Transcription
National Institute of Neurological Disordersand StrokeNational Institutes of HealthHope Through ResearchTraumatic Brain Injury
NINDS health-related material is provided forinformation purposes only and does not necessarilyrepresent endorsement by or an official position of theNational Institute of Neurological Disorders and Strokeor any other Federal agency. Advice on the treatmentor care of an individual patient should be obtainedthrough consultation with a physician who hasexamined that patient or is familiar with that patient’smedical history.All NINDS-prepared information is in the public domainand may be freely copied. Credit to the NINDS or theNIH is appreciated.
Table of ContentsWhat is a TBI? . 1What are the signs and symptoms? . 2TBI in children . 3Effects on consciousness . 4How does TBI affect the brain? . 5What are the leading causes of TBI? . 9How is TBI diagnosed? . 11How is TBI treated? . 13Treating mild to moderate TBI . 14Treating severe TBI . 15Rehabilitation . 16Other factors that influence recovery . 17Genes. 17Age . 18Can a TBI be prevented? . 18What research is NINDS funding? . 20Clinical trials . 22Interagency and International ResearchCollaboration . 23How can I support TBI research? . 24Where can I get more information? . 25i
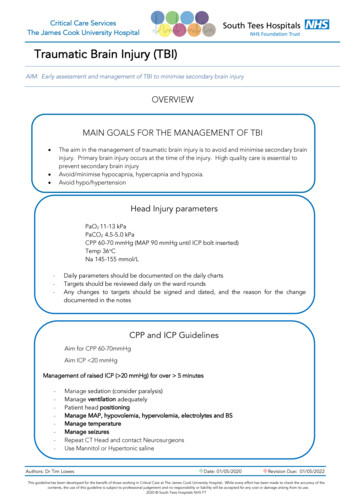
What is a TBI?A traumatic brain injury (TBI) can be caused by aforceful bump, blow, or jolt to the head or body, or froman object that pierces the skull and enters the brain.Not all blows or jolts to the head result in a TBI.Some types of TBI can cause temporary or shortterm problems with normal brain function, includingproblems with how the person thinks, understands,moves, communicates, and acts. More serious TBIcan lead to severe and permanent disability, andeven death.Some injuries are considered primary, meaning thedamage is immediate. Other outcomes of TBI can besecondary, meaning they can occur gradually over thecourse of hours, days, or appear weeks later. Thesesecondary brain injuries are the result of reactiveprocesses that occur after the initial head trauma.There are two broad types of head injuries:penetrating and non-penetrating. Penetrating TBI (also known as open TBI) happenswhen an object pierces the skull (for example, abullet, shrapnel, bone fragment, or by a weaponsuch as hammer or knife) and enters the braintissue. Penetrating TBI typically damages only partof the brain. Non-penetrating TBI (also known as closed headinjury or blunt TBI) is caused by an external forcestrong enough to move the brain within the skull.Causes include falls, motor vehicle crashes, sportsinjuries, blast injury, or being struck by an object.Some accidents such as explosions, natural disasters,or other extreme events can cause both penetratingand non- penetrating TBI in the same person.1
What are the signs and symptoms?Seek immediate medical attention if you experienceany of the following physical, cognitive/behavioral,or sensory symptoms, especially within the first 24hours after a TBI:Physical headache convulsions or seizures blurred or double vision unequal eye pupil size or dilation clear fluids draining from the nose or ears nausea and vomiting new neurologic deficit, i.e., slurred speech;weakness of arms, legs, or face; loss of balance2Cognitive/behavioral loss of or change in consciousness anywherefrom a few seconds to a few hours decreased level of consciousness, i.e., hardto awaken mild to profound confusion or disorientation problems remembering, concentrating, ormaking decisions changes in sleep patterns (e.g., sleeping more,difficulty falling or staying asleep); inability towaken from sleep frustration, irritabilityPerception/sensation light-headedness, dizziness, vertigo, or loss ofbalance or coordination
blurred vision hearing problems, such as ringing in the ears bad taste in the mouth sensitivity to light or sound mood changes or swings, agitation, combativeness,or other unusual behavior feeling anxious or depressed fatigue or drowsiness; a lack of energy ormotivationHeadache, dizziness, confusion, and fatigue tend tostart immediately after an injury, but resolve over time.Emotional symptoms such as frustration and irritabilitytend to develop during recovery.TBI in childrenChildren might be unable to let others know that theyfeel different following a blow to the head. A child witha TBI may display the following signs or symptoms: changes in eating or nursing habits persistent crying, irritability, or crankiness;inability to be consoled changes in ability to pay attention lack of interest in a favorite toy or activity changes in sleep patterns seizures sadness or depression loss of a skill, such as toilet training loss of balance or unsteady walking vomiting3
