Transcription
Consortium for Oral Health Systems Integration andImprovementOral Health Quality Indicators for the Maternal and ChildHealth Population: User Guide and Technical SpecificationsMarch 2022Prepared by:Dental Quality AllianceNational Maternal and Child Oral Health Resource Center
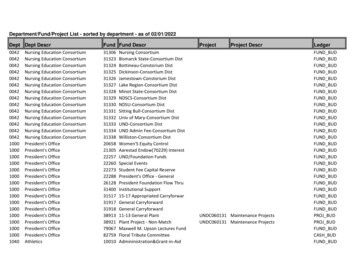
Table of ContentsPreface . 1A. Purpose . 1B. Organization of User Guide. 2C. Technical Assistance and Contacts . 3Section 1: Introduction . 4A. Background . 4B. Maternal and Child Health Oral Health Quality Indicators . 4C. Level of Measurement . 6D. Readiness Assessment: Evaluating Capacity to Measure . 7Section 2: Quality Indicator Summaries . 7Section 3: General Guidelines for Data Collection, Preparation, and Reporting 23A. Data Sources and Critical Data Elements. 23B. Time Frame . 24C. Level of Reporting . 24D. Included Populations and Age Eligibility . 25E. Data Collection and Quality . 25F. Stratification . 26G. Reporting Missing and Invalid Data . 27H. Minimum Denominator Size and Data Suppression . 27I. Guidance for Indicators Reported on Using Specific Data Sources . 27Appendix 1. Technical Specifications . 29A. Oral Health Quality Indicators for Women of Child-Bearing Age and PregnantWomen . 31Indicator W.1. Percentage of Pregnant Women Reporting Difficulty GettingDental Care During Pregnancy . 31Indicator W.2. Percentage of Pregnant Women Who Had Insurance to CoverDental Care During Pregnancy . 36Indicator W.3. Percentage of Pregnant Women Who Reported Having TheirTeeth Cleaned by a Dentist or Dental Hygienist During Pregnancy . 41Indicator W.4. Percentage of Women of Child-Bearing Age (ages 18–44) WhoReport Having a Visit to a Dentist or Dental Clinic in the Past Year . 46ii
Indicator W.5. Percentage of Pregnant Women Reporting That They Neededto See a Dentist for a Problem During Pregnancy . 51B. Oral Health Quality Indicators for Children . 56Indicator C.1. Dentists Who Actively Participate in Medicaid per 1,000 EPSDTEligible Enrolled Children . 56Indicator C.2. Utilization of Services, Dental Services (NQF #2511) . 59Indicator C.3. Preventive Services for Children, Dental and Oral HealthServices . 60Indicators C.4./C.5. Prevention: Topical Fluoride for Children, Dental (NQF#2528) and Oral Health Services . 61Indicator C.6. Prevention: Sealant Receipt on Permanent 1st Molars . 62Indicator C.7. Prevention: Sealant Receipt on Permanent 2nd Molars. 63Indicator C.8. Percentage of Kindergarten Children with Dental CariesExperience (Treated or Untreated Tooth Decay) . 64Indicator C.9. Percentage of Third-Grade Children with Dental CariesExperience (Treated or Untreated Tooth Decay) . 67Indicator C.10. Percentage of Kindergarten Children with Urgent DentalTreatment Needs . 70Indicator C.11. Percentage of Third-Grade Children with Urgent DentalTreatment Needs . 73Appendix 2. Resources, Acknowledgements, and Attributions. 76A. Consortium for Oral Health Systems Integration and Improvement (COHSII)Maternal and Child Health Oral Health Quality Indicators Reports andResources . 76B. Additional Online Resources . 76C. Acknowledgements . 77D. Indicator Sources. 78E. Proprietary Codes . 79F. Citation and Funding Acknowledgement . 79iii
PrefaceA. PurposeThis user guide provides guidance on implementing oral health quality indicators for thematernal and child health (MCH) population.Importance of MCH Oral Health Quality IndicatorsTooth decay is the most common chronic disease among children in the United States,causing pain and other problems that can interfere with eating, sleeping, socializing,and learning. Tooth decay can also lead to more serious health problems. The need fororal health care is one of the most prevalent unmet health care needs reported byparents. Poor oral health among pregnant women may contribute to adverse birthoutcomes, and a mother’s oral health status can influence her child’s oral health status.Quality indicators are foundational to quality improvement in health care. They aim todetect how well systems are working, allow for comparisons between entities thatpromote shared learning, enable assessments of improvement over time, and improvetransparency. To date, oral health care quality indicators for the MCH population havebeen spread across different programs and data sources and inconsistently reported.Lack of consistent and standardized measurement is a barrier to achieving system-wideimprovements in care and outcomes.This set of standardized indicators has been identified through expert consensusprocesses as