Transcription
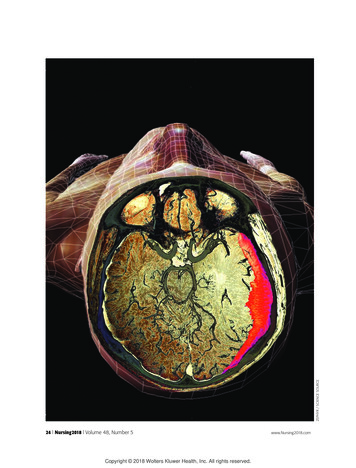
ZEPHYR / SCIENCE SOURCE24 l Nursing2018 l Volume 48, Number 5Copyright 2018 Wolters Kluwer Health, Inc. All rights reserved.www.Nursing2018.com
1.0ANCCCONTACT HOURSUBDURAL HEMATOMA (SDH) ischaracterized by a collection of bloodor fluid blood products in the spacebetween the dura mater and arachnoid or pial layer in the brain. AnSDH can occur spontaneously orresult from a head injury or variousother pathologies.An SDH is classified as acute,chronic, or subacute based on thetiming of occurrence and brain imaging. Morbidity and mortality associated with an SDH increases with ageand exposure to anticoagulant andantiplatelet therapy.1-3Chronic SDH (cSDH) in adults,the focus of this article, typically develops 2 to 3 weeks after the incitingevent and often has a poor prognosis. Because prompt diagnosis andtreatment is essential to prevent disability or death, this article discussesnursing assessment and interventionsthat may improve patient outcomesin patients with cSDH.SDH: Surprisingly commonData collected from the United Statescensus bureau show that the incidence of SDH almost doubles fromages 65 to 75, and continues toincrease in people over age 80. Theincidence of SDH is highest in thefifth through seventh decades of life.4The median age of patients withcSDH is 63, and 69% of them areover age 65. The incidence of cSDHis expected to increase as the population continues to age.4 (See cSDH: Anexpanding threat to older adults.)Several causes and predisposingfactors are associated with cSDH.These include cerebral atrophy,older age, male gender, head trauma,Chronicsubdural hematoma:A common complexityBy Vincent M. Vacca, Jr., MSN, RN, CCRN, SCRN, ENLS, and Isabel Argento, BSN, RN, CCRNMay l Nursing2018 l 25www.Nursing2018.comCopyright 2018 Wolters Kluwer Health, Inc. All rights reserved.
exposure to certain medications,alcohol use, and seizure activity(see Risk factors for cSDH).Similar to an acute SDH, whichis typically caused by trauma, cSDHis often associated with head injury.Falls are the most common cause ofall traumatic brain injuries, includingSDH. The incidence of falls peaks inboth males and females between ages75 and 79.5The incidence of mild head trauma has been reported in up to 80%of patients with cSDH, althoughmany have little or no memory of theinciting event.5,6 Approximately 38%of patients with a cSDH have a his-tory of only minor head trauma orcan’t recall any prior head trauma.7Regardless of whether they’re awareof a discrete traumatic event, mostpatients with cSDH experienced amild trauma without loss of consciousness, suggesting that they mayalso have an intrinsic susceptibilityto developing SDH.6,7Systemic effects of anticoagulationand antiplatelet therapy are wellknown risk factors for cSDH.Approximately 75% of primaryspontaneous or nontraumatic casesof cSDH are diagnosed in patientstaking these medications. In population studies, patients on oral antico-cSDH: An expanding threat to older adultsAccording to the CDC, the population of the United States in 2010 included 40 million people age 65 and over.27,28 The older population is projected to increase to 72million by 2030, representing nearly 20% of the total U.S. population. The oldestold population, defined as those age 85 and over, grew from just over 100,000 in1900 to 5.5 million in 2010. The U.S. Census Bureau projects that the populationage 85 and over could grow to 19 million by 2050.28As the population ages, the incidence of cSDH is expected to increase accordingly. Current trends in aging predict that once 20% to 25% of the population isover age 65, cSDHwill surpass priSubdural hematomamary and metaDura materstatic brain tumorsto become theArachnoidmost commonneurosurgical condition. This is projected to occur inthe United Statesby 2030.5,7Source: Pillitteri A. Maternal and Child Nursing.4th ed. Philadelphia, PA:Lippincott, Williams &Wilkins; 2003.agulation therapy are estimated tohave a 4- to 15-fold increased riskfor cSDH.8An SDH in the setting of anticoagulation can expand rapidly.Unless anticoagulation is quicklyreversed, the expanding SDH canresult in severe signs and symptomsand/or death.6,8PathophysiologySlow bleeding from the low-pressurevenous system into the subduralspace is the pathophysiologic mechanism leading to cSDH. A cSDH typically develops over 2 to 3 weeks toseveral months following an incitingevent.3,4,9The relatively slow rate of bleeding enables a large collection ofblood, blood degradation products,cerebrospinal fluid (CSF), and fluiddrawn by osmosis from