Transcription
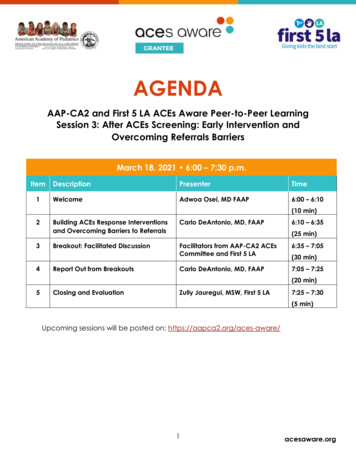
AGENDAAAP-CA2 and First 5 LA ACEs Aware Peer-to-Peer LearningSession 3: After ACEs Screening: Early Intervention andOvercoming Referrals BarriersMarch 18, 2021 6:00 – 7:30 p.m.Item1DescriptionPresenterTimeWelcomeAdwoa Osei, MD FAAP6:00 – 6:10(10 min)234Building ACEs Response Interventionsand Overcoming Barriers to ReferralsCarlo DeAntonio, MD, FAAPBreakout: Facilitated DiscussionFacilitators from AAP-CA2 ACEsCommittee and First 5 LA6:35 – 7:05Carlo DeAntonio, MD, FAAP7:05 – 7:25Report Out from Breakouts6:10 – 6:35(25 min)(30 min)(20 min)5Closing and EvaluationZully Jauregui, MSW, First 5 LA7:25 – 7:30(5 min)Upcoming sessions will be posted on: https://aapca2.org/aces-aware/1
BIOGRAPHYCarlo DeAntonio, MD, FAAPDr. Carlo DeAntonio is a pediatrician and the Director of Clinical Services at the NorthLos Angeles County Regional Center.He earned his Bachelor of Arts at Harvard University and his Medical Doctorate atUniversity of California, Los Angeles (UCLA). He completed his residency in pediatricsat Mattel Children’s Hospital at UCLA.Dr. DeAntonio is a past Fellow of the California Health Care Foundation (CHCF) HealthCare Leadership Program. Areas of interest include developmental disabilities, earlyintervention, and child advocacy.2
American Academy of Pediatrics – Chapter 2 (AAP-CA2)and First 5 LA present:ACEs AwarePeer-to-Peer Learning SeriesA Provider Engagement ActivityMarch 18, 2021
AgendaDescriptionPresenterTime1WelcomeAdwoa Osei, MD FAAP6:00 – 6:10 (10 min)2Building ACEs ResponseInterventions and OvercomingBarriers to ReferralsCarlo De Antonio, MD, FAAP6:10 – 6:35 (25 min)3Breakout: Facilitated Discussion4Report Out from BreakoutsCarlo De Antonio, MD, FAAP7:05 – 7:25 (20 min)5Closing and EvaluationZully Jauregui, MSW, First 5 LA7:25 – 7:30 (5 min)Facilitators from AAP-CA2 ACEs6:35 – 7:05 (30 min)Committee and First 5 LA
Zoom EtiquettePlease MUTE yourself upon entering the Zoom call;Unmute yourself before you speak(press *6 to unmute yourself and *9 to raise hand via phone)Add your organization to your name;Hover over your name in the Participant box to “Rename”Feel free to use the chat box throughout the meetingJoin us by video if you can!If you have any technical difficulties, feel free to private chat the Host, Tomas Torices
After ACEs Screening: EarlyIntervention and OvercomingReferral BarriersCarlo De Antonio MD, FAAPNorth LA County Regional CenterMarch 18, 2021
Learning Objectives:By the end of this session, learners will be able to o Describe AAP Guidelines for Developmental screeningo Understand the relationship between ACEs screening and developmental screeningo Understand Early Intervention as an effective strategy for addressing ACEs for childrenages 0-3o Understanding referral guidelines for CA Early Start and Regional Centero Understand impact of pandemic on screening and referralso Navigate common barriers to implementing screening and referrals in practice
Recap ofSession 1 &Session 2
Recap of Session 1 – January 7th with Christine Thang, MDACEs Study Conclusions from Dr. Anda:o ACEs are common.o The cumulative impact of multiple exposures can becaptured in an “ACE Score”.o The ACE Score likely captures the cumulative(neuro)developmental consequences of traumatic stress.o The ACE Score has a strong, graded relationship tonumerous health, social, and behavioral problemsthroughout a person's lifespan.1AndaR. The Health and Social Impact of Growing Up With Adverse Childhood Experiences The Human and Economic Costs of the Status Quo.
