Transcription
In collaboration withMcGill UniversityShaping the Future of theInternet of Bodies: Newchallenges of technologygovernanceBRIEFING PAPERJ U LY 2 0 2 0
Cover: Unsplash/UmbertoContents3Foreword4Executive summary61 Part One: The internet of bodies is here71.1 Range and categories of technologies81.2 Data-enabled social benefits10131.3 Risks associated with the internet of bodies2 Part Two: Governance of internet of bodies data142.1 Data regulatory landscape in the US and EU182.2 New governance challenges in the age of big data212.3 Envisioning possibilities and options23Contributors25Endnotes 2020 World Economic Forum. All rightsreserved. No part of this publication maybe reproduced or transmitted in any formor by any means, including photocopyingand recording, or by any informationstorage and retrieval system.Shaping the Future of the Internet of Bodies2
July 2020Shaping the Future of the Internet of Bodies:New challenges of technology governanceForewordAs new technologies integrate with thehuman body, the opportunities– and risks – abound.Xiao LiuMcGill University Faculty Fellowat the World Economic ForumCentre for the Fourth IndustrialRevolution; Wilson China FellowIn the wake of the COVID-19 pandemic, wearabletechnologies such as health and location trackershave been thrust into the public spotlight – spurringnot only excitement about their potential benefitsbut also debate over their potential risks. Couldthese devices help public health authorities betterpredict, manage and avert future outbreaks?How might employers use data from wearabledevices to safely reopen businesses? What arethe implications for privacy and equity? How mightthis data be abused or used for other intendedpurposes such as public surveillance?These questions are at the heart of new effortsby the World Economic Forum, in collaborationwith public health authorities, leading technologycompanies and other stakeholders, to developand pilot new approaches for the ethical treatmentand sharing of health data collected by consumerwearable devices.1This paper aims to take these efforts one stepfurther, looking beyond the scope of wearableJeff MerrittHead of Internet of Things,Robotics and Smart Cities,Member of ExecutiveCommittee, World EconomicForumdevices at the broader ecosystem of connectedtechnologies that is coming together to create“the internet of bodies” (IoB). As with any area ofemerging technology, the IoB is evolving rapidly andits future is unknown. It is for exactly this reasonthat careful attention and thought – not simply onthe part of business but from government, civilsociety and the public at large – is required.We stand at the beginning of an important publicdialogue that will have major implications for publichealth, safety and the global economy and may alsoultimately challenge how we think about our bodiesand what it means to be human.This paper does not claim to provide acomprehensive view of all of the many facets of theIoB. However, it provides a glimpse of the myriad ofcomplex issues that can arise when the cyber andphysical worlds come together. We invite you to joinus in this important work to shape the development,use and impact of these technologies for the benefitof all society.Shaping the Future of the Internet of Bodies3
Executive summaryTo realize the full potential of the internetof bodies, we need robust, up-to-dategovernance frameworks.Shaping the Future of the Internet of Bodies4
The internetof things (IoT)is increasinglyentangling withhuman bodies.The internet of things (IoT) is increasingly entanglingwith human bodies. This emergence and fastexpansion of the “internet of bodies” (IoB)2 – thenetwork of human bodies and data throughconnected sensors – while offering enormous socialand health benefits, also raises new challenges oftechnology governance.With an unprecedented number of sensorsattached to, implanted within or ingested intohuman bodies to monitor, analyse and evenmodify human bodies and behaviour, immediateactions are needed to address the ethical and legalconsiderations that come with the IoB. The urgencyof such actions is further brought to the forefrontby the global COVID-19 pandemic, with extensiveIoB technologies and data being enlisted for thesurveillance and tracking of coronavirus.This white paper comprises two parts. Part oneprovides a landscape review of IoB technologies,as well as their benefits and risks. An examinationof the ecosystem shows that IoB technologiesare deployed not only in medical scenarios butalso across different sectors, from fitness andhealth management to employment settings andentertainment. The accelerating convergence ofconsumer devices and health/medical devices alsoshows that the line between medical and nonmedical IoB devices is blurring. This suggests thatnew strategies of governance are needed for IoBdevices, which are traditionally subject to differentregulatory agencies and rules.It is worth noting that this white paper will not delveinto gaming and virtual reality (VR) devices nor thedata from