surroundingtissues to accumulate in the subdural space before clinical signs andsymptoms appear. Over time, acSDH may further enlarge due tocontinued or recurrent venousbleeding, leading to serious complications such as increased intracranial pressure (ICP).3,4,9Like other masses that enlargewithin the rigid nonexpandableskull, an SDH may become lethal byincreasing ICP. Compression of braintissue results in cerebral ischemia,stroke, brain tissue shift, and brainherniation. Two common typesof brain herniation associatedwith SDH are subfalcine (cingulategyrus) herniation and transtentorial(uncal) herniation.10 (See Herniationsyndromes.)Clinical manifestationsThe presentation of cSDH can occasionally mimic stroke or rapidly progressive dementia.3,4 Many patientswith cSDH present with multiplesigns and symptoms, includingheadache (progressing in severity),gait disturbance, paresis, and acuteconfusion. Presentation can also26 l Nursing2018 l Volume 48, Number 5Copyright 2018 Wolters Kluwer Health, Inc. All rights reserved.www.Nursing2018.com
include neurologic focal signs,aphasia, seizures, and significantalteration in level of consciousness,including coma.3,4,11,12 Patientswith cSDH are at risk for additionalintracerebral hemorrhage, seizureactivity, and exacerbation of existingcomorbidities, especially when thecSDH is associated with anticoagulant therapy.7,11-14 Up to 20% havepoor neurologic outcomes resultingin permanent and significant disability.13DiagnosisNoncontrast brain computed tomography (CT) is the initial imaging studyof choice. Because a cSDH developsover 2 to 3 weeks or longer, cSDHsappear as isodense or hypodense(lighter) crescent-shaped lesions thatdeform the brain’s surface on CTscan.15 (See SDH on CT scan.)Over time, a cSDH will developencapsulating vascular membranes.Risk factors for cSDH11Pharmaceutical agents vitamin K antagonists, such aswarfarin novel oral anticoagulants, such asdabigatran antiplatelet medications, such asaspirin sympathomimetics, such as pseudoephedrineMechanism of injury syncope falls motor vehicle crashesUnderlying pathology cerebral atrophy cerebral vascular disease hypertension atherosclerosis malignancyPredisposing conditions older age CSF shunt seizure activity lumbar puncture alcohol use.Recurrent bleeding from small,friable vessels within these vascularmembranes accounts for the expansion of some cSDHs, causing them topersist and enlarge over time.4,6,11Magnetic resonance imagingdoesn’t routinely have a role indiagnosis of cSDH, but it may beperformed when SDH is suspectedbut not demonstrated on CT scan.4,15Initial managementBecause many older adults withcSDH also have chronic and oftencomplex comorbidities, management requires collaboration amongneurologists, neurosurgeons, neuroscience nurses, rehabilitation specialists, and others such as a socialworker and case manager, basedon the patient’s clinical status.3,11As with any emergency situation,immediate interventions are initiatedto support the ABCs—airway,breathing, and circulation—optimizeBP and hemodynamics, and normalize coagulation status.4 Correction ofexisting coagulopathy is crucial toreduce the risk of continued or recurrent bleeding.6Besides immediate discontinuationof all anticoagulant and antiplatelettherapy, a specific anticoagulantreversal strategy will be initiatedaccording to the specific agent’smechanism of action.14 Interventions may include infusion of prothrombin complex concentrate(PCC), fresh frozen plasma (FFP)or vitamin K.Reversal of newer novel oralanticoagulants (NOACs) is necessaryonly in cases of life-threateningbleeding or emergency surgery.14,16For patients taking any NOAC inthe absence of life-threatening acutehematoma expansion, surgery shouldbe delayed until 24 hours after thelast dose if possible. This delayshould be extended to 48 hours ifthe patient also has renal impairment.17 The dabigatran-specifichumanized monoclonal antibodyHerniationsyndromes291234Herniation of the cingulate gyrus underthe falx cerebri [1], central or transtentorial herniation [2], uncal herniationof the temporal lobe into the tentorialnotch [3], and infratentorial herniationof the cerebellar tonsils [4].Source: Porth CM. Essentials of Pathophysiology. 