purpose of the workshop wasto bring together relevant stakeholders—COPDpatients and caregivers, members of advocacyorganizations, clinicians, representatives ofNational health organizations and coalitions,and Federal Government representatives—toidentify what is currently being done to addressCOPD education issues and what gaps ineducation exist.Workshop participants were tasked with makingrecommendations to NHLBI for education andawareness activities based upon presentationsmade at the workshop as well as their ownknowledge and experiences.Approximately 60 stakeholders attended theworkshop and heard presentations by expertsin COPD on the current environment relativeto COPD management and treatment; earlydetection and diagnosis; the role of patientadvocacy organizations; and risk factors fordeveloping COPD. In addition, a panel ofpatients and caregivers shared their personalexperiences being diagnosed and treated forCOPD. A second panel, comprised of healthcare providers, shared their experiences andperspectives on diagnosing and treating COPD.In small group break-out sessions, workshopparticipants defined the needs of targetaudiences and made recommendations forawareness and education activities for thoseaudiences. Target audiences addressed in thesmall groups were health care professionals;at-risk and early stage patients; and patientswith established and advanced disease.The primary recommendation made to NHLBIat the conclusion of the workshop was todevelop and implement a public awarenesscampaign on COPD that targets patients andthose at risk as well as health care providers.Introduction1
PresentationsWednesday, September 22, 2004Presentations: Wednesday, September 22, 20043
PresentationsWednesday, September 22, 2004How Strategy Development WorkshopsHave Shaped NHLBI’s NationalEducation Programs?GREGORY J. MOROSCO, PH.D., M.P.H.During the past 30 years, NHLBI has educatedprofessionals, patients, and the public onpertinent public health issues through highprofile programs, including the National HighBlood Pressure Education Program, theNational Cholesterol Education Program,the National Asthma Education and PreventionProgram, the NHLBI Obesity EducationInitiative, and the NHLBI Women’s HeartHealth Education Initiative.All of these programs share three characteristics: Messages are rooted in the best science. Education and communication efforts aretailored to appropriate audiences. Local and national partnerships help toexpedite the delivery of the latest sciencebased information to improve public health.The goal of this meeting is to develop ablueprint for health education andcommunication about COPD for patients,health professionals, and the public.In 2001, NHLBI held a similar meeting forheart health and women to address the lackof awareness of heart disease as the leadingkiller of women. That 2-day meeting spurreda hugely successful effort—The Heart Truthcampaign symbolized by the red dress—the newnational symbol for women and heart disease.The impact of the campaign is quicklybecoming apparent. In 1997, the AmericanHeart Association found that only 34 percentof women realized that heart disease was the#1 killer among women. In 2003, that figurejumped to 46 percent.Why a Strategy Development Workshopon COPD Is Needed?JAMES P. KILEY, PH.D.Ultimately, our goal is to improve the healthof the Nation. Because COPD is consistentlyunderestimated as a public health problem, thetime has arrived to raise awareness of the diseaseand its treatments. One critical path to that goalis educating the public, patients, healthprofessionals, and policymakers.This burden is increasing. See Box 1. From1965 to 1998, deaths caused by COPD haverisen 163 percent. Turning this trend aroundwill take a concerted effort, and we’re at a criticalpoint for doing so. NHLBI has a COPD clinicalresearch network that is testing new treatments,and we need to ensure that the widest possiblecross-section of patients benefits from theseadvances. To do that, we need an infrastructurefor education that leverages partnerships and fillsBox 1: The burden of COPD is staggering and can be summarized by the “15s”: 15 million patients in the United States 1.5 million emergency department visits annually 150 million days of lost work annually 15 billion annually in direct medical expenses4Chronic Obstructive Pulmonary Disease
the gaps in awareness. NHLBI can playa role, but we need guidance and input fromeveryone—researchers, policymakers, physicians,patients, and family members.COPD Awareness and Education:What Is Needed?HOMER A. BOUSHEY, M.D.Any successful COPD education program mustbuild on our knowledge of the disease. Here isa brief outline of our understanding.What is COPD?COPD is characterized by airflow limitationdue to airspace and airway disease that is onlypartially reversible by treatment. Physicians andthe public use several labels to refer to COPD,including chronic bronchitis, chronicobstructive bronchitis, emphysema, and“smoker’s lung.”Any education and awareness program willhave to confront the issue of multiple names.Multiple labels confuse patients and complicateepidemiological research, making it difficult forresearchers to pinpoint exactly how manypeople have the disease.Although cigarette smokers are at high