them. While related, these devices raisedistinct issues from the more traditional health andfitness devices.Part two examines the governance of IoB data –focusing, in particular, on the regulatory landscape inthe United States, with a comparative perspective ofregulation in the European Union. This part examinescurrent regulatory approaches to IoB data, as wellas the challenges raised by the rapidly shiftingecosystem, especially the wide adoption of big dataalgorithms. Whereas IoB technologies also entail otherissues such as the physical effects of devices on usersand liability for physical harms, this paper focusesonly on the governance of data generated from IoB,particularly from health and wellness IoB devices.Two main findings for policy-makers andstakeholders are highlighted. First, broad adoptionof the IoB and frequent flows of IoB data acrossscenarios and sectors requires robust and consistentgovernance frameworks in both the medical andnon-medical sectors. This is particularly the casefor IoB data governance as, while clinically deriveddata is in general strictly regulated, the regulationof consumer-generated data and other non-clinicaldata is often, given the sensitivity of the data, unevenin terms of coverage and strength across sectorsand jurisdictions; this is the case in, for example,the United States. Second, IoB data governanceapproaches and data protection laws need urgentupdates to address the risk of privacy, unfairnessand discrimination brought about by commonpractices of big data analytics. This risk presented bybig data analytics exists with both medical data andnon-medical data, as even deidentified medical datacan be reidentified or misused in a way that causesharm and discrimination to individuals and groups.We therefore urge stakeholders from acrosssectors, industries and geographies to worktogether to mitigate the risks in order to fullyunleash the potential of the IoB.Shaping the Future of the Internet of Bodies5
1Part One: The internetof bodies is hereRecent advancements in the internet ofthings are transforming the human bodyinto a new technology platform.Shaping the Future of the Internet of Bodies6
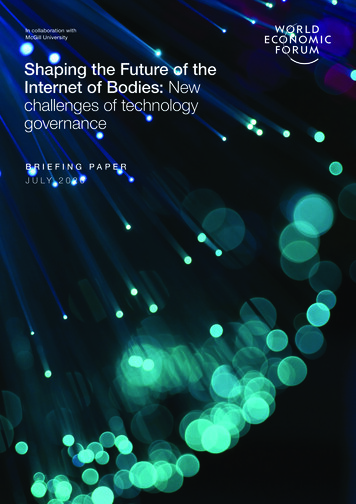
1.1 Range and categories of technologiesRecent technological advancements have usheredin a new era of the “internet of bodies” (IoB),3 withan unprecedented number of connected devicesand sensors being affixed to or even implanted andingested into the human body. This has turned thehuman body into a technology platform.4 The IoBgenerates tremendous amounts of biometric andhuman behavioural data. This is, in turn, fuellingthe transformation of health research and industry,as well as other aspects of social life, such as theadoption of IoB in work settings, or the provision ofnew options for entertainment – all with remarkabledata-driven innovations and social benefits. Yet theIoB also raises new challenges for data governancethat concern not only individual privacy andautonomy but also new risks of discrimination andbias in employment, education, finance, access tohealth insurance and other important areas for thedistribution of social resources.Generally, IoB technologies include medical devices,5a variety of lifestyle and fitness tracking devices,As reflected in Figure 1, IoB technologies can becharacterized as non-invasive or less-invasive, inthe sense that they are not expected to interferewith the structure or any function of the body; oras invasive, with sensors going under the skin tobe implanted into or become part of the body.Examples of internet of bodies technologiesntable (invasive)ImplaImplanted chips tospeed up access tohome, office and otherdevicesActivity trackers,smartwatches,smart garments,brainwearneurotechnology,augumented realitywearables, other bodyproximity consumerproductsMedicalNon-medicalDigital pills, artificialpancreas and organs,smart prostheses, brainimplant devicesWeaHearing or eyesightaid/augumentingdevices, continuousvitals (e.g. glucose)monitoring system,wearable peritonealdialysis devicese)FIGURE 1other smart consumer devices that stay in proximityto the human body and an expanding range of bodyattached or embedded devices that are deployed inenterprise, educational and recreational scenarios. Itis worth noting that the IoB technologies examinedhere are mostly “personal devices”, in the sensethat the devices always develop a relatively stablerelationship with the individual body of the user overa regular, extended period of contact. This, therefore,excludes the type of biometric technologies that areinstalled in public and private spaces, such as facialrecognition systems, fingerprint sensors and retinalscanners, which focus on collecting and processingthe data of a large population or group rather thanparticular individuals.rab leandbodyp r o x i m it y t e c h n o l o g i eos (nn-insvaivShaping the Future of the Internet of Bodies7