4thed. Philadelphia, PA: Wolters Kluwer Health; 2014.fragment idarucizumab was recentlyapproved for dabigatran-treated patients when reversal of anticoagulanteffects is needed for emergencysurgery or urgent procedures, or incases of life-threatening or uncontrolled bleeding.16,18For patients taking antiplateletmedications such as aspirin orclopidogrel, evidence is availableto support a treatment delay of 7 to10 days if possible to allow for theproduction of fully functional platelets. If treatment can’t be delayed,the American Society of Hematologyguidelines recommend preoperativeplatelet transfusion.6 Other sourcesof coagulation and platelet dysfunction that might exist in patients withSDH should be treated in consultation with hematologists. Surgicalintervention may or may not beindicated and is determined on acase-by-case basis.6,7,11Surgical options for cSDHThe general consensus is that patients with signs and symptoms thatcan be attributed to radiologicallyconfirmed cSDH should be treatedMay l Nursing2018 l 27www.Nursing2018.comCopyright 2018 Wolters Kluwer Health, Inc. All rights reserved.
surgically.11 While some reportsdescribe successful nonsurgicalmanagement of cSDH, experts generally agree that most patients witha cSDH require surgical drainagebecause the hematoma’s very existence suggests the failure or inability of physiologic mechanisms tonaturally reabsorb it. Although nospecific guidelines currently existon the indications for surgery incSDH, all symptomatic individualsshould be considered potential surgical candidates.6Surgical evacuation is recommended in cases of any SDH confirmed by radiologic imaging withmaximal thickness of greater thanor equal to 1 cm, or greater than orequal to 0.5 cm of brain tissue midline shift. For an SDH not meetingthose criteria, prompt surgicalevacuation may be indicated if thepatient has a Glasgow Coma Scale(GCS) score of 8 or less (severebrain injury) and meets one ofthe following criteria: a decrease in GCS score by 2 ormore points from the time of injuryto hospital presentationSDH on CT scan3Head CT reveals crescentic hyperdenselesions (see arrows) with edema/masseffect.Source: Hickey JV. Clinical Practice of Neurological& Neurosurgical Nursing. 7th ed. Philadelphia, PA:Wolters Kluwer Health; 2013. asymmetric or fixed and dilatedpupils ICP greater than 20 mm Hg(normal, 0 to 15 mm Hg).6,11See Glasgow Coma Scale (GCS)scoring for details about GCS scoring.ICP monitoring is indicatedfollowing successful emergent resuscitation and stabilization for patientswith a traumatic brain injury, including SDH, who have a GCS score from3 to 8 and an abnormal CT scan thatreveals hematomas, contusions,swelling, herniation, or compressedbasal cisterns.19 Increased ICP associated with reduced cerebral bloodflow causes hypoperfusion of braintissue, resulting in potentially lethalcerebral infarctions or strokes.4Once ICP monitoring is in place,treatment goals are to maintain ICPbelow 20 mm Hg and cerebral perfusion pressure between 50 and 70mm Hg to achieve and sustain adequate cerebral perfusion andoxygenation.1,20Surgical techniquesSurgery to treat a symptomaticcSDH can result in both rapid improvement of signs and symptomsand a favorable outcome in over80% of patients.4,21 Coupled withrelatively low surgical risk, surgicalevacuation is currently the mainstayof management for symptomaticpatients.11 However, the optimalmethod of cSDH surgical management remains an area of continuedresearch.6 The three primary surgical techniques are: twist drill craniostomy (TDC) involving small openings ( 10 mm)using a handheld twist drill. burr hole craniostomy (BHC)involving openings of 10 to 30 mm. open craniotomy (OC) involvinglarger openings.The TDC technique involves thecreation of a small craniostomy using ahandheld drill and closed systemdrainage. The advantage of thistechnique is that it can be performedGlasgow Coma Scale(GCS) scoringEye openingSpontaneousTo verbal stimuliTo painNo response4321Verbal responseOrientedConfused but can answerquestionsInappropriate wordsIncomprehensible speechNo responseMotor responseObeys commandsPurposeful movement to painWithdraws from painFlexion (decorticate posturing)to painExtension (decerebrate posturing)to painNo response54321654321Severe head injury----GCS score of 8 or lessModerate head injury----GCS score of 9 to 12Mild head injury----GCS score of 13 to 15Source: Centers for Disease Control and s/gcs.pdf.under local anesthesia at the bedside,making it an attractive option foran older adult with multiple comorbidities.11BHC involves creation of two burrholes, usually drilled about 5 to 8 cmapart on the same side as the cSDH.This is done under general anesthesia. The cSDH is irrigated with salineuntil the effluent runs clear, and asoft silicone drain is inserted into thesubdural space and connected to apassive closed drainage system that’sremoved after approximately 48hours.11OC, which also requires generalanesthesia, involves creation of alarger ( 30 mm) free bone flap toallow direct irrigation and evacuation of the hematoma. Followingirrigation and evacuation thebone flap is replaced and secured.6,11 If significant cerebraledema is associated with OC for28 l Nursing2018 l Volume 48, Number 5Copyright 2018 Wolters Kluwer Health, Inc. All rights reserved.www.Nursing2018.com