TBI symptoms including headache, dizziness, confusion, and fatigue tend tostart immediately after an injury, but resolve over time.Effects on consciousness4A TBI can cause problems with consciousness,awareness, alertness, and responsiveness. Generally,there are four abnormal states that can result from asevere TBI: Minimally conscious state — People with severelyaltered consciousness who still display someevidence of self-awareness or awareness ofone’s environment (such as following simplecommands, yes/no responses). Vegetative state — A result of widespreaddamage to the brain, people in a vegetativestate are unconscious and unaware of theirsurroundings. However, they can have periodsof unresponsive alertness and may groan,move, or show reflex responses. If this statelasts longer than a few weeks, it is referredto as a persistent vegetative state. Coma — A person in a coma is unconscious,unaware, and unable to respond to external stimuli
such as pain or light. Coma generally lasts a fewdays or weeks after which the person may regainconsciousness, die, or move into a vegetative state. Brain death — The lack of measurable brainfunction and activity after an extended period oftime is called brain death and may be confirmed bystudies that show no blood flow to the brain.How does TBI affect the brain?TBI-related damage can be confined to one areaof the brain, known as a focal injury, or it can occurover a more widespread area, known as a diffuseinjury. The type of injury also affects how the brainis damaged.Primary effects on the brain include various typesof bleeding and tearing forces that injure nerve fibersand cause inflammation, metabolic changes, andbrain swelling. Diffuse axonal injury (DAI) — one of the mostcommon types of brain injuries — refers towidespread damage to the brain’s white matter.White matter is composed of bundles of axons(the projections of nerve cells that carry electricalimpulses and connect various areas of the brain toone another). DAI usually results from rotationalforces (twisting) or sudden forceful stoppingthat stretches or tears these axon bundles. Thisdamage commonly occurs in auto accidents,falls, or sports injuries. DAI can disrupt and breakdown communication among nerve cells (neurons)in the brain. It also leads to the release of brainchemicals that can cause further damage. Braindamage may be temporary or permanent andrecovery can be prolonged.5
Concussion — a type of mild TBI that may beconsidered a temporary injury to the brain but couldtake minutes to several months to heal. Concussioncan be caused by a number of things includinga bump, blow, or jolt to the head, sports injuryor fall, motor vehicle accident, weapons blast, ora rapid acceleration or deceleration of the brainwithin the skull (such as the person having beenviolently shaken). The individual either suddenlyloses consciousness or has sudden altered state ofconsciousness or awareness. A second concussionclosely following the first one causes furtherdamage to the brain — the so-called “second hit”phenomenon — and can lead to permanent damageor even death in some instances. Post-concussionsyndrome involves symptoms that last for weeks orlonger following concussion.6 Hematomas — bleeding in and around the braincaused by a rupture to a blood vessel. Differenttypes of hematomas form depending on wherethe blood collects relative to the meninges, theprotective membranes surrounding the brain,which consist of three layers: dura mater(outermost), arachnoid mater (middle), andpia mater (innermost).– Epidural hematomas involve bleeding into thearea between the skull and the dura mater.These can occur within minutes to hours afterdamage to a brain vessel under the skull andare particularly dangerous.– Subdural hematomas involve bleeding betweenthe dura and the arachnoid mater, and, likeepidural hematomas, exert pressure on theoutside of the brain. They are very common inthe elderly after a fall.