being both feasible and meaningful for measuring and improving thequality of care in MCH programs. A combination of indicators is necessary to show howwell MCH systems are providing access to care, delivering evidence-based care, andimproving population health.Intended UseThe MCH oral health quality indicators constitute a standardized and aligned qualitymeasurement system designed to promote state efforts to monitor and improve thequality of oral health care for the MCH population. Incorporating indicators into stateoral health quality measurement and surveillance plans for reporting over time will helpstates. Assess current system performance.Identify priority areas.Develop action plans to drive improvements in care quality and outcomes.Assess progress in achieving improvement goals.The indicators are designed to be used as a set to provide a more complete picture ofcare than is possible when using indicators in isolation. It is important to recognize that1
each indicator provides a broad assessment about the extent to which access, use,process, and outcomes goals are being achieved. States seeking to improve on anyindicator will need to evaluate the care domain addressed by the indicator in moredepth to better understand the underlying factors contributing to current performanceand identify improvement strategies.Intended UsersThe indicators are designed for use by the state oral healthprogram in partnership with the state MCH program, thestate department of health, and the state Medicaid agency.Implementation of these indicators will require involvement ofepidemiologists and/or data analysts within these programs.With resources and technical assistance from the Consortiumfor Oral Health Systems Integration and Improvement(COHSII), state oral health programs can conduct a readinessassessment and report on the indicators.Implementation ofthese indicators willrequire involvement ofepidemiologists and/ordata analysts withinthese programs.B. Organization of User GuideThis user guide is organized into six sections:Section 1: IntroductionContent. This section provides background information on the selection of the MCH oralhealth quality indicators.Intended Audience. This section is designed for stakeholders interested in monitoringand improving oral health care quality for the MCH population, including directors andstaff of state oral health programs, MCH programs, and Medicaid agencies.Section 2: Quality Indicator SummariesContent. This section includes an at-a-glance summary for each quality indicator thathighlights the main features and importance of the indicator.Intended Audience. This section is designed to aid all stakeholders in understanding andcommunicating the purpose and characteristics of each indicator.Section 3: General Guidelines for Data Collection, Preparation, and ReportingContent. This section describes data sources, data elements within those data sources,and other considerations when preparing to report the quality indicators.2
Intended Audience. This section is designed for epidemiologists and/or data analystswho will be calculating the indicators.Appendix 1: Technical SpecificationsContent. This section provides a detailed, step-by-step approach for calculating eachquality indicator.Intended Audience. This section is designed for epidemiologists and/or data analystswho will be calculating the indicators.Appendix 2: Resources, Acknowledgements, and AttributionsContent. This section includes additional online resources available to assist withindicator reporting and use, a list of Quality Indicator Advisory Team (QIAT) membersand other contributors, and data sources and code sets used for indicator reporting.Intended Audience. This section is designed for all stakeholders.C. Technical Assistance and ContactsTechnical assistance is available to state implementation teams for the collection,analysis, and interpretation of MCH oral health quality indicator data.Contact the Dental Quality Alliance (DQA) (DQA@ada.org, www.ada.org/dqa) to beconnected to the appropriate technical advisor.National Maternal and Child Oral Health Resource Center (OHRC):OHRCinfo@georgetown.edu, www.mchoralhealth.org3