cSDH management, the dural membrane can be left open or replacedwith duraplasty, and the bone flapcan be left off to allow for cerebralexpansion. Known as a decompressive hemicraniectomy, this is doneto control ICP, improve cerebralcompliance, and maximize cerebralperfusion.22Post-op complicationsBetween 11% and 19% of patientsdevelop seizures following surgeryto manage cSDH, but the use ofantiepileptic drugs (AEDs) for seizure prophylaxis in cSDH patientsremains controversial.6 Preoperative AED prophylaxis has beenshown to lower the postoperativeseizure rate but not to affect longterm development of posttraumaticepilepsy. The use of prophylacticAEDs in patients without a historyof seizure isn’t currently recommended.11,23Surgical complications can include focal brain injury, stroke, newacute subdural or intracranial hemorrhage, seizures, surgical site infection, subdural empyema, andpneumocephalus. Besides these,possible post-op complications include those related to general anesthesia, recurrent or residual hematoma, intracranial hypertension,wound infection, CSF leak, meningitis, cerebral abscess, residual neurologic deficits such as speech disturbances or motor deficit, boweland bladder sphincter dysfunction,and behavioral changes. Severalstudies have shown a significantrelationship between patient ageand postoperative complications,meaning that complications increase with older age.24Although surgical outcomes inpatients with cSDH are generallyfavorable, perioperative mortalityranges from 1.2% to 11%. Oneyear mortality in patients withcSDH can be as high as 32%, depending on such factors as comor-curring within the first year after theprimary event.25The cumulative riskfor recurrence of anSDH is approximately15%, usually withinthe first year after theprimary event.bidities and GCS score.11 Datasuggest that an admission GCSscore of 9 or above in patientswho undergo surgical treatmentfor cSDH is associated with goodoutcome at 6 months postoperatively. However, a recurrence within the same period is associatedwith poor outcomes.11,12Recurrence of SDH is a significantconcern, with rates from 3.8% to30% being reported.6 Predictive factors for recurrence include malegender, older age, hypertension, alcohol use, diabetes, cirrhosis, renalinsufficiency, coagulopathy, and surgical treatment of the primary SDH.Exposure to medications includingstatins and anticoagulation and antiplatelet therapy also increase therisk of SDH recurrence. The cumulative risk for recurrence of an SDHis approximately 15%, usually oc-Medical managementSome patients with mild signs andsymptoms and/or small hematomasmay be treated medically. This approach includes observation andcontinued assessments and management of complications such as cerebral edema. Because of the knowninflammatory nature of cSDH, steroids may be useful as adjunctivetherapy as an alternative to surgicalintervention, but their role remainsill-defined.6,7,11The decision on whether to manage cSDH surgically or nonsurgically is largely based on expertopinion, with only sparse evidenceavailable to guide decisions. In alarge, heterogeneous population ofpatients with nonsurgically managed cSDH, one study found thatapproximately one out of everyeight patients was readmitted withnew or worsening cSDH within 90days. Approximately half of thesereadmissions resulted in surgicalhematoma evacuation, and about 1in 20 readmissions resulted indeath. The risk of these outcomeswas significantly higher after nontraumatic compared with traumaticcSDH because nontraumatic cSDHsare associated with older age andmore comorbidities.6,26Nontraumatic cSDHs presentin those who may be less able totolerate the presence of an undrained cSDH and would benefitfrom surgical management. Current recommendations for surgicalversus nonsurgical managementare based on clinical symptomatology and radiographic size of thelesion. However, inclusion of thecSDH etiology as a factor whendeciding surgical versus nonsurgical management of cSDH can bebeneficial. Conclusions from onestudy suggest that in the context ofcurrent practice, patients withMay l Nursing2018 l 29www.Nursing2018.comCopyright 2018 Wolters Kluwer Health, Inc. All rights reserved.