Invasive technologies include, for example,digital pills – a recent drug-device combinationdeveloped to deliver encapsulated medicine andmonitor medication adherence – which rely oningestible mini-sensors to be activated in thepatient’s stomach, and which then transmit datato sensors, the patient’s smartphone and otherdata portals. Other examples of smart medicalimplantables include: an internet-connectedartificial pancreas as an automated insulin deliverysystem for diabetes patients; and robotic limbs formovement rehabilitation in people with physicalmobility limitations. In recent years, increasingnumbers of people have chosen to implant chipsunder their skin, not for medical purposes but asa personal choice to speed up their daily routinesand for convenience – accessing their homes,offices or other devices just by swiping theirhands, for example.6 As part of biohacking culture,people have also sought to enhance their bodieswith implanted technology, from magnets andRFID chip implants to miniature hard drives andwireless routers.7Among less invasive technologies, some devicesremain on the surface of the human body – theseare usually called wearables. Wearable technologiesare a fast expanding area, with a 15.74 billionmarket in 2015, estimated to grow to 51.60billion by 2022.8 Electronic skin patches alone,which are widely adopted in medical wearables forcardiovascular monitoring, diabetes management,temperature, sweat and motion sensing and othertypes of biomarker monitoring, achieved morethan 7.5 billion in revenue in 2018.9 Non-medicalwearables are a dynamic field, with products andadoptions ranging from personal fitness trackersand smartwatches to enterprise applications.These include connected glasses and helmets inemployment settings for location tracking, safetymonitoring and job performance improvement;neurotechnological devices for work/learningproductivity; and augmented and VR devicesfor entertainment and education. In addition toimplantable and wearable technologies, smartsensors are increasingly appearing in ordinaryconsumer products such as combs, razors,toothbrushes, skin products, mattresses andothers. Although they do not stay affixed to thehuman body at all times, these products remain inproximity to the body and collect users’ biologicaland behavioural data on a regular basis.Currently, medical and non-medical IoB devices areoften subject to oversight by different governancebodies and separate sets of legal regulationsand rules. In the United States, for example, thepre-market approval and post-market oversightof medical devices fall under the domain of theFood and Drug Administration (FDA), while nonmedical devices in the consumer domain aremainly overseen by the Federal Trade Commission.Yet, in terms of their use scenarios, the divisionbetween medical devices and non-medicalconsumer devices is becoming blurred. Consumerwearable manufacturers such as Apple and Fitbitlook to expand their products into certified healthmonitoring devices and tap into health insurers andenterprises as their customers, while traditionalmedical device companies are also buildingdevices for use outside medical facilities. IoBdevices are being increasingly adopted across thedivision of medical/non-medical categories. Smartexoskeletons, for example, are used in industrialsettings to augment human performance, but alsofor mobility assistance, rehabilitation and otherhealth purposes. A national survey conducted inthe United States by Valencell in 2018 revealed theaccelerating convergence of consumer wearablesand personal health/medical devices.10 This invitesa reconsideration of the line between medical andnon-medical in the governance of IoB technologies.1.2 Data-enabled social benefitsThe variety and vast amount of data collectedthrough IoB technologies is propellingtransformations in health research andindustry, especially with the development of thedirect‑to‑consumer digital health market. IoBtechnologies have also been adopted to enhancework safety in high-risk scenarios. Four of the morenotable social benefits are detailed below.1. Enabling remote patient tracking and reducing cross infectionThe continuous monitoring of body vital signs throughsensors allows healthcare providers to better trackthe condition of patients within and beyond medicalfacilities, from data regarding blood pressure, oxygenlevels, glucose levels and heart rate to the person’ssleep, steps and other health-related factors.Continuous monitoring is increasingly recognized asa helpful tool to address the healthcare needs of theworld’s ageing population and patients with a chronicdisease.11 Recently, remote monitoring has also beenused in the fight against the COVID-19 outbreak. Forexample, VivaLNK, a California-based connectedhealth start-up, has designed a multipatient remotemonitoring solution with Alibaba to safely monitorpatient temperature, electrocardiogram (ECG),heart rate, respiratory rate and motion, and reducethe chance of cross infection for the protection ofmedical workers.12Shaping the Future of the Internet of Bodies8