– Subarachnoid hemorrhage is bleeding betweenthe arachnoid mater and the pia mater.– Bleeding into the brain itself is called anintracerebral hematoma and damages thesurrounding tissue. Contusions — a bruising or swelling of the brainthat occurs when very small blood vessels bleedinto brain tissue. Contusions can occur directlyunder the impact site (i.e., a coup injury) or, moreoften, on the complete opposite side of the brainfrom the impact (i.e., a contrecoup injury). They canappear after a delay of hours to a day. Coup andcontrecoup lesions generally occur when the headabruptly decelerates, which causes the brain tobounce back and forth within the skull (such as in ahigh-speed car crash or in shaken baby syndrome). Skull fractures — breaks or cracks in one or moreof the bones that form the skull. They are a resultof blunt force trauma and can cause damage to themembranes, blood vessels, and brain under thefracture. One main benefit of helmets is to preventskull fracture. Chronic traumatic encephalopathy (CTE) is aprogressive neurological disorder associated withsymptoms that mayinclude problems withthinking, understanding,and communicating;motor disorders(affecting movement);problems with impulsecontrol and depression;confusion; andirritability. CTE occurs inthose with extraordinaryexposure to multipleSkull fractures result from blunt forcetrauma and can cause damage tounderlying areas of the skull.7
blows to the head and as a delayed consequenceafter many years. Studies of retired boxers haveshown that repeated blows to the head can causeissues including memory problems, tremors, andlack of coordination and dementia. Recent studieshave demonstrated rare cases of CTE in other sportswith repetitive mild head impacts (e.g., soccer,wrestling, football, and rugby). A single, severe TBIalso may lead to a disorder called post-traumaticdementia (PTD), which may be progressive andshare some features with CTE. Studies assessingpatterns among large populations of people withTBI indicate that moderate or severe TBI in early ormid-life may be associated with increased risk ofdementia later in life.Secondary damage can include:8 Hemorrhagic progression of a contusion (HPC)injuries occur when an initial contusion from theprimary injury continues to bleed in and aroundthe brain and expand over time. This creates a newor larger lesion — an area of tissue that has beendamaged through injury or disease. This increasedexposure to blood, which is toxic to brain cells,leads to swelling and further brain cell loss. A breakdown in the blood-brain barrier — anetwork of cells that controls the movement of cellsand molecules between the blood and fluid thatsurrounds the brain’s nerve cells. Once the bloodbrain barrier is disrupted, blood, plasma proteins,and other foreign substances leak into the spacebetween neurons in the brain and trigger a chainreaction that causes brain swelling. It also causesmultiple biological systems to go into overdrive,including inflammatory responses which can beharmful to the body if they continue for an extendedperiod of time. It also permits the release of
neurotransmitters — chemicals used by brain cellsto communicate — which can damage or kill nervecells when depleted or over-expressed. Increased intracranial pressure, usually caused bybrain swelling inside the confined area of the skullas a result of the injury. This pressure can damagebrain tissue and can prevent blood flow to the brainand deprive it of the oxygen it needs to function.Other secondary damage can be caused by infectionsto the brain, low blood pressure or oxygen flow as aresult of the injury, hydrocephalus (a buildup of fluid inthe brain that can increase pressure on brain tissue),and seizures.What are the leading causes of TBI?Falls. According to data from the Centers for DiseaseControl and Prevention (CDC), falls are the mostcommon cause of TBIs and occur most frequentlyamong the youngest and oldest age groups. From 2006to 2010 alone, falls caused more than half (55 percent)of TBIs among children aged 14 and younger. AmongAmericans age 65 and older, falls accounted for morethan two-thirds (81 percent) of all reported TBIs.Blunt trauma accidents. Accidents that involve beingstruck by or against an object, particularly sportsrelated injuries, are a major cause of TBI. Anywherefrom 1.6 million to 3.8 million sports- and recreationrelated TBIs are estimated to occur in the UnitedStates annually.Vehicle-related injuries. Pedestrian-involved accidents,as well as accidents involving motor vehicles andbicycles, are the third most common cause of TBI.In young adults aged 15 to 24 years, motor vehicleaccidents are the most likely cause of TBI.9
Assaults/violence. Assaults include abuse relatedTBIs, such as head injuries that result from domesticviolence or shaken baby syndrome, and gunshotwounds to the head. TBI-related deaths in children age4 and younger are most likely the result of assault.Explosions/blasts. TBIs caused by blast trauma fromroadside bombs became a common injury to servicemembers in recent military conflicts. The majority ofthese TBIs were classified as mild head injuries.Adults age 65 and older are at greatest risk for beinghospitalized and dying from a TBI, most likely from afall. In every age group, serious TBI rates are higherfor men than for women. Men are more likely to behospitalized and are nearly three times more likely todie from a TBI than women.10Additional information about TBI and its causes canbe found on the U.S. Centers for Disease Controland Prevention TBI website: elated injuries are the third most common cause of TBI.