nontraumatic cSDH have worseoutcomes when managed nonsurgically than do patients with traumatic cSDH.6,26Nursing considerationsWhen caring for patients withcSDH, the nurse must understandthe risks of neurologic deterioration,such as SDH expansion or recurrence. This can result spontaneouslyor from factors such as uncontrolledhypertension, coughing, vomiting,or falls. Nursing care for these patients must be comprehensive because they’re at risk for many complications including alteration insleep-wake cycles, malnutrition,pain, confusion, delirium, falls,pressure injuries, dysphagia, impaired or loss of airway protectivereflexes, infection, stroke, and venous thromboembolism.Nurses must be prepared toperform admission and serial standardized neurologic assessments,including: mental status cranial nerve function motor system sensory system deep tendon, abdominal, and plantar reflexes.Nurses must also maintain theintegrity and accuracy of the ICPmonitoring system and reportpressure elevations beyond established parameters.1 These ongoingassessments are essential to bothestablish a baseline and to enabledetection of changes that may represent neurologic deterioration.Because these changes may signal animpending neurologic catastrophe,they must be reported immediately,thoroughly investigated, and treatedpromptly. The neurologic assessmentshould include evaluation for a newheadache or increased severity of anexisting headache; dizziness; changes in level of consciousness or memory; and impaired ability to understand, speak clearly, and followcommands. The nurse should bevigilant for evidence of seizures inthis population. Maintain seizureprecautions, monitor serum levels ofAEDs if prescribed, and be preparedto respond immediately should aseizure occur.3In collaboration with the healthcare provider, the nurse shouldmaintain euvolemia by administeringisotonic I.V. fluids to support cerebral perfusion without exacerbatingcerebral edema. Avoid administeringhypotonic I.V. fluids because theyincrease brain edema.Keep the patient’s head and neckaligned and free of constriction fromdevices such as cervical collars. Elevatethe head of bed to approximately45 degrees unless contraindicated.These strategies promote venousreturn from the brain, help controlICP, and facilitate reabsorption ofthe cSDH.The nurse must assess the patientfor the presence of pain using a standard validated pain intensity ratingscale. The healthcare provider, pharmacist, and nurse collaborate on apain management strategy with thegoal of managing pain without excessive sedation, which could make theneurologic assessment difficult toperform and interpret.For postoperative patients witha subdural drain, the nurse mustassess the site for signs and symptoms of leaking or infection, ensurethe patency of the drainage system,and monitor the dressing. Thenurse must also secure and protectthe drain from accidental dislodgement or removal, monitor theamount and characteristics of drainage, and report any abnormalitiessuch as failure to drain or excessivedrainage.Patient and family educationshould include an explanation of theneurologic assessment and the treatment plan, and address questionsand expectations of the patient andfamily.24It takes teamworkcSDH is a common neurologicdisorder in older adults, and itsincidence is rising due to an agingpopulation and increasing use ofanticoagulant and antiplatelet medications. Patients with cSDH areincreasingly being managed bymultidisciplinary teams, includingneurologists, neurosurgeons, neuroscience nurses, pharmacists, therapists, and rehabilitation specialists.All team members must be familiarwith the presentation, diagnosis, andmanagement of all types of SDH.More research is required to refinethe management of cSDH, includingexploration of minimally invasivetechniques and adjuvant treatmentsthat might reduce both recurrenceand the need for surgery.11,12 REFERENCES1. Bader MK, Littlejohns LR, Olson DM, eds.AANN Core Curriculum for Neuroscience Nursing.6th ed. Chicago, IL: American Association ofNeuroscience Nurses; 2016.2. McBride W. Subdural hematoma in adults:prognosis and management. UpToDate. 