risk forCOPD, few recognize it as a threat. The vastmajority do not realize that they are nearly aslikely to die from COPD as from lung cancer.What is the burden of COPD?COPD now ranks as the fourth leading causeof death in the United States, accounting for114,000 deaths annually. This rate is rising inboth males and females but is rising fasteramong women, as they recently passed men intotal deaths from COPD. Globally, during thenext 30 years, COPD will rise to become thethird leading cause of death. However, there arestill gaps in our epidemiological knowledge ofCOPD, especially in estimating the prevalenceof undiagnosed disease.What causes COPD?The disease is attributed to an abnormalinflammatory response to repeated inhalationof harmful particles and gases, especially thosein cigarette smoke. The size, density, andcomposition of particles and gases determinehow harmful they are to the airways.This broad understanding, though, is limitedby enormous gaps in knowledge. Viral andbacterial infections might play a role, butevidence is limited. We have identified alpha-1antitrypsin deficiency as a genetic risk factor forCOPD but do not know the role of other genesin determining a person’s susceptibility.How can COPD be detected?The disease is easy to detect, but only ifphysicians have a high index of suspicion.One problem is that many physicians simplydo not think of COPD or look for it. For thatreason, the prevalence is probably grosslyunderestimated. Patients often fail to bringbreathing problems to the attention of theirphysicians. Instead, they tend, oftenunconsciously, to modify their behavior to avoidshortness of breath.Spirometry is a safe, accurate, and painless test.Unlike the devices used in the past, modernequipment is inexpensive, compact, and easy touse. Many physicians maintain outdated viewsof spirometry. They believe that the equipmentis unwieldy, that the results are difficult tointerpret, and that treatment decisions can bemade just as easily on the basis of symptomsand a physical exam. All of these views aredemonstrably false. Generally, physicians willonly use spirometry if they believe a diagnosiswill lead to a benefit. In patients with moderateor severe COPD, there is a proven benefit todiagnosis: It leads to treatment, and despitecommon misperceptions, effective treatmentsare available.Presentations: Wednesday, September 22, 20045
Figure 1: Another Way of Defining tyHow does COPD progress?Gaps in our knowledge prevent a concreteanswer, but we know that continued exposureto particles and gases that cause COPDaccelerates its course. We also know that thecourse is punctuated by periodic exacerbations,most often caused by viral or bacterial infectionsof the bronchial airways. These account forgreat morbidity and cost, and occur morefrequently in patients with severe COPD.Recovery from exacerbations of COPD may beprolonged, but their impact on the overall rateof loss of pulmonary function is unknown.Progression of COPD can be defined as adescending spiral. See Figure 1. The diseaseleads to dyspnea, which leads to inactivity,6Chronic Obstructive Pulmonary DiseaseDyspneaDeconditioningwhich causes deconditioning, which causesmore dyspnea, and so on.Can it be treated?Although treatment cannot fully reverseairflow obstruction, it can improve qualityof life. Bronchodilators temporarily improveairflow obstruction and alleviate immediatesymptoms; some drugs decrease the frequencyof exacerbations; smoking cessation slowsprogression of the disease; and oxygensupplementation can prolong life. The onlytreatment effective against progression of thedisease is smoking cessation. The onlytreatment proven to prolong life is oxygensupplementation in patients with oxygeninsufficiency.
Box 2: COPD Goals of Healthy People 2010GoalHP 2010 TargetCurrent RateReduce COPDamong adults.1.5%2.2%Reduce death rate fromCOPD among all adults.60 per 100,000119.4 per 100,000Pulmonary rehabilitation is another treatmentoption. While it does not significantly improvepulmonary function, it reduces symptoms,alleviates anxiety and depression, reduceshospitalization rates, improves exercise performance, and enhances overall quality of life.Unfortunately, all of these treatments areunderused. The public, patients, and physiciansoften believe that treatments are not useful.This is untrue. Although the treatments wehave are not perfect, they help many patients.doing much better in caring for those who haveit. The 2002 Confronting COPD Survey1interviewed 3,265 people with COPD andfound that: 60 percent reported limitations in physicalactivities. 45 percent reported limitations in socialactivities. 