Transcription
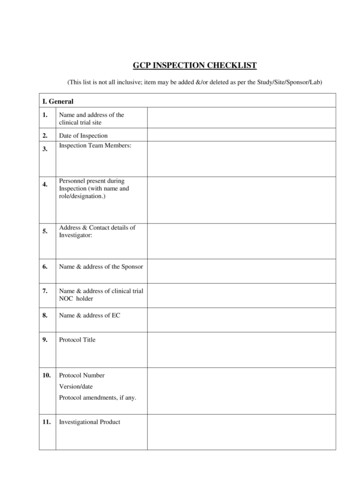
PHARMACY, MEDICINES & POISONS BOARDGCP INSPECTION CHECKLISTPage 1 of 10
ABBREVIATIONS / NAPIRASAEAdverse Drug ReactionAdvanced Life Support SystemsCase Report FormCertificate of AnalysisCardio-pulmonary resuscitationClinical Research OrganisationCurriculum VitaeData Safety Monitoring BoardGood Clinical PracticesGood Laboratory PracticesInternational Conference on HarmonisationIndependent Ethics CommitteeInstitutional Review BoardInvestigational Productnot checked or not applicablePrincipal InvestigatorRegulatory AuthoritySerious Adverse EventSOP Standard Operating ProcedureGCP INSPECTION CHECKLISTNames of InspectorsDate of InspectionName and address of the siteProtocol numberStage of study:Before trial commencementDuring clinical conductAfter completion of trialName of principal InvestigatorName of Sub (Co) InvestigatorStudy TitleRegulatory Authority Protocolapproval No.Page 2 of 10
Version & date:Amendment History approvalVersion & date:Ethics Protocol approvalVersion & date:Informed consent (ICON)Version approved & date:Amendment History approvalVersion & date:Screening date of 1stparticipantHow many participantsenrolled?How many participantswithdrew from the study?How many participantscompleted the study?Observations are classified into the categories “Critical”, “Major”, “Other (Minor)”. Therecommendations are listed at the end of the report. To be classified at a later stageA.FACILITY INSPECTION1Consulting Area1.1Is the consulting area where the PI/designated Physicianevaluates the participants during visits adequate in size?1.2Are there lock-up cupboards for confidential documents?1.3Is the trial specific equipment available in the consulting room?1.4If not, is the area where procedures are performed adequate andeasily accessible?1.5Does the PI manage and maintain the trial visits? To add to inspectionYESNONAtraining that this could be not applicable in the case of field sites2Procedure Room2.1Is all equipment e.g. Baumanometer, scale, lung functionmachine (asthma, COPD) as per protocol calibrated andvalidated?2.2Are SOPs on how to use equipment available?2.3Is the blood sampling area kept according to infection controlPage 3 of 10
A.2.4FACILITY INSPECTIONprocedures?YESNONAWaste handling according to applicable guidelines, e.g. from theRA or site or government?Page 4 of 10
A.2.5FACILITY INSPECTIONYESNONAIs the emergency trolley available in the procedure area? As per therequirements for vaccines and medical devices3 Is the trolley locked and are the keys available andcontrolled? Is the emergency trolley frequently checkeddocumentation as proof available? Are expiry dates clearly checked and controlled? Oxygen and accessories available, checked and signed? Are PI and sub-investigators ALSS trained? Are clinical staff CPR trained?andPharmacy (Investigational Product storage area)3.1Is the pharmacy access controlled, temperature and humiditycontrolled?3.2Are vaccines stored as per required temperature and humidity?3.3Is the preparation of investigational product management doneaccording to the approved protocol by suitable qualified staff?3.4In case of vaccines, are a spillage SOP available and the studyteam trained to handle such an incidence?3.5Are electronic or hand-written temperature logs available?3.6Is an SOP on how to handle electricity or temperature failure inthe pharmacy available?3.7Are the different studies Investigational Products in separatelock-up cupboards and clearly identified’?3.8Are vaccines transported and handled as per cold chainrequirements?4Archive4.1Is there an agreement between Sponsor and Trial Site/CRO onthe archiving of documentation?4.2Is this clause documented in the protocol or contract55.1Clinical LaboratoryIs the clinical laboratory at the same site?5.2If not, are procedures in handling biological samples clearlydocumented?(If clinical laboratory is nearby arrange for a GLP inspection)5.3Are all equipment and testing procedures used in the laboratoryvalidated?Page 5 of 10
A.FACILITY INSPECTIONYES5.4Is the laboratory accredited for the tests to be performed?6Waste disposal6.1Is the disposal of biological specimens and sharps appropriate?B.DOCUMENTATIONNONAEssential Documents are those documents that individually and collectively permitevaluation of the conduct of a trial and the quality of the data produced. These documentsserve to demonstrate the compliance of the investigator, sponsor and monitor with thestandards of GCP and all applicable regulatory requirements. (ICH GCP section 8.1) WHOreference?Check the availability of the following documents:(During the planning stage, the following documents should begenerated before the conduct of the trial)YESNONAGeneral1.1Approved, signed and final version of the Protocol (includingamendments)1.2Final version of the Investigator’s Brochure1.3Information Leaflet, information regarding the trial in lay terms1.4Informed Consent Form (translation) and applicable procedure1.5Sample of the case report forms (CRF) as per protocolrequirements1.6Any other written information (e.g. advertisements)1.7IEC approval of advertisement for participant recruitment1.8Financial aspects of the trial as predefined in an agreementbetween the Investigator and the sponsor1.9Guaranteed indemnity / insurance document / statement1.10Signed agreements between involvedInvestigator/CRO, Investigator/Sponsor1.11Source documents and CRF verification procedure (SOP)available?1.12Clear documentation of transfer of responsibilities1.13All approval documentation:partiese.g. Independent Ethics Committee approval (Clearly statedwhich dated version of protocol and informed consent isapproved.) Regulatory approval. (Clearly stated which dated version ofprotocol and informed consent is approved.)Page 6 of 10