2. Improving patient engagement and promoting a healthy lifestyleIoB technologies facilitate the expansion ofhealthcare to actively engage patients beyondtraditional medicine architecture. A goodexample is a virtual rehab programme that KaiserPermanente started in Southern California in2019, in which health professionals remotelymonitored the exercise and medication-takinghabits of enrolled patients recovering fromcardiac events. Wearing smartwatches enablespatients to share their vital and activities datawith their care providers, who interact with themregularly. The enhanced relationship betweenpatients and care providers and the flexibility ofthe remote programme beyond traditional clinicsettings improved the completion rate of the rehabprogramme from less than 50% to 87%, effectivelylowering readmission rates, and also reducingmedical costs.133. Advancing preventive care and precision medicineThe data provided by IoB technology enablesphysicians to spot diseases early and offerpreventive measures. Also, the volume and variety ofdata may help advance precision medicine researchby linking individual lifestyle and environmental datawith genetic and biologic data, providing deeperinsights into the drivers and treatments of disease.Consumer wearables provide new types of dataand possibilities in scientific research and clinicaltrials. From 2012 to 2017, more than 500 publishedstudies explored the use of Fitbit devices, withresearch conducted across a variety of differentstudy populations and environments.14 New andcomplex data sources beyond traditional clinicsettings can also extend research from individualhealth to population health to understanding howhuman behaviour, characteristics of communities,living and environmental conditions, as well asinstitutions and policies, all contribute to the generalhealth of a social group. This can potentially helpalleviate existing and potential equity issues inmarginalized groups’ access to health resources.4. Enhancing workplace safetyBeyond health applications, IoB technologies arealso being adopted in hazardous workplaces suchas construction sites, mines and factories to trackworker location, oversee environmental risks,reduce exposure to musculoskeletal injuries or otherharms, and mitigate risks by issuing informationremotely.15 High-quality real-time sensor dataprovides guidance to workers under complicatedand fast-shifting conditions, and improves safetymonitoring. Advancements in neurotechnology havealso delivered brainwear devices that can measureairline pilots’ and drivers’ alertness to improve travelsafety. Biometric sensors, from caps and vests towristbands and eyewear, are becoming lighter andcheaper, and can measure drivers’ fatigue levelsand alert them to pull off the road when drowsy.16Shaping the Future of the Internet of Bodies9
1.3 Risks associated with the internet of bodiesAlong with the social benefits and innovationsenabled by data from the IoB come new risksassociated with the misuse of data that containsintimate details of personal health and behaviours.Admittedly, IoB technologies share many concernswith the internet of things, such as consumer trust,safety, security and interoperability. Several aspectsof particular concern are detailed below.1. Interoperability and data accuracyIssues of standardization of data and interoperabilityof technologies present important obstacles incombining and benefitting from different types ofdata from varied sources to improve medical careand advance research. With millions of devicesin the health ecosystem deployed to monitor thehuman body, from the hospital bed to anywherethe IoB devices go with the body to which they areattached, the dominance of proprietary and closedcommunication methods results in vendor lock-inand a lack of interoperability between these devicesat the platform and technical level. The lack of astandardized platform to pull continuous streams ofdata from different devices constrains the use of thatdata to deliver valuable insights unless all data sourcesare inherently from interoperable devices. Increasingly,we are seeing interoperability between wearables andconsumer platforms, but this is more difficult to ensurewhen it comes to combining that data with data frommedical records, for example. The Health InsurancePortability and Accountability Act (HIPAA) in the USsupports portability of health information such asmedical records, but because wearables collect datathat is not under the remit of HIPAA, there is no onuson the manufacturers of wearables to ensure that levelof interoperability of system or portability of data.Besides interoperability, data accuracy is a concern,especially with consumer fitness devices. Currently,medical devices and non-medical devices aresubject to different regulatory and pre-marketapproval standards. However, as consumer trackingdevices are becoming integrated in healthcare– for example, to monitor heart rate and energyexpenditure in patients with cardiovascular disease– the issue of whether their measurements reacha level of clinically acceptable accuracy needsassessment and discretion.17 The replacement