2017.www.uptodate.com.3. Hickey JV. The Clinical Practice of Neurologicaland Neurosurgical Nursing. 7th ed. Philadelphia, PA:Wolters Kluwer/Lippincott Williams & Wilkins;2009.4. Meagher RJ. Subdural hematoma. Medscape. 7overview.5. Tabuchi S, Kadowaki M. Chronic subduralhematoma in patients over 90 years old in a superaged society. J Clin Med Res. 2014;6(5):379-383.6. Huang KT, Bi WL, Abd-El-Barr M, et al. Theneurocritical and neurosurgical care of subduralhematomas. Neurocrit Care. 2016;24(2):294-307.7. Balser D, Rodgers SD, Johnson B, Shi C, Tabak E,Samadani U. Evolving management of symptomaticchronic subdural hematoma: experience of a singleinstitution and review of the literature. Neurol Res.2013;35(3):233-242.8. Guha D, Coyne S, Macdonald RL. Timing of theresumption of antithrombotic agents followingsurgical evacuation of chronic subdural hematomas:a retrospective cohort study. J Neurosurg. 2016;124(3):750-759.9. Iliescu IA. Current diagnosis and treatment ofchronic subdural haematomas. J Med Life. 2015;8(3):278-284.10. Ryan CG, Thompson RE, Temkin NR, Crane PK,Ellenbogen RG, Elmore JG. Acute traumatic subduralhematoma: current mortality and functional outcomesin adult patients at a Level I trauma center. J TraumaAcute Care Surg. 2012;73(5):1348-1354.11. Kolias AG, Chari A, Santarius T, Hutchinson PJ.Chronic subdural haematoma: modern management30 l Nursing2018 l Volume 48, Number 5Copyright 2018 Wolters Kluwer Health, Inc. All rights reserved.www.Nursing2018.com
and emerging therapies. Nat Rev Neurol. 2014;10(10):570-578.12. de Araújo Silva DO, Matis GK, Costa LF, et al.Chronic subdural hematomas and the elderly: surgicalresults from a series of 125 cases: old “horses” are notto be shot! Surg Neurol Int. 2012;3:150.13. Connolly BJ, Pearce LA, Hart RG. VitaminK antagonists and risk of subdural hematoma:meta-analysis of randomized clinical trials. Stroke.2014;45(6):1672-1678.14. Lucke-Wold BP, Turner RC, Josiah D, KnottsC, Bhatia S. Do age and anticoagulants affect thenatural history of acute subdural hematomas? ArchEmerg Med Crit Care. 2016;1(2):1010.15. McBride W. Subdural hematoma in adults:etiology, clinical features, and diagnosis. UpToDate.2015. www.uptodate.com.16. Brown KS, Zahir H, Grosso MA, Lanz HJ,Mercuri MF, Levy JH. Nonvitamin K antagonist oralanticoagulant activity: challenges in measurementand reversal. Crit Care. 2016;20(1):273.17. Hemphill JC 3rd, Greenberg SM, Anderson CS,et al. Guidelines for the management of spontaneousintracerebral hemorrhage: a guideline for healthcareprofessionals from the American Heart Association/American Stroke Association. Stroke. 2015. . Chesnut RM, Temkin N, Carney N, et al.A trial of intracranial-pressure monitoring intraumatic brain injury. N Engl J Med. 2012;367(26):2471-2481.28. Ortman JM, Velkoff VA, Hogan H. An agingnation: the older population in the United States.Population estimates and projections. United StatesCensus Bureau. 2014.21. Englehard HH III. Subdural hematoma surgery.Medscape. 2015. view.29. Porth CM. Essentials of Pathophysiology. 4thed. Philadelphia, PA: Wolters Kluwer/LippincottWilliams & Wilkins;2015.22. Crudele A, Shah SO, Bar B. Decompressivehemicraniectomy in acute neurological diseases.J Intensive Care Med. 2016;31(9):587-596.RESOURCES23. Emich S, Richling B, McCoy MR, et al. Theefficacy of dexamethasone on reduction in thereoperation rate of chronic subdural hematoma—the DRESH study: straightforward study protocolfor a randomized controlled trial. Trials. 2014;15(6):1-10.24. Ghanem HM, El-khayat RAE-A. Chronicsubdural hematoma: effect of developing andimplementing postoperative nursing carestandards on nurses performance for reductionor prevention postoperative complications. J AmSci. 