Transcription
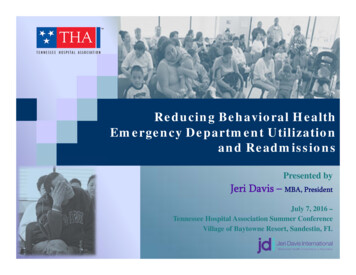
Reducing Behavioral HealthEmergency Department Utilizationand ReadmissionsPresented byJeri Davis – MBA, PresidentJuly 7, 2016 –Tennessee Hospital Association Summer ConferenceVillage of Baytowne Resort, Sandestin, FL
2Presentation OverviewI.The ProblemII. The CausesIII. The ImpactIV. The SolutionsA. Case Study 1: Hospital Association Collaboration SolutionB. Case Study 2: Internal Hospital SolutionC. Case Study 3: Community Collaboration SolutionD. Case Study 4: Payer Partnership SolutionV. The FutureVI. Summary 2016 JDi All Rights Reservedwww.jeridavisintl.com
3The Problem 2016 JDi All Rights Reservedwww.jeridavisintl.com
4The Problem Hospitals, nationally and in Tennessee, havebeen challenged by a shortage ofpsychiatric beds, access to services andgaps in service coordination. This has resulted in EDs overcrowded withpsychiatric and substance use patients, andexcessive holds for these patients. The problem is reaching crisis proportion,with recent studies revealing transferstaking as long as 2 to 10 days. 2016 JDi All Rights Reservedwww.jeridavisintl.com
5The ProblemBehavioral Health ED Utilization and Boarding is ReachingEpidemic ProportionsThe National PerspectiveOne in eight, or nearly 12 million of the 95 millionhospital emergency department visits, were for mentalhealth disorders, substance use or both. About 41% led to a hospital stay, 2.5 times the rate ofhospitalizations for other conditions. Behavioral Health visits to EDs are increasing at therate of 9% a year, often due to budget reductionsin public “safety net” community Behavioral Healthproviders. Behavioral Health services delivered through the ED requiremore than twice the time as the average medical protocoloffered in the same setting.Source: Agency for Healthcare Research & Quality Statistics 2010 (Reporting 2007 data) 2016 JDi All Rights Reservedwww.jeridavisintl.com
6The ProblemBehavioral Health ED Utilization and Boarding is ReachingEpidemic Proportions (cont’d) BH patients are likely to use the ED on multipleoccasions and to have multiple hospitalizations,compared to patients without psychiatricdisorders. Nearly half of EDs report operating at or abovecapacity, and 9 out of 10 hospitals report holdingor “boarding” admitted patients in the ED whilethey await inpatient beds.Sources: J. Baillargeon, C.R. Thomas and B. Williams et al., Emergency department utilization patterns among uninsured patients with psychiatric disorders, Psychiatry Serv 59 (2008), pp. 808–811.Mental Disorders and/or Substance Abuse Related to One of Every Eight Emergency Department Cases. AHRQ News and Numbers, July 8, 2010. Agency for Healthcare Research and Quality, Rockville, MD.http://www.ahrq.gov/news/nn/nn070810.htm Ibid. 2016 JDi All Rights Reservedwww.jeridavisintl.com
7The ProblemBehavioral Health ED Utilization and Boarding is ReachingEpidemic Proportions (cont’d) Of these, 63.7% were related to mental healthproblems, 24.4% involved substance use disordersand 11.9% involved co‐occurring psychiatric andsubstance use disorders. Among ED visits involving mental health andsubstance use disorders, 42.7% were for mooddisorders, 26.1% for anxiety disorders and 22.9%for alcohol‐related conditions.Source: Mental Disorders and/or Substance Abuse Related to One of Every Eight Emergency Department Cases. AHRQ News and Numbers, July 8, 2010. Agency for Healthcare Research and Quality, Rockville, MD.http://www.ahrq.gov/news/nn/nn070810.htm Ibid. 2016 JDi All Rights Reservedwww.jeridavisintl.com