Section 1: IntroductionThis user guide provides guidance for reporting on oral health quality indicators for theMCH population during 2022.1A. BackgroundCOHSII established a QIAT to identify a set of MCH oral health quality indicators tomonitor and improve oral health care services delivered to the MCH population inpublic health programs and systems of care. The QIAT identified these indicators bydeveloping a quality measurement and performance improvement framework,conducting a broad environmental scan of existing oral health care quality indicatorsand using a consensus-based process to determine the indicator set (find moreinformation on the Oral Health Quality Indicators for the MCH Population webpage).COHSII is funded by the Maternal and Child Health Bureau (MCHB), Health Resourcesand Services Administration. COHSII is led by OHRC in partnership with the Associationof State and Territorial Dental Directors and DQA. COHSII works with key stakeholders toimprove systems of care in support of a quality improvement, patient-centeredapproach to address the oral health needs of the MCH population.The MCH oral health quality indicators are national indicators; their scores arecalculated using the following data sources collected at the state level: Basic Screening Survey (BSS)Behavioral Risk Factor Surveillance System (BRFSS)Pregnancy Risk Assessment Monitoring System (PRAMS)Medicaid administrative claims and enrollment dataThe availability of standardized data sources was an important consideration whenselecting the indicators. Indicators were selected based on their potential to drivemeaningful improvements in quality and on their near-term implementation feasibility.B. Maternal and Child Health Oral Health Quality IndicatorsThe MCH oral health quality indicators span the quality domains of access, utilization,process, and outcomes (Figure 1). As the DQA User Guide notes: “There is no single‘magic’ measure. Rather, a set of carefully chosen measures can be used to provide amore complete picture of care, establish baseline performance, identify improvementopportunities, and monitor progress toward achieving the ultimate care goals.”The indicators are grouped by two MCH sub-populations: (1) women of child-bearingage and pregnant women and (2) children. The indicators are listed below. Section 2provides non-technical summaries of the indicators. Detailed technical specifications2022 represents when indicators are reported and not when data for indicators were collected.Data collection timeframes vary by indicator and are noted within the specifications for eachindicator.14
for epidemiologists and data analysts who calculate the indicators are provided inAppendix 1.Figure 1. Measure Sets to Support Attaining Ultimate Care GoalQuality Indicators for Women of Child-Bearing Age and Pregnant WomenAccess Percentage of pregnant women reporting difficulty getting dental care during pregnancy(Data source: PRAMS) Percentage of pregnant women who had insurance to cover dental care during pregnancy(Data source: PRAMS)Utilization Percentage of pregnant women who reported having their teeth cleaned by a dentist ordental hygienist during pregnancy (Data source: PRAMS) Percentage of women of child-bearing age (ages 18–44) who report having a visit to adentist or dental clinic in the past year (Data source: BRFSS)Outcome Percentage of pregnant women reporting that they needed to see a dentist for a problemduring pregnancy (Data source: PRAMS)Quality Indicators for ChildrenAccess Dentists who actively participate in Medicaid per 1,000 EPSDT-eligible enrolled children (Datasource: Medicaid enrollment and claims)5
Utilization Percentage of children who had a dental visit in the last 12 months (Data source: Medicaidenrollment and claims)* † Percentage of children at elevated risk receiving preventive dental services (Data source:Medicaid enrollment and claims)*Process Percentage of children receiving at least two topical fluoride applications as a dental or oralhealth service (Data source: Medicaid enrollment and claims)* Percentage of children who have ever received sealants on permanent first molar teeth bythe10th birthdate (Data source: Medicaid enrollment and claims)* Percentage of children who have ever received sealants on permanent second molar teethby the 15th birthdate (Data source: Medicaid enrollment and claims)*Outcome Percentage of kindergarten children with dental caries experience (treated or untreatedtooth decay) (Data source: Basic Screening Survey [BSS]) Percentage of third-grade children with dental caries experience (treated or untreatedtooth decay) (Data source: BSS) Percentage of kindergarten children with urgent dental treatment needs (Data source: BSS) Percentage of third-grade children with urgent dental treatment needs (Data source: BSS)*Developerand steward: DQA† In 2021, two indicators were combined into one by