ofmedical-grade devices with consumer devices mayrun the risk of misdiagnosis such as false alarms andovertreatment.18 We see consumers increasinglyrelying on wearables to self-assess their own healthbased on data from wearables, without FDA ormedical oversight, and as such without guidance.2. Cybersecurity and privacyThere is increasing awareness of the vulnerabilityof wearables and medical IoT devices to hackingand cyberattacks, which expose human lives topotential physical harm and privacy risks. Globally,healthcare cybersecurity breaches in 2018accounted for 25% of 750 reported incidents, morethan any other industry.19 The issue is no less gravefor consumer devices. Researchers have foundserious security flaws with children’s smartwatches,which hackers can use to track children, gainaccess to audio, and make phone calls to them.20Privacy is one major factor affecting consumers’ trustand adoption of IoB devices. Increasing adoptionof IoB devices beyond traditional medical facilitiesalso raises new concerns about security andprivacy, while technical standards and policies areyet to reflect these new challenges. For example,an interactive map showing the whereabouts ofpeople who use wearable fitness devices revealedinformation about the locations and activities ofsoldiers at US military bases. Taken as an aggregate,this is highly sensitive information because itdescribes military movements even though personalidentifier information is removed from the publisheddata.21 At a consumer level, geolocation data derivedfrom a wearable can point to commuting patterns orother information that could be misused in the wronghands. Amid the global outbreak of COVID-19, withthe enlisting of data for coronavirus tracking and therelaxation of enforcement regarding health data in theUS and other countries, the privacy of health datahas generated serious concerns. The (im)balancebetween data privacy and the transparency requiredto tackle a public health emergency continues tobe a contentious topic. For example, the use ofsmart thermometer data for health surveillance andto create a “US health weather map” has raisedalarming privacy concerns. Some thermometercompanies are using this personal information tomarket and sell the data to third-party companies.22To address these issues regarding wearablesin order to standardize the approach taken bymanufacturers globally, the Institute of Electricaland Electronics Engineers (IEEE) and its StandardsAssociation have been working with the FDA,National Institutes of Health, and universities andindustry since 2016. Through the initiatives, theIEEE and its community has established TIPPSS(trust, identity, privacy, protection, safety andsecurity) as the principles to ensure patient safety.23Shaping the Future of the Internet of Bodies10
3. Risks of discrimination and fairness in data analyticsEmergent practices in relation to the handling ofdata derived from IoB devices signal potentialalarming discriminations and bias againstindividuals. When this user-generated, biologicallyderived data is combined with data from myriadother sources, such as retail stores, consumerproduct and service companies, finance servicesand government institutions for data analytics,abuse can occur. Algorithmic analytics can beused to make important decisions in areas suchas insurance, employment, finance, education,criminal justice, social services and the allocationof other types of social resources, all based ondata derived from IoB devices. Profiling andgrouping based on inaccurate or incomplete data,proxy data and the generation of sensitive datafrom inferences can result in biased policies anddecision-making that affect not only individualsbut also groups and vulnerable populations, eventhough data processors and decision-makerssometimes may not realize the implicit bias orpotential harm. Several examples of areas inwhich this discrimination and bias may be seenare noted below.–Discriminatory insurance policies: The useof IoB data with minute details of individualhealth conditions and life habits in insurancecould fragment the solidarity foundation ofinsurance and shake its socioeconomic andethical basics. Some insurers have already duginto vast amounts of personal data, rangingfrom home addresses and ownership, andeducation levels, to lifestyle data such asdietary habits, daily activities and exercises.The information is fed into computer algorithmsto assign each individual a risk score fordecisions regarding healthcare insurance, butalso in other types of insurance, such as lifeinsurance, disability insurance and even in areasnot directly related to health, such as financialloans.24 The data from IoB technologies oftenincludes fine-grained details of personal lifeas well as physical and mental health. Themisuse of this data could lead to discriminativeinsurance policies and prices, making it harderfor marginalized populations to access basichealthcare, and other types of insurance.