36 percent of those under age 65 were unableto work.How are we doing?Healthy People 2010 set two goals for COPD:to reduce the proportion of adults older than45 whose activities are limited by chronic lungproblems and to reduce deaths from COPDamong all adults (See Box 2.). These goals willbe hard to achieve since COPD develops andprogresses insidiously, causing symptoms onlywhen the loss of pulmonary function becomessevere enough to interfere with usual activities.There is thus a large reservoir of “preclinical”COPD patients who will add to the numbersof those diagnosed with COPD as the “babyboomer” population ages.While we are not doing well in detectingpatients with “preclinical” COPD, we are not 13 percent had been hospitalized in thepast year.The survey also found that patients consistentlyunderestimated the severity of their disease. Forinstance, of those whose symptoms were so severethey had trouble leaving the house, 36 percentsaid they had “mild or moderate” disease.Why are we doing so poorly?One theory holds that patients, providers, andsociety are coconspirators in denial about theprevalence and severity of COPD. Our builtenvironment2 makes it easy to avoid symptoms.Many patients feel shame, blaming themselvesfor bringing on the disease. Time pressures onRennard S, Decramer M, Calverley PMA, et al. Impact of COPD in North America and Europe in 2000: Subjects’ perspectiveof confronting COPD international survey. Eur Respir J. 2002;20:799–805.2“Built environment” encompasses all of the buildings, spaces, and products created or modified by people.Also see tations: Wednesday, September 22, 20047
physicians and “therapeutic nihilism”—thebelief that treatments do not work—lead tounderdiagnosis and undertreatment.What can we do about it?Facts are the best remedy for denial: COPDis common and is growing in prevalence; theburden is great and becoming greater; COPDis easy to diagnose; and treatments, althoughnot perfect, are effective, especially for patientswith moderate-to-severe disease.Lessening the burden of COPD will requirea broad, coordinated education strategy.Government commitment to and communityinvolvement in a focused plan can push ustoward our goals. For maximum impact,legislative, educational, research, and treatmentinitiatives must fit together logically.What Do Patients, Families, and At-RiskIndividuals Need To Know?JOHN W. WALSHMany patients feel we are “on our own” withthis disease. We need to know what a diagnosisof COPD means and what challenges lay ahead.Many of us are unsure where to turn for help.In talking with other patients, I’ve found thatmany are despondent and feel helpless.Two surveys, Confronting COPD3 and theCOPD Resource Network Needs AssessmentSurvey4, show that patients do not feel wellinformed about treatment options. Manynever or rarely see lung specialists. Awarenessof pulmonary rehabilitation and its benefitsis low, and dissatisfaction with treatment ishigh.We need direction, advice, and education.We know that patients connected with advocacygroups fare better and feel more informed. “Themore aware, the better the care” could be our8slogan. Unfortunately, 83 percent of patientsare unaware that patient groups are available.Although the Internet harbors much usefulinformation and support for COPD,approximately 80 percent of patients reportlittle or no access to the Internet. That meanswe need to reach patients through otherchannels. Patient education improves outcomesand reduces costs. The desire and need for moreand better information is extremely high, butwe’ve got a long way to go.Moving Forward Through Translationand CommunicationLAWRENCE FRIEDMAN, M.D.Dr. Friedman said that we need to pay moreattention to translation and communication.We’ve done that with high blood pressure andother health risks. Clearly, the whole issue oftranslation—getting what we know out into thecommunity—is something we have not paidenough attention to in COPD.The NHLBI invites your input and guidance.How can we proceed? What are the appropriateways? What information do we need to learnhow to communicate better?The Current Environment: Managementand TreatmentFERNANDO J. MARTINEZ, M.D., M.S.During the past 5 years, there has been anexplosion of professional guidelines for themanagement and treatment of COPD.However, awareness among physicians is low:Approximately 45 percent of primary carephysicians and 6 percent of pulmonologistsdo not know that COPD guidelines exist.See Figure 2.The various guidelines are similar to somedegree: 98 percent present a definition of3Rennard S, Decramer M, Calverley PMA, et al. Impact of COPD in North America and Europe in 2000: Subjects’ perspectiveof confronting COPD international survey. Eur Respir J. 2002;20:799–805.4Barr RG, Celli BR, Martinez FJ, et al. Physician and patient perceptions in COPD: The COPD Resource Network NeedsAssessment Survey. Am J Med. 2005;118:1415.e9–1415.e17.Chronic Obstructive Pulmonary Disease
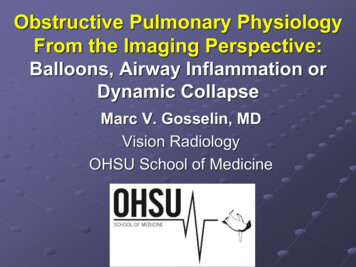
Figure 2: Awareness of Professional Guidelines for COPDPrimary care doctorsPulmonologists(N 528)(N 523)No answer , 1%No answer , 1%No, 6%No, 45%Yes , 54%Yes , 94%Are you aware of any professional guidelifor the diagnosis and management4 of COPD?COPD; 98 percent recommend lungrehabilitation; and 83 percent recommendspirometry for diagnosis.However, physician adherence is not uniform.When diagnosing COPD, only 32 percentof primary care physicians and 79 percent ofpulmonologists state they use spirometry fordiagnosis all the time. That figure should be100
National Heart, Lung, and Blood Institute Education Strategy Development Workshop U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES . Washington, DC Lawrence Grouse, M.D., Ph.D. Executive Director U.S. COPD Coalition . bronchodilators and pulmonary rehabilitation, are available but are also underused. Unfortunately, no current treatments reverse .