DQAC. Level of MeasurementQuality indicators can be reported at different levels. DQA notes that to achievesystem-level improvement, it is important to have measurement that is horizontallyaligned across public and private sectors and vertically aligned from the point of careto the broader systems level. “Starting with broad populations, national goals guide thedevelopment of program-level measures, which are then used to derive practice- andclinician-level measures.”2 Thus, achieving improvement at the broader systems levelusing the MCH oral health quality indicators requires engagement of stakeholders andalignment of measures across all system levels (Figure 2).Dental Quality Alliance. 2019. Quality Measurement in Dentistry: A Guidebook. Chicago: IL:American Dental Association.26
Figure 2. Measurement Alignment Across Reporting LevelsFederal coremeasure setsProgram, planmeasuresPractice, clinicmeasuresFigure adapted from Dental Quality Alliance. 2018. Alignment and Harmonization in Reporting Quality:Establishing Reliability Across Reporting Levels. Chicago, IL: American Dental Association.D. Readiness Assessment: Evaluating Capacity to MeasureBefore beginning to report on the MCH oral health quality indicators, states areencouraged to conduct a readiness assessment to determine what can be measuredin the near term and what will require building data collection and reporting capacity.It is envisioned that staff in the state oral health program will take the lead on thereadiness assessment in partnership with state epidemiologists, data analysts, the stateMCH director, and Medicaid staff. Readiness assessment results can be used todevelop an action plan with specific time-based goals to obtain the data and analyticcapacity necessary to report on MCH oral health quality indicators. Contact COHSII foraccess to an online readiness assessment form that provides tips for how to interpretyour results.Section 2: Quality Indicator SummariesThis section includes a one-page summary for each quality indicator that highlights themain features of each indicator and explains its importance. These summaries areintended to aid program administrators and staff in understanding and communicatingthe purpose and characteristics of each indicator.7
Indicator W.1. Percentage of Pregnant Women Reporting Difficulty Getting Dental CareDescription:The percentage of pregnant women reporting difficulty getting dental care.What data source isused?The Pregnancy Risk Assessment Monitoring System (PRAMS) is a surveillanceproject of the Centers for Disease Control and Prevention (CDC) and statehealth departments. PRAMS collects self-reported data on women’s attitudesand experiences before, during, and shortly after pregnancy.Who is the targetpopulation?PRAMS is an state-level survey of resident women in the state who gave birthto a live-born infant during the year.Which PRAMS questionis used for this indicator?Standard Question Y6: Did any of the following things make it hard for you togo to a dentist or dental clinic during your most recent pregnancy? For eachitem, check No if it was not something that made it hard for you or Yes if it was.NoYesa. I could not find a dentist or dental clinic that would takepregnant patientsrrb. I could not find a dentist or dental clinic that would takeMedicaid patientsrrc. I did not think it was safe to go to the dentist during pregnancyrrd. I could not afford to go to the dentist or dental clinicrrHow is the indicatormeasured?The indicator is expressed as a percentage [numerator/denominator x 100%].Numerator: The subset of women in the denominator whoanswered “Yes” to any of the items about difficulty gettingdental care in PRAMS standard question Y6Denominator: Number of women who answered PRAMS standardquestion Y6Are any PRAMSrespondents excluded?Women who responded to the PRAMS questionnaire overall but did not answerstandard question Y6 are excluded from the indicator.What does this indicatormeasure and why is itimportant?This indicator is a measure of access to oral health care among pregnantwomen. Medical and oral health professional organizations, such as theAmerican College of Obstetricians and Gynecologists and the AmericanDental Association, recommend that pregnant women have a visit with adentist before and during pregnancy to get their oral health assessed, obtainpreventive services, receive any treatment needed, and receive guidanceabout good eating and oral hygiene practices.iAre there any limitationsto this indicator?PRAMS data are collected only from women who delivered a live-born infant,not all pregnant women. PRAMS data are self-reported and may be subject tovarious types of response and measurement bias, such as inaccurate recall orresponses that are influenced by what is “socially acceptable” rather thanwhat the “true” answer would be. Not all states conduct PRAMS every year.Where can I get moreinformation aboutPRAMS? Additional information about PRAMS is available from CDC.Each state has a PRAMS coordinator.I OralHealth Care During Pregnancy Expert Workgroup. 2012. Oral Health Care During Pregnancy: A National ConsensusStatement. Washington, DC: National Maternal and Child Oral Health Resource Center.8