–Discrimination and bias in employment:The adoption of wearables and IoB devicesin employee wellness programmes and inemployment scenarios creates new concernsabout employee privacy and workplacesurveillance. With employers using devices andalgorithms to monitor and direct employees’movements, communication and behaviourpatterns, relatively weak regulations in thisarea offer limited legal protection. This canexpose workers to higher risks of misuse ofdata and black-box algorithms that may leadto biased decisions regarding hiring, promotionand retention.25 For example, hiring algorithmsand predictive technologies are found toreplicate institutional and historical biases,but such biases are less easy to detect dueto the lack of transparency of the algorithmsand the sources and quality of data usedfor such algorithm training.26 The increasedrisks of privacy intrusion and unfairness havealready generated opposition from employees,unions and activists.27 In 2018, West Virginiateachers went on strike to demand the removalof a workplace wellness programme that wascriticized for penalizing members for not scoring“acceptable” levels on biometric measures.28Workers at UPS, McDonald’s and Amazonwarehouses have also protested against theexacerbated work stress and precarity imposedby management through intensive datacollecting trackers, and requested new rulesregarding employers who use tracking data todiscipline employees.29–Public policy that creates and/or reinforcessocial inequality: Policy-makers areincreasingly using new data sources anddata analytics for decision-making in publicpolicy such as health, disaster response,urban design, national security, economicdevelopment and other areas. Potential biasin the types and quality of data and algorithmsmay intentionally or unintentionally createand reinforce social inequality, limiting accessfor certain social groups to health and otherpublic resources. New sources of data frommobile phones and IoB devices, for example,have been adopted to track and predictthe outbreak and transmission of diseases.Yet, when deployed without attention to thepotential biases of data and algorithms, thereis a risk that data may remove an epidemicfrom its political and societal context, and,in particular, affect the lives of vulnerablepopulations. In the case of the 2014 Ebolaoutbreak, for example, many humanitarianorganizations active in Africa encouragedgovernments, charitable foundations,technology companies and mobile networks toshare data. But studies show that they lackedthe data-modelling capabilities, professionaltechnology implementation standards andenforcement capacity to define or protect thepublic interest, which resulted in the violationof basic human rights and aggravated theinequality gap in terms of accessing disasterassistance resources. 30The adoption of data analytics in decision-makinginvolves unprecedented volume, velocity andvariety of data, among which the data from IoBtechnologies is combined with those from othersources for cross-reference purposes. Thissuggests that the collection and use of IoB dataoften goes beyond the health sector; and on theother hand, data that is not directly health-related,Shaping the Future of the Internet of Bodies11
such as social media data, can also be used togenerate analytics relating to individual and grouphealth. These emergent practices and potentialrisks raise new challenges in governing the datagenerated by the expanding range of IoB networks.It is already difficult to guard data rights and ensuretransparency and fairness in the age of big data,and the specific challenges that IoB technologiescreate in this space mean that they need to beconsidered as part of that debate.As will be discussed in the following section, whileclinically based data is, in general, subject to strictregulation, the governance of data from healthbased lifestyle and other non-medical devicesis more uneven due to the divergence in dataregulations across sectors and under differentjurisdictions. It is suggested that laws governingthe collection of medical data are largely insufficientto address the security, privacy and discriminationrisks arising from the processing of IoB data.Shaping the Future of the Internet of Bodies12
2Part Two: Governanceof internet of bodiesdataCurrent regulations address some but notall of the many risks introduced by IoB data.Shaping the Future of the Internet of Bodies13
While the manufacturing and security of IoB devicesmay be subject to different government agenciesand related rules (such as Federal CommunicationCommission [FCC] regulations and guidelines formanufacturing IoT devices in the United States),the focus here is on the collection, transfer and useof IoB data, particularly the risks of discrimination
1 Part One: The internet of bodies is here 1.1 Range and categories of technologies 1.2 Data-enabled social benefits 1.3 Risks associated with the internet of bodies 2 Part Two: Governance of internet of bodies data 2.1 Data regulatory landscape in the US and EU 2.2 New governance challenges in the age of big data 2.3 Envisioning possibilities .