(During the planning stage, the following documents should begenerated before the conduct of the trial)YESNONAGeneral1.14List of Ethics Committee members1.15Latest signed and dated CV’s of investigators1.16Proof of GCP training of all study team members1.17Pre-trial GCP site assessment report (only at the Sponsor site)1.18List of DSMB members1.19Verify the availability of the Local Safety Monitor’s CV1.20Trial initiation visit , agenda and study team attendance list1.21Verify the availability of the Serious Adverse Event reportingforms and reporting procedures/timelines (including supportingSOP’s)Laboratory1.22Normal values / ranges for medical / laboratory / technicalprocedures as supplied by the laboratory / contract laboratory1.23Laboratory Certification1.24Laboratory Accreditation1.25Quality Control or quality assessment of laboratory by thesponsor1.26Validation methods where applicableInvestigational Product1.27Sample labels of IP (only at Sponsor)1.28All shipping records of IPs (dates, batch numbers)1.29Proof that conditions as stated in the protocol have beenmaintained during shipment and storage of products1.30CoA of IPs (Check stability, expiry dates)1.31Vaccine accountability records e.g. quantities ordered andreceived1.32Decoding procedures for blinded trials1.33Master randomization list (only at Sponsor site)1.34Instruction for handling of investigational product and trial relatedmaterials1.35Proof that the correct diluent has been packed according to thecorrect storage condition and shipped with the vaccine?Page 7 of 10
2ICH GCP section 8.3(In addition to having on file the aforementioned documents thefollowing documentation should be added to the files during theconduct of the trial)Documentation2.1Updates of Investigator’s Brochure e.g. ADRs2.2Any approved amendments too protocolo informed consent2.3IEC and regulatory approval of any new investigators, and theirCVs2.4Proof of GCP training2.5Updates of normal values / ranges for medical / laboratory /technical procedures as supplied by the laboratory / contractlaboratory2.6Vaccine accountability documentation and correct use of theproduct according to the protocol and IP management2.7Shipment documentation of any new batches of IPs includingCoA, batch release and temperature control.2.8Communications other than monitoring visitsYESNONAo Letterso Meeting minutes and agendaso Notes of telephone calls2.9Signed Informed Consents2.10Source documents, e.g. X-rays, serology printout, diary cards2.11Signed and dated CRFs2.12SAE reporting to sponsor2.13Reporting of any serious unexpected ADR and relevant safetyinformation to NRA and IEC where required2.14Progress reports to IEC2.15Participant screening log2.16Participant identification code list2.17Participant enrolment log2.18Study team signature sheet with delegated functions by PI2.19Retained biological samples (records, storage conditions)2.20All deviations e.g. inclusive/exclusive criteria (waiver) recordedPage 8 of 10
3ICH GCP section 8.4(Documentation after completion or termination of the trial)3.1IP accountability at site (final reconciliation)3.2Documentation on disposal of IPs3.3Completed participant identification code list3.4Audit Certificate (if applicable), i.e. if carried out3.5Final trial close-out monitoring report3.6Final report by investigator to IEC and regulatory authority (referto ICH GCP section 4.13)3.7Clinical study report (refer to ICH GCP section 5.22)3.8Treatment allocation and decoding documentation that haveoccurred available.3.9Is a follow up plan available (post trial period) for participantswith adverse events related to the IP as per protocol?C.INFORMED CONSENT PROCESSYES1Was the informed consent form version used the same as the oneapproved by the IEC/IRB?2Was a written SOP used to solicit informed consent?3Were all the participants given a copy of a signed informedconsent form?4Did all the participants sign the consent form prior to any studyrelated procedure?D.GENERAL INFORMATION1Ask for an organogram of the Trial Site/CRO and note the following points:NONA1.1number and categories of people employed1.2description of the qualifications, training and experience of the personnel1.3work load of study team1.4number of concurrent clinical studies performed on site and identification of participants toavoid confusion and mix-ups of IP’s administration2Ask for a description of the quality assurance system set up at the trial site.3Check the existence, availability, accessibility and validity of the operating procedures; askfor a list of the Standard Operating Procedures used for the trial.4Verify the availability of 100 % of all documentation particularly the ICF, CRF and sourcedocuments.Page 9 of 10
5Perform verification of Informed Consent forms as per NRA requirements.6Perform at least 25 % Source documentation versus CRFs verification7Perform a100 % accountability of IPE.REFERENCES1ICH Guideline for good clinical practice, recommended for adoption at step 4 of the ICHprocess on 1 May 19962Guidance on General Considerations for Clinical Trials (ICH-E8)3Guidelines for good clinical Practice (GCP) for trials on pharmaceutical products. WHOTechnical Report Series, No. 850, Annex 3, 1995Page 10 of 10
3.4 Audit Certificate (if applicable), i.e. if carried out 3.5 Final trial close-out monitoring report 3.6 Final report by investigator to IEC and regulatory authority (refer to ICH GCP section 4.13) 3.7 Clinical study report (refer to ICH GCP section 5.22) 3.8 Treatment allocation and decoding documentation that have occurred available.