How is TBI diagnosed?All TBIs require immediate assessment by aprofessional who has experience evaluating headinjuries. A neurological exam will judge motorand sensory skills and test hearing and speech,coordination and balance, mental status, and changesin mood or behavior, among other abilities. Screeningtools for coaches and athletic trainers can identify themost concerning concussions for medical evaluation.Initial assessments may rely on standardizedinstruments such as the Acute Concussion Evaluation(ACE) form from the Centers for Disease Control andPrevention or the Sport Concussion Assessment Tool 2,which provide a systematic way to assess a person whohas suffered a mild TBI. Reviewers collect informationabout the characteristics of the injury, the presenceof amnesia (loss of memory) and/or seizures, as wellas the presence of physical, cognitive, emotional, andsleep-related symptoms. The ACE is also used to tracksymptom recovery over time. It also takes into accountrisk factors (including concussion, headache, andpsychiatric history) that can impact how long it takes torecover from a TBI.Diagnostic imaging. When necessary, medicalproviders will use brain scans to evaluate the extent ofthe primary brain injuries and determine if surgery willbe needed to help repair any damage to the brain. Theneed for imaging is based on a physical examination bya doctor and a person’s symptoms. Computed tomography (CT) is the most commonlyused imaging technology to assess people withsuspected moderate to severe TBI. CT uses a seriesof X-rays (concentrated bursts of ionizing radiation)to create a two-dimensional image of organs,bones, and tissues and can show a skull fracture orany brain bruising, bleeding, or swelling.11
Magnetic resonance imaging (MRI) uses computergenerated radio waves and a powerful magneticfield to produce detailed images of body tissue.It may be used after the initial assessment andtreatment as it is a more sensitive test and picks upsubtle changes in the brain that the CT scan mighthave missed.12Much of what is believed to occur to the brainfollowing mild TBI happens at the cellular level.Significant advances have been made in the lastdecade to image milder TBI damage. For example,diffusion tensor imaging can image white mattertracts, more sensitive tests like fluid-attenuatedinversion recovery can detect small areas ofdamage, and susceptibility-weighted imagingvery sensitively identifies bleeding. Despitethese improvements, currently availableimaging technologies, blood tests, and othermeasures remain inadequate for detectingthese changes in a way that can help diagnosemild concussive injuries.The most common imaging technology used to evaluate people with suspected TBI iscomputed tomography or CT.
Neuropsychological tests to gauge brain functioningare often used in conjunction with imaging in peoplewho have suffered mild TBI. Such tests involveperforming specific cognitive tasks that help assessmemory, concentration, information processing,executive functioning, reaction time, and problemsolving. The Glasgow Coma Scale is the most widelyused tool for assessing the level of consciousnessafter TBI. The standardized 15-point test measures aperson’s ability to open his or her eyes and respond tospoken questions or physical prompts for movement. Atotal score of 3-8 indicates a severe head injury; 9-12indicates moderate injury; and 13-15 is classified asmild injury. (For more information about the scale, seehttp://glasgowcomascale.org/).Many athletic organizations recommend establishinga baseline picture of an athlete’s brain function at thebeginning of each season, ideally before any headinjuries have occurred. Baseline testing should beginas soon as a child begins a competitive sport. Brainfunction tests yield information about an individual’smemory, attention, and ability to concentrate andsolve problems. Brain function tests can be repeatedat regular intervals (every 1 to 2 years) and also aftera suspected concussion. The results may help healthcare providers identify any effects from an injuryand allow them to make more informed decisionsabout whether a person is ready to return to theirnormal activities.How is TBI treated?Many factors, including the size, severity, and locationof the brain injury, influence how a TBI is treatedand how quickly a person might recover. People whoreceive immediate medical attention at a certifiedtrauma center tend to have the best health outcomes.13
Treating mild to moderate TBISome people with mild TBI such as concussion may notrequire treatment other than rest and over-the-counterpain relievers. Treatment should focus on symptomrelief and “brain rest.” Monitoring by a healthcarepractitioner is important to note any worsening ofsymptoms or new ones.Children and teens who have a sports-relatedconcussion should stop playing immediately andreturn to play only after being approved by aconcussion injury specialist.Preventing future concussions is critical. While mostpeople recover fully from a first concussion within afew weeks, the rate of recovery from a second or thirdconcussion is generally slower.14Even after symptoms resolve entirely, people shouldreturn to their daily activities gradually once they aregiven permission by a doctor. There is no clear timelinefor a safe return to normal activities although there areguidelines such as those from the American Academyof Neurology and the American Medical Society forSports Medicine to help determine when athletes canreturn to practice or competition. Further research isneeded to better understand the effects of mild TBI onthe brain and to determine when it is safe to resumenormal activities.People with a mild TBI should: Make an appointment for a follow-up visit withtheir healthcare provider to confirm the progressof their recovery. Inquire about new or persistent symptoms andhow to treat them. Pay attention to any new signs or symptoms evenif they seem unrelated to the injury (for example,mood swings, unusual feelings of irritability).