Recap of Session 2 – February 11 with Dr. Adam Schickedanz MDo Describe common barriers to identifying and addressingadverse childhood experienceso Examine health system barriers to identifying andaddressing adverse childhood experiences in theirown practices.o Assess readiness to deliver trauma-informed care inone’s practice1AndaR. The Health and Social Impact of Growing Up With Adverse Childhood Experiences The Human and Economic Costs of the Status Quo.
Adversity, Neuroendocrine Response, & Life Course Health Outcomes
THREADS: The ResiliencyFactors of ChildhoodResiliency skills as the THREADS ofchildhood:–––––––Thinking and learning brainHopeRegulation or self controlEfficacyAttachmentDevelopmental skill masterySocial connectedness
When the THREADS ofResilience are FRAYEDYou are FRAYED (and at the end of yourrope):––––––Fits, Frets and FearRestricted developmentAttachment concernsYelling and yawningEducational delaysDefeated/dissociation
Upstream Health Care & Life Course HealthRoot Causes of Poor Health Outcomes are Found UpstreamWhat Happens Here Impacts Health Here
ACEs Screeningo erse-childhoodexperiences/o Abuse : Physical, emotional and sexual abuseo Neglect: Physical and emotional neglecto Household Challenges: growing up in a household with incarceration, mentalillness, substance dependence, absence due to separation or divorce, orintimate partner violence
tified-English.pdf
ACEs Aware Screening & Response assessment-treatment-planning/
After ACEsScreening: EarlyIntervention andOvercomingReferral Barriers
ACEs and Developmental Delayo Developmental Delay associated with ACEso Both ACEs screening and Developmental screening areimportant components of Pediatric Well Child Careo Reimbursement for ACEs screening and Developmentalscreening
ated-Health-Conditions.pdf
ification-issue-brief-1 620.pdf
/californiadata.pdf
AAP Guidelines AAP Policy Statement: July 2006 American Academy of Pediatrics. Identifying Infants and YoungChildren with Developmental Disorders in the Medical Home:Algorithm for Developmental Surveillance and Screening.Pediatrics. 2006;118:405-420 Reaffirmed 2009 and 2014 AAP Policy Statement: November 2007 Johnson CP, Myers SM, American Academy of Pediatrics Councilon Children with Disabilities. Identification and Evaluation ofChildren with Autism Spectrum Disorders. Pediatrics 2007;120:11831215. Reaffirmed 2010 and 2014.
When to Screen?GeneralDevelopmentAutism9 months18months18months24months24 or 30months
Why Screen?
Common Screening Testso Global Developmental Screens– Ages and Stages Questionnaire (ASQ)– Parent’s Evaluation of Developmental Status (PEDS)o Condition Specific Screens– Autism: Modified Checklist for Autism in Toddlers – Revised (MCHAT-R/F)– ACES: PEARLSo Global Behavioral Screens– ASQ: SE-2 Ages & Stages Questionnaire – Social Emotional– Pediatric Symptom Checklist (PSC)
Summary Surveillance at every well-child check Add in ASD specific milestones and observations tosurveillance visits Screening Parental or provider concerns at any interval At intervals of 9, 18 and 24-30 months Autism specific screening @ 18 and 24 months Refer for Developmental Evaluation promptly Concerns from provider or discovered with screening
Early Intervention:California Early Start and RegionalCenter
Referral to Regional CenterResource for:Developmental EvaluationEarly Intervention Services (under 3)Diagnostic evaluation for ASD, Intellectual DisabilityLifelong services for individuals with diagnosed withhandicapping developmental disability
Regional Centers in California
Impact of Pandemic on ReferralsFewer Well Child VisitsFewer opportunities for Developmental Surveillance andScreeningSchool closuresFewer social opportunities for parernts and young childrenIncrease in stressDecline on EI referrals March-August 2020 (NLACRC data)Need to catch up on missed developmental screenings
Criteria for Regional Center Early StartEligibilityInfants up to 36 months who: Have been diagnosed with an Established Risk condition Are under 36 months of age with a 33% or greater Delayin one developmental domain Are High Risk of having a substantial developmentaldisability due to a combination of bio-medical risk factors
ACEs and Early Start EligibilityDevelopmental Delay :Cognitive, Motor, Language, Social-Emotional, AdaptiveHigh Risk Factors: Prenatal substance exposure, Bio-medical insult (including non-accidentaltrauma), failure to thrive, developmentally disabled parent.
Early Start- Assessment 45 day timeline from date of referral to eligibility determination Eligibility determined by parental history, review of medicalrecords, and by direct developmental assessment by qualifiedprovider
Early Start- Assessment Direct Assessment typically includes: Developmental evaluation with standardized tool (such as Bayley) assessing all 5 areas ofdevelopment (Cognitive, Motor, Language, Social/ Emotional, Adaptive). Additional Speech and Language evaluation or PT/ OT evaluation depending on clinicalsituation. Qualified providers used
Criteria for Regional Center Eligibility- Over 3Persons with a substantially handicappingdevelopmental disability
Criteria for Regional Center EligibilityDEVELOPMENTAL DISABILITY Intellectual Disability Cerebral Palsy Epilepsy Autism Spectrum Disorder Disabling conditions found to be closely related to intellectual disability or to requiretreatment similar to that required for individuals with intellectual disability
Eligibility Assessment Psychological evaluation Performed by Licensed Clinical Psychologist with training / experience in cognitive and ASDassessment Psychometric testing Adaptive testing Autism specific testing School observation Review of records (medical, school, prior testing)
Service Provision Once an applicant is found eligible for services an IPP or IFSP (EarlyStart) is developed Services are developed based on need Regional Center payor of last resort and cannot provide servicesprovided by other generic agencies
Examples of Services Early Start (under 3):– Infant development, advocacy, speech therapy PT, OT, BehavioralServices (ABA) Lanterman (over 3):– Advocacy, family support, residential, work training, day program,social/adaptive skills, behavioral.
OvercomingReferral Barriers
Common Barriers to ReferralFamily LevelPractice LevelResource LevelPandemic Challenges
Common Barriers to ReferralParent Hesitation or Resistance114Unsure Who Provides Services77Other38Limited Time37Unsure How to ReferLimited Staff3529*Los Angeles County Department of Public Health Survey, 2018
Issue Briefo Too many children under 5 years old withor at risk for developmental-behavioraldelays are not connected to earlyintervention services in California.– Fragmented services, complex eligibilityand unclear referral processes– Limited availability of early interventionservices– Unable to make timely referrals– Families have diverse perceptions andunderstanding about early ds/files/linkage-to-services-issue-brief-2 417.pdf
Strengthening Early Identification and Intervention for Children withMild to Moderate Developmental Delays 2019 Strategic ForumParticipants identified the following areas of focus:1.Multi-system communication, collaboration and coordination– Closing the feedback loop– Use technology and other innovative approaches– Normalize reaching out to other providers (Incentivize & Facilitate cross-system peersupport groups)2.Embedding a family centered approach– Draft “Bill of Rights” for families/caregivers– Prioritize family’s identified needs/priority as a starting point– Expand family sensitive approaches, resources
Questions?Email: cdeantonio@nlacrc.orgWant more info on AAP-CA & ACEs?Visit aapca2.org/aces/
Breakout Objectives Engage in solution-oriented discussions Share information and ideas that may be useful forpeers Share information and ideas to elevate to keydecision makers
Breakout: Solutions for Common Referral BarriersYou will be placed in a breakout that focuses on ONE of thesecategories: Family Level (no follow through with referral due to hesitation, stigma, other priorities,disagreement, etc.) Provider Level (hesitation/training, staff capacity, knowledge of resources) Resources (no feedback from referring party, information out of date, waiting lists) Pandemic Challenges (missing well child visits and thus screenings, added stress,misinformation about availability of referring parties)
Breakout Discussion Topics1. Propose solutions or examples of ways to overcomethese barriers.2. What are additional supports and resources that youwould need to make implement these solutions?
Report Out1. What solutions did your group propose?2. What resources would be needed to implementthese solutions?
Closing and Evaluation Thank you for your attendance andparticipation! Please complete the post-session surveyat http://tinyurl.com/PeerToPeerSession3(Required to receive CME credit).This link will also be emailed to you.
AAP-CA2 and First 5 LA Peer-to-Peer Learning Session SeriesSessionDateSession 1January 7, 2021TopicACEs Science – The Physiology of ToxicStressChildhood Adversity, Health SystemsChange, and the Future of TraumaInformed Pediatric PracticeSpeakerChristine Thang,MD, FAAPAdam Schickedanz, MD,PhD, FAAPSession 2February 11, 2021Session 3March 18, 2021After ACEs screening: Early Interventionand Overcoming Barriers to ReferralsCarlo DeAntonio,MD, FAAPApril 22, 2021Impact of Secondary Trauma andBurnout, with a Blueprint for WellnessNirupama Madduri,MD, FAAP, andAdwoa Osei, MD, FAAPSession 4Upcoming sessions posted here: https://aapca2.org/aces-aware/
Resources
Find your local Regional /listings/
Screening Resourceso ACEs Screening (PEARLS) https://www.acesaware.org/screen/o ASQ https://agesandstages.com/screening-navigator/o PEDS: https://www.pedstest.com/AboutOurTools/o MCHAT: https://m-chat.org/
Pediatric Medical Clinic Toolkito The toolkit offers:– Implementation Steps– Recommendations & Considerations– Lessons from the Field– Templates and Toolso Download at: comes-developmentalscreening-referral-toolkits/
ification-issuebrief-1 y-identification-issue-brief-1 620.pdf
Appendix
Referenceso Data Resource Center for Child & Adolescent Health. (2014). 4 essential facts aboutlifelong health, school success and adverse childhood experiences among California’schildren. Retrieved from /californiadata.pdfo Macrides, P., & Ryherd, S. (2011). Screening for developmental delay. American FamilyPhysician, 84(5), 544-549. Retrieved d67a79c3d34e28186d4e3022c387.pdfo Sullivan, P. A., & Knutson, J. F. (1998). The association between child maltreatment anddisabilities in a hospital-based epidemiology study. Child Abuse & Neglect, 22(4), 271288.
References American Academy of Pediatrics, Council on Children with Disabilities. Policy Statement:Identifying infants and young children with developmental disorders in the MedicalHome: An algorithm for developmental surveillance and screening. Pediatrics. 2006;118:405- 420. American Academy of Pediatrics, Is your One-Year-Old Communicating with you? ElkGrove Village, IL: American Academy of Pediatrics; 2004 (available at www.aap.org) California Department of Developmental Services. Autistic Spectrum Disorders: BestPractice for Screening Diagnosis and Assessment. 2002(available at www.dds.ca.gov)
References Filipeck, PA, et al. Practice parameter: Screening and diagnosis of autism. Neurology2000;55:468-479. Glascoe, FP. Early detection of developmental and behavioral problems. Pediatric. Rev.2000;21:272-278. Plauche-Johnson C, Meyers SM. Identification and evaluation of children with autisticspectrum disorders. Pediatrics. 2007;120:1183-1215
Overcoming Referrals Barriers March 18, 2021 6:00 - 7:30 p.m. Item Description Presenter Time 1 Welcome Adwoa Osei, MD FAAP 6:00 - 6:10 (10 min) 2 Building ACEs Response Interventions and Overcoming Barriers to Referrals Carlo DeAntonio, MD, FAAP (2 6:10 - 6:35 5 min) 3 Breakout: Facilitated Discussion Facilitators from AAP-CA2 ACEs