Transcription
PCFA INFORMATION GUIDEUNDERSTANDINGURINARY PROBLEMSFOLLOWINGPROSTATE CANCERTREATMENT
This book is for men who have made a decision to have a specifictreatment or have already received treatment for prostate cancer.It contains information about important issues to help men whoneed to know about treatment, urine symptom managementissues and incontinence.PCFA provides a range of resources to support men, partners andtheir families with prostate cancer. For further information, pleasesee www.pcfa.org.au.NOTE TO READERBecause what is known about prostate cancer and its treatmentis constantly changing and being updated, your treating healthprofessionals will give you information that is specific to your uniqueneeds and situation.If you would like further information please contact PCFA(telephone: (02) 9438 7000 or freecall 1800 220 099email: enquiries@pcfa.org.au website: www.pcfa.org.au).DISCLAIMERPCFA develops materials based on the best available evidence andadvice from recognised experts; however, it cannot guarantee andassumes no legal responsibility for the currency or completeness of theinformation.ACKNOWLEDGEMENTSThis resource was developed by a multidisciplinary Expert AdvisoryGroup.PCFA gratefully acknowledges the input, advice and guidance of themen with prostate cancer and health professionals who helped in thedevelopment of this booklet by offering their time to review its content.— Associate Professor Nick Brook (Urologist)— Professor Suzanne Chambers (Psychologist)— Associate Professor Pauline Chiarelli (Physiotherapist)— Associate Professor Eric Chung (Urologist)— Mr Nigel Cook (Consumer)— Professor Jon Emery (Primary care physician)— Ms Susan Hanson (Cancer Australia)— Dr Amy Hayden (Radiation Oncologist)— Mr Ian Henderson (Prostate Cancer Specialist Nurse)— Ms Sharron Hickey (Clinical Nurse)— Associate Professor Michael Izard (Radiation Oncologist)— Associate Professor Michael Jefford (Medical Oncologist)— Ms Jocelyn Klug (Sexual Rehabilitation Specialist)PERIODIC UPDATES— Associate Professor Anthony Lowe (PCFA)It is planned that PCFA will review this booklet after a period of, but notexceeding, four years.— Dr David Malouf (Urologist) Prostate Cancer Foundation of Australia 2014This work is copyright. Apart from any use as permitted under theCopyright Act 1968 no part may be reproduced by any processwithout prior written permission from the Prostate Cancer Foundationof Australia. Requests and enquiries concerning reproduction andrights should be addressed to the Chief Executive Officer, ProstateCancer Foundation of Australia, PO Box 499, St Leonards, NSW 1590Australia. Website: www.pcfa.org.au Email: enquiries@pcfa.org.au— Professor Ian Olver (Cancer Council Australia)— Dr Vivienne Milch (Cancer Australia)— Ms Carolyn Russell (Radiation Oncology Nurse