These symptoms may be related even if theyoccurred several weeks after the injury.Medications to treat some of the symptoms of TBImay include: Over-the-counter or prescribed pain medicines Anticonvulsant drugs to treat seizures Anticoagulants to prevent blood clots Diuretics to help reduce fluid buildup and reducepressure in the brain Stimulants to increase alertness Antidepressants and anti-anxiety medicationsto treat depression and feelings of fear andnervousness.Treating severe TBIImmediate treatment for someone who has suffereda severe TBI focuses on preventing death; stabilizingthe person’s spinal cord, heart, lung, and other vitalorgan functions; ensuring proper oxygen delivery andbreathing; controlling blood pressure; and preventingfurther brain damage. Emergency care staff alsowill monitor the flow of blood to the brain, braintemperature, pressure inside the skull, and thebrain’s oxygen supply.Surgery may be needed to for emergency medicalcare and to treat secondary damage, including: relieving pressure inside the skull (inserting aspecial catheter through a hole drilled into theskull to drain fluids and relieve pressure) removing debris or dead brain tissue (especiallyfor penetrating TBI) removing hematomas repairing skull fractures.15
In-hospital strategies for managing people with severe TBI focus on preventing infectionand blood clots (like the one shown above).16In-hospital strategies for managing people with severeTBI aim to prevent conditions including: Infection, particularly pneumonia deep vein thrombosis (blood clots that occurdeep within a vein; risk increases during longperiods of inactivity)People with TBIs may need nutritional supplementsto minimize the effects that vitamin, mineral, andother dietary deficiencies may cause over time.Some individuals may even require tube feedingto maintain the proper balance of nutrients.RehabilitationAfter the acute care period of in-hospital treatment,people with severe TBI are often transferred to arehabilitation center where a multidisciplinaryteam of health care providers help with recovery.
The rehabilitation team includes neurologists,nurses, psychologists, nutritionists, as well asphysical, occupational, vocational, speech, andrespiratory therapists.Therapy is aimed at improving the person’s abilityto handle activities of daily living and to addresscognitive, physical, occupational, and emotionaldifficulties. Treatment may be needed only short-termor throughout a person’s life. Some therapy isprovided through outpatient services.Cognitive rehabilitation therapy (CRT) is a strategyaimed at helping individuals regain their normalbrain function through an individualized trainingprogram. Using this strategy, people may alsolearn compensatory strategies for coping withpersistent deficiencies involving memory, problemsolving, and the thinking skills to get things done.CRT programs tend to be highly individualizedand their success varies. A 2011 Institute ofMedicine report concluded that cognitiverehabilitation interventions need to be developedand assessed more thoroughly.Other factors that influence recoveryGenesGenetics may play a role in how quickly andcompletely a person recovers from a TBI. For example,researchers have found that apolipoprotein E ε4(ApoE4) — a genetic variant associated with higherrisks for Alzheimer’s disease — is associated withworse health outcomes following a TBI. Much workremains to be done to understand how geneticfactors, as well as how specific types of headinjuries, affect recovery. This research may leadto new treatment strategies and improvedoutcomes for people with TBI.17
AgeStudies suggest that age and the number of headinjuries a person has suffered over his or her lifetimeare two critical factors that impact recovery. Forexample, TBI-related brain swelling in children canbe very different from the same condition in adults,even when the primary injuries are similar. Brainswelling in newborns, young infants, and teenagersoften occurs much more quickly than it does in olderindividuals. Evidence from very limited CTE studiessuggest that younger people (ages 20 to 40) tendto have behavioral and mood changes associatedwith CTE, while those who are older (ages 50 )have more cognitive difficulties.18Compared with younger adults with the same TBIseverity, older adults are likely to have less completerecovery. Older people also have more medical issuesand are often taking multiple medications that maycomplicate treatment (e.g., blood-thinning agentswhen there is a risk of bleeding into the head). Furtherresearch is needed to determine if and how treatmentstrategies may need to be adjusted based on aperson’s age.Researchers are continuing to look for additionalfactors that may help predict a person’s courseof recovery.Can a TBI be prevented?The best treatment for TBI is prevention. Unlike mostneurological disorders, head injuries can be prevented.According to the CDC, doing the following can helpprevent TBIs: Wear a seatbelt when you drive or ride in amotor vehicle.