8The ProblemBehavioral Health ED Utilization and Boarding is ReachingEpidemic Proportions – Tennessee Data 2016 JDi All Rights Reservedwww.jeridavisintl.com
9The ProblemBehavioral Health ED Utilization and Boarding is ReachingEpidemic ProportionsTABLE 1 ‐ 2014 Behavioral Health Claim Volumes and Estimated Costs byPayerED OnlyDiagnosis GroupBehavioral Health Other DxPayerVisits%EstimatedCost%Blue Cross61,6309.14% 70,185,84910.78%28,6839.57% 84% 61,251,0019.41%24,3818.13% 284,956,4929.50%179,38826.59% 145,720,44022.38%28,0629.36% 265,395,4078.84%Medicare157,22523.31% 194,469,53129.87%170,27856.81% 1,630,911,80754.35%34,8485.17% 31,672,1234.86%9,0423.02% 103,080,1273.43%TennCare/Medicaid188,63127.96% 147,772,11322.70%39,29313.11% 390,539,69113.01%All Payers674,635Blue Cross8,235Commercial 651,071,05710.38% 5,482,401299,739 3,000,910,76510.19%3,1257.52% 13,109,7155.66%7,2299.11% 5,038,0209.37%6,74916.24% 33,595,27114.50%Medically Indigent/self Pay22,15727.94% 14,697,65927.33%3,3608.09% 13,685,2935.91%Medicare17,73722.36% 13,688,38325.45%16,36739.39% 104,355,08845.03%Other3,5374.46% 2,497,4294.64%2,9877.19% 19,315,1998.34%TennCare/Medicaid20,42025.75% 12,380,96223.02%8,96621.58% 47,662,10120.57%All Payers79,315 53,784,85441,554 otalSource: Cleave, M; THA Claims Data, 2014AdmissionsMedically Indigent/Self PayOtherBehavioral Health Primary DxIP (Inc ED) 2016 JDi All Rights Reservedwww.jeridavisintl.com
10The ProblemBehavioral Health ED Utilization and Boarding is ReachingEpidemic ProportionsTABLE 2 ‐ 2014 Behavioral Health Claim Volumes and Estimated Costs ByTop 6 Other DxDiagnosis GroupsTop 6 ‐ Behavioral HealthOther DxSource: Cleave, M; THA Claims Data, 2014ED OnlyEstimatedCost64.06% 335,649,27354.40%86,300IP (Inc ED)Estimated%Cost33.13% 892,966,030 34.95%75,71111.65% 85,916,92213.92%41,92716.09% 405,803,293 15.88%DEPRESSIVE DISORDER NEC51,0867.86% 62,066,64210.06%47,06418.07% 472,393,310 18.49%DEMEN NOS W/O BEHV DSTRB(BEGIN 2011)MANIC‐DEPRESSIVE NOSALCOHOL ABUSE‐UNSPEC13,5042.08% 19,323,1083.13%25,8739.93% 197,363,1537.72%21,38611,7163.29%1.80% 21,456,165 18,683,2153.48%3.03%8,7884,6453.37%1.78% 77,965,406 46,200,6733.05%1.81%Behavioral Health Diagnosis inthe Other Diagnosis fieldsTOBACCO USE DISORDER(BEGIN 1994)ANXIETY STATE NOSVisits416,293%%Admissions%Top 6 d Total (ALL Other DxGroups)649,886617,056,555260,5092,555,062,934 2016 JDi All Rights Reservedwww.jeridavisintl.com
11The ProblemBehavioral Health ED Utilization and Boarding is ReachingEpidemic Proportions (cont’d)TABLE 3 ‐ 2014 Behavioral Health Claim Volumes and Estimated Costs by Top9 Primary DxDiagnosis GroupTop 9 ‐ Behavioral HealthPrimary DxSource: Cleave, M; THA Claims Data, 2014DiagnosisANXIETY STATE NOSDEPRESSIVE DISORDER NECALCOHOL ABUSE‐UNSPECPSYCHOSIS NOSRECUR DEPR PSYCH‐SEVERESCHIZOAFFECTIVE‐UNSPECAFFECTIVE PSYCHOSIS NOSDEMEN NOS W BEHAV DISTRB(BEGIN 2011)REC DEPR 1128212ED OnlyEstimatedCost25% 7,990,69813% 5,096,26913% 6,679,5147.16% 4,558,2450.05% 61,7730.35% 152,1820.33% 139,2050% 1,526,511%0% 2%1,824IP (Inc ED)%Estimated%Cost0.65% 746,002 0.51%5.73% 5,706,034 3.92%0.57% 518,442 0.36%5.94% 8,568,622 5.89%21.63% 28,093,062 19.31%10.18% 19,785,962 13.60%9.79% 13,598,620 9.35%6.15% 11,487,598 7.89%6.78% 10,895,814Top 9 Subtotal38,59926,215,46718,13999,400,156Grand Total (ALL Diagnoses)64,68544,512,30626,903145,506,5807.49% 2016 JDi All Rights Reservedwww.jeridavisintl.com