Indicator W.2. Percentage of Pregnant Women Who Had Insurance to Cover Dental Care DuringPregnancyDescription:Percentage of pregnant women reporting that they had insurance to coverdental care during pregnancy.What data source isused?The Pregnancy Risk Assessment Monitoring System (PRAMS) is a surveillanceproject of the Centers for Disease Control and Prevention (CDC) and statehealth departments. PRAMS collects self-reported data on women’s attitudesand experiences before, during, and shortly after pregnancy.PRAMS is an state-level survey of resident women in the state who gave birthto a live-born infant during the year.Standard Question Y7: This question is about the care of your teeth during yourmost recent pregnancy. For each item, check No if it is not true or does notapply to you or Yes if it is true.No Yesra. I knew it was important to care for my teeth and gums during my rpregnancyrb. A dental or other health care worker talked with me about how rto care for my teeth and gumsrrc. I had insurance to cover dental care during my pregnancyWho is the targetpopulation?Which PRAMS questionis used for this indicator?d. I needed to see a dentist for a probleme. I went to a dentist or dental clinic about a problemHow is the indicatormeasured?rrrrThe indicator is expressed as a percentage [numerator/denominator x 100%].Numerator: The subset of women in the denominator whoanswered “Yes” to the response option: “I had insurance tocover dental care during my pregnancy”Denominator: Number of women who answered “yes” or “no” tostandard question Y7, response option “I had insurance to coverdental care during my pregnancy”Are any PRAMSrespondents excluded?What does this indicatormeasure and why is itimportant?Are there any limitationsto this indicator?Where can I get moreinformation aboutPRAMS?Women who responded to the PRAMS questionnaire overall but did not answerstandard question Y7, response option “I had insurance to cover dental careduring my pregnancy” are excluded from the indicator.This indicator is a measure of access to oral health care among pregnantwomen. Medical and oral health professional organizations, such as theAmerican College of Obstetricians and Gynecologists and the AmericanDental Association, recommend that pregnant women have a visit with adentist before and during pregnancy to get their oral health assessed, obtainpreventive services, receive any treatment needed, and receive guidanceabout good eating and oral hygiene practices.iPRAMS data are collected only from women who delivered a live-born infant,not all pregnant women. PRAMS data are self-reported and may be subject tovarious types of response and measurement bias, such as inaccurate recall orresponses that are influenced by what is “socially acceptable” rather thanwhat the “true” answer would be. Not all states conduct PRAMS every year. Additional information about PRAMS is available from CDC. Each state has a PRAMS coordinatorI OralHealth Care During Pregnancy Expert Workgroup. 2012. Oral Health Care During Pregnancy: A National ConsensusStatement. Washington, DC: National Maternal and Child Oral Health Resource Center.9
Indicator W.3. Percentage of Pregnant Women Who Reported Having Their Teeth Cleaned by aDentist or Dental Hygienist During PregnancyDescription:Percentage of pregnant women reporting that they had their teeth cleanedby a dentist or dental hygienist during pregnancy.What data source isused?The Pregnancy Risk Assessment Monitoring System (PRAMS) is a surveillanceproject of the Centers for Disease Control and Prevention (CDC) and statehealth departments. PRAMS collects self-reported data on women’s attitudesand experiences before, during, and shortly after pregnancy.Who is the targetpopulation?PRAMS is an state-level survey of resident women in the state who gave birthto a live-born infant during the year.Which PRAMS