2012;8(2):686-697.25. Schmidt L, Gørtz S, Wohlfahrt J, Melbye M,Munch TN. Recurrence of subdural haematoma ina population-based cohort—risks and predictivefactors. PLoS One. 2015;10(10):e0140450.18. Praxbind (idarucizumab) injection, forintravenous use. Prescribing information.www.praxbind.com.26. Morris NA, Merkler AE, Parker WE, et al.Adverse outcomes after initial non-surgicalmanagement of subdural hematoma: a populationbased study. Neurocrit Care. 2016;24(2):226-232.19. Carney N, Totten AM, O’Reilly C. Guidelines forthe management of severe traumatic brain injury,fourth edition. Neurosurgery. 2017;80(1):6-15.27. National Center for Health Statistics.Older Americans: Key Indicators of Well-Being.www.agingstats.gov. Akwaa F, Spyropoulos AC. Treatment of bleedingcomplications when using oral anticoagulants forprevention of strokes. Curr Treat Options CardiovascMed. 2013;15(3):288-298.De Bonis P, Trevisi G, de Waure C, et al.Antiplatelet/anticoagulant agents and chronicsubdural hematoma in the elderly. PLoS One.2013;8(7):e68732.McClelland S, Mackey SJ, Kim SS. The dangerousgamble of heparinization within two weeks ofnonoperative traumatic acute subdural hematomain patients with increased stroke risk: a case series.J Postgrad Med. 2014;60(2):194-197.Ross AG. Prudent care of head trauma in theelderly: a case report. J Med Case Rep. 2014;8:448.Vincent M. Vacca, Jr., is adjunct faculty at Massachusetts College of Pharmacy and Health Sciences University in Boston, Mass., and Isabel Argento is a nursein the Burn/Trauma/Surgical Intensive Care Unit atBrigham and Women’s Hospital, also in Boston.The authors and planners have disclosed no potentialconflicts of interest, financial or For more than 97 additional continuing education articles related toneurological topics, go to NursingCenter.com/CE Earn CE credit online:Go to www.nursingcenter.com/CE/nursing and receivea certificate within minutes.INSTRUCTIONSChronic subdural hematoma: A common complexityTEST INSTRUCTIONS To take the test online, go to our secure website atwww.nursingcenter.com/ce/nursing. View instructions fortaking the test online there. If you prefer to submit your test by mail, record your answers in thetest answer section of the CE enrollment form on page 32. You maymake copies of the form. Each question has only one correct answer.There is no minimum passing score required.DISCOUNTS and CUSTOMER SERVICE Send two or more tests in any nursing journal published byLippincott Williams & Wilkins together by mail, and deduct 0.95 from the price ofeach test. We also offer CE accounts for hospitals and other healthcare facilities onnursingcenter.com. Call 1-800-787-8985 for details.PROVIDER ACCREDITATIONLippincott Professional Development will award 1.0 contact hour for this Complete the registration information and course evaluation. Mailcontinuing nursing education activity.the completed form and registration fee of 12.95 to: LippincottLippincott Professional Development is accredited as a provider of continuingProfessional Development, 74 Brick Blvd., Bldg. 4, Suite 206,nursing education by the American Nurses Credentialing Center’s Commission onBrick, NJ 08723. We will mail your certificate in 4 to 6 weeks. ForAccreditation.faster service, include a fax number and we will fax your certificateLippincott Professional Development is also an approved provider ofwithin 2 business days of receiving your enrollment fo
basal cisterns.19 Increased ICP asso-ciated with reduced cerebral blood flow causes hypoperfusion of brain tissue, resulting in potentially lethal cerebral infarctions or strokes.4 Once ICP monitoring is in place, treatment goals are to maintain ICP below 20 mm Hg and cerebral per-fusion pressure between 50 and 70 mm Hg to achieve and sustain ad-