Wearing a seatbelt when you drive or ride in a motor vehicle can help prevent TBI. Wear the correct helmet and make sure it fitsproperly when riding a bicycle, skateboarding,and playing sports like hockey and football. Install window guards and stair safety gates athome for young children. Never drive under the influence of drugs or alcohol. Improve lighting and remove rugs, clutter, andother trip hazards in the hallway. Use nonslip mats and install grab bars next to thetoilet and in the tub or shower for older adults. Install handrails on stairways. Improve balance and strength with a regularphysical activity program. Ensure children’s playgrounds are made ofshock-absorbing material, such as hardwoodmulch or sand.19
What research is NINDS funding?The mission of the National Institute on NeurologicalDisorders and Stroke (NINDS) is to seek fundamentalknowledge about the brain and nervous systemand use that knowledge to reduce the burden ofneurological disease. The NINDS is a component ofthe National Institutes of Health (NIH), the leadingsupporter of biomedical research in the world.NINDS supports research across the full range of TBIseverity, in animal models and people, from childrento adults. Projects focus on the mechanisms that resultin immediate and delayed damage to the brain, on theprocesses that underlie recovery, and developing betterdiagnostic tools and more effective treatments.Among NINDS research efforts:20 Transforming Research and Clinical Knowledgein TBI, or TRACK TBI, is an observational study ofadults and children with TBI across the spectrumof injury severity. It is creating a TBI databaseand provides tools and resources to establishmore precise methods to diagnose TBI, improveoutcome assessment, and compare theeffectiveness and costs of tests, treatments,and services. The data from this study will beavailable in the Federal Interagency TBI Researchdatabase (which enables comparisons acrossclinical trials and clinical studies. Scientists can now look in real time at how headinjury affects thousands of individual cells andgenes simultaneously in mice. Using a novelsequencing technique that can quickly analyzethe gene activity of a cell, scientists were able tolook individual brain cells in the hippocampus,a region of the brain involved in learning andmemory, after TBI or in uninjured control animals.Scientists can now pinpoint which genes to treatwith new therapies.
Researchers are conducting studies to betterunderstand the lasting effects of a single headinjury vs. repetitive injuries to the brain, howrepetitive TBI might lead to chronic traumaticencephalopathy, and how commonly thesechanges occur among adults. NINDS researchers arecurrently working to identify biomarkers (signs thatmay indicate risk of a disease and aid in diagnosis)for chronic traumatic encephalopathy in order todetect this and similar disorders in living peoplerather than through brain studies after death. Researchers are exploring ways to promote thebrain’s innate ability to adapt and repair itself,known as neuroplasticity. A developed mouse model of TBI is enablingresearchers to look at potential treatments forconcussion. Using the model, they found thatapplying glutathione (an antioxidant that isnormally found in our cells) directly on the skullsurface after brain injury reduced the amount ofbrain cell death.NINDS funds a wide range of TBI research in an effort to find better ways tosafely detect, treat, and ultimately prevent TBI.21
The NINDS-funded Translational Outcomes Projectin Neurotrauma (TOP-NT) consor
time is called brain death and may be confirmed by studies that show no blood flow to the brain. How does TBI affect the brain? TBI-related damage can be confined to one area of the brain, known as a . focal injury, or it can occur over a more widespread area, known as a . diffuse injury. The type of injury also affects how the brain is damaged.