questionis used for this indicator?Core Question 17: During your most recent pregnancy, did you have yourteeth cleaned by a dentist or dental hygienist?r Nor YesHow is the indicatormeasured?The indicator is expressed as a percentage [numerator/denominator x 100%].Numerator: The subset of women in the denominator whoanswered “yes” to core question 17Denominator: Number of women who answered “yes” or “no” tocore question 17Are any PRAMSrespondents excluded?Women who responded to the PRAMS questionnaire overall but did not answercore question 17 are excluded from the indicator.What does this indicatormeasure and why is itimportant?This indicator is a measure of utilization of oral health care services by pregnantwomen. Medical and oral health professional organizations, such as theAmerican College of Obstetricians and Gynecologists and the AmericanDental Association, recommend that pregnant women have a visit with adentist before and during pregnancy to get their oral health assessed, obtainpreventive services, receive any treatment needed, and receive guidanceabout good eating and oral hygiene practices.iAre there any limitationsto this indicator?PRAMS data are collected only from women who delivered a live-born infant,not all pregnant women. PRAMS data are self-reported and may be subject tovarious types of response and measurement bias, such as inaccurate recall orresponses that are influenced by what is “socially acceptable” rather thanwhat the “true” answer would be. Not all states conduct PRAMS every year.Where can I get moreinformation aboutPRAMS? Additional information about the PRAMS survey is available from CDC.Each state has a PRAMS coordinator.I OralHealth Care During Pregnancy Expert Workgroup. 2012. Oral Health Care During Pregnancy: A National ConsensusStatement. Washington, DC: National Maternal and Child Oral Health Resource Center.10
Indicator W.4. Percentage of Women of Child-Bearing Age (ages 18–44) Who Report Having aVisit to a Dentist or Dental Clinic in the Past YearDescription:Percentage of women of child-bearing age (ages 18–44) who report having aWhat data source isused?Who is the targetpopulation?Which BRFSS question isused for this indicator?visit to a dentist or dental clinic in the past year.The Behavioral Risk Factor Surveillance System (BRFSS) is a system of telephonesurveys that collect self-reported data about U.S. residents regarding theirhealth-related risk behaviors, chronic health conditions, and use of preventiveservices. BRFSS is sponsored by the Centers for Disease Control and Prevention(CDC) along with other federal agencies. The oral health module is a rotatingcore that is included in the BRFSS questionnaire in even-number years.BRFSS is a state-level survey of U.S. adults ages 18 and older. The targetpopulation for this indicator is women ages 18–44.Section 7: Oral Health, Question COH.01: Including all types of dentists, suchas orthodontists, oral surgeons, and all other dental specialists, as well asdental hygienists, how long has it been since you last visited a dentist or adental clinic for any reason? [Response options only read if necessary.]a.b.c.d.e.f.g.How is the indicatormeasured?Within the past year (anytime less than 12 months ago)Within the past 2 years (1 year but less than 2 years ago)Within the past 5 years (2 years but less than 5 years ago)5 or more years agoDon’t know/Not sure (do not read)Never (do not read)Refused (do not read)The indicator is expressed as a percentage [numerator/denominator x 100%].Numerator: The subset of women in the denominator whoreported visiting a dentist or dental clinic within the past yearDenominator: Number of female respondents, ages 18–44, whoanswered core question COH.01Are any BRFSSrespondents excluded?What does this indicatormeasure and why is itimportant?Are there any limitationsto this indicator?Where can I get moreinformation?Respondents who are not female, and female respondents ages 45 and olderare excluded. Women ages 18–44 who responded to the BRFSS questionnaireoverall but did not answer core question 17 (or have responses marked as“don’t know/not sure” or “refused”) also are excluded.This indicator is a measure of utilization of oral health care services by womenof child-bearing age. Ro
Health Population: User Guide and Technical Specifications March 2022 Prepared by: Dental Quality Alliance National Maternal and Child Oral Health Resource Center . ii Table of Contents . Data collection timeframes vary by indicator and are noted within the specifications for each