12The ProblemBehavioral Health ED Utilization and Boarding is ReachingEpidemic Proportions (cont’d)TABLE 4 ‐ 2014 Behavioral Health Diagnoses ‐ Uninsured Patients Only Listedin Any Diagnostic FieldClaim TypeEmergency DepartmentInpatientSource: Cleave, M; THA Claims Data, 2014Behavioral Health Diagnosis Listed inany Diagnosis FieldNonpsychotic Mental DisorderNonpsychotic Mental DisorderPsychosesPsychosesNonpsychotic Mental DisorderNonpsychotic Mental DisorderPsychosesPsychosesPayer TypeSelf PayMedically Indigent, Free CareSelf PayMedically Indigent, Free CareSelf PayMedically Indigent, Free CareSelf PayMedically Indigent, Free CareNumber of Claims178,3097,73414,4841,01822,9611,6305,2451,586 2016 JDi All Rights Reservedwww.jeridavisintl.com
13The ProblemThe Opiate Epidemic in TN and NationallyNational Data Indicates that the Following Groups areat Especially High Risk for Prescription Drug Abuse: Men ages 25 to 54 have the highest numbers ofprescription drug overdoses and are about twotimes more likely to die from an overdose thanwomen. In the United States, about 18 women die each dayfrom prescription painkiller overdoses. For everyone woman who dies, 30 more visit an emergencydepartment for painkiller misuse or abuse.Source: Trust for America’s Health. (2013) Prescription Drug Abuse: Strategies to Stop the Epidemic 2013. Accessed via the web: xDrugAbuseRptFINAL.pdf 2016 JDi All Rights Reservedwww.jeridavisintl.com
14The ProblemThe Opiate Epidemic in TN and Nationally (cont’d)National Data Indicates that the Following Groups areat Especially High Risk for Prescription Drug Abuse:(cont’d) While rates are high in both urban and ruralcommunities, people in rural counties are abouttwice as likely to overdose on prescription drugs aspeople in big cities. Nearly one in 12 high school seniors reportednonmedical use of Vicodin and one in 20 reportednonmedical use of OxyContin. One in eight active duty military personnel is acurrent user of illicit drugs or is misusingprescription drugs. 2016 JDi All Rights Reservedwww.jeridavisintl.com
15The ProblemThe Opiate Epidemic in TN and Nationally (cont’d) By the CDC’s estimate, there are atleast 1,074,813 Tennesseans, orabout 1 in 6, misusing or abusingopioids or in treatment. In 2012, prescription opioidssurpassed alcohol as the primarysubstance of abuse.* Tennesseans were more than threetimes more likely to identifyprescription opioids as theirprimary substance of abuse thanthe national average.Source: Substance Abuse and Mental Health Services administration. (2012). Treatment Episode Data Set—Admissions (TEDS‐A). U.S. Department of Health and Human Services, Washington, D.C.*for people whose treatment was funded through the Tennessee Department of Mental Health and Substance Abuse Services. 2016 JDi All Rights Reservedwww.jeridavisintl.com
16The ProblemImpact of Behavioral Health Co-Morbidities on Medicaid CostsN 1,725Source: Richard Louis, Consultant 2016 JDi All Rights Reservedwww.jeridavisintl.com
17The ProblemCo-Occurring Disorders Exacerbate Mental Health ProblemsDepression is Commonly Present in Patients withCoronary Heart Disease (CHD) Depression is 3 times more common in patientsafter an acute myocardial infarction (AMI) than inthe general community. Depression is also independently associated withincreased cardiovascular morbidity and mortality.Source: Thombs BD, Bass EB, Ford DE, Stewart KJ, Tsilidis KK, Patel U, Fauerbach JA, Bush DE, Ziegelstein RC. Prevalence of depression in survivors of acute myocardial infarction. J Gen Intern Med. 2006; 21: 30–38Bartels, S and Desilets R (2012) Health promotion programs for people with serious mental illness (Prepared by the Dartmouth Health Promotion Research Team) Washington DC, SAMHSA‐HRSA Center for IntegratedHealth Solutions 2016 JDi All Rights Reservedwww.jeridavisintl.com
18The ProblemCo-Occurring Disorders Exacerbate Mental Health Problems (cont’d)Smoking (both Marijuana and Tobacco) are HighlyAssociated with Increased Risk of COPD. Smokers who reported using both marijuana andtobacco were almost 2.5 times more likely thannonsmokers to have respiratory symptoms. This same group was nearly 3 times more likely thannonsmokers to have COPD as defined by Spirometric testing.Source: Wan C. Tan, MB, Christine Lo, BSc, Aimee Jong, BSc, Li Xing, MSc, Mark J. FitzGerald, MB, William M. Vollmer, PhD, Sonia A. Buist, MD PhD, and Don D. Sin, MD PhD, for the Vancouver Burden of Obstructive LungDisease (BOLD) Research Group. Marijuana and chronic obstructive lung disease: a population‐based study. 2016 JDi All Rights Reservedwww.jeridavisintl.com
19The ProblemCo-Occurring Disorders Exacerbate Mental Health Problems (cont’d) Persons with major mental disorders lose 25 to 30years of potential life in comparison with thegeneral population due to prematurecardiovascular mortality.Source: Bartels, S and Desilets R (2012) Health promotion programs for people with serious mental illness (Prepared by the Dartmouth Health Promotion Research Team) Washington DC, SAMHSA‐HRSA Center forIntegrated Health Solutions 2016 JDi All Rights Reservedwww.jeridavisintl.com
20The Causes 2016 JDi All Rights Reservedwww.jeridavisintl.com
21The CausesAccording to the AHA, the Primary Reasons forOvercrowding in EDs by Patients with Mental Healthand/or Substance Use are as Follows: Years of funding cuts to public mental healthorganizations The resulting loss of thousands of inpatient beds atstate and county facilities Increased demand for services Barriers to access 2016 JDi All Rights Reservedwww.jeridavisintl.com
22The CausesThe Need is Increasing The need for Behavioral Health services at alllevels, long and short‐term, has growndramatically over the last several years as aresult of: Increased stress and illness in the community due toeconomic conditions and aging Baby Boomers Increased acuity and complexity of patients Reduction of state hospital beds without sufficient,timely and comprehensive service replacement Shutting down of community‐based resources due tobudget cuts Increasing suicide rates 2016 JDi All Rights Reservedwww.jeridavisintl.com
23The CausesRising Suicide Rates Rates of suicide deaths are rising in the U.S. Therates jumped 24% from 1999 to 2014, from 10.5to 13 per 100,000 people, according to an April2016 report from the Centers for Disease Controland Prevention.Source: Peterson, Andrea, “Researchers Study New Ways to Treat Suicide Risk” The Wall Street Journal, 2016 June 21 D4 2016 JDi All Rights Reservedwww.jeridavisintl.com
24The CausesRising Suicide Rates in Tennessee In any given day, three people in Tenn
Sources: J. Baillargeon, C.R. Thomas and B. Williams et al., Emergency department utilization patterns among uninsured patients with psychiatric disorders, Psychiatry Serv 59 (2008), pp. 808–811. Mental Disorders and/or Substance Abuse Related to One of Every Eight Emergency Department Cases. AHRQ News and Numbers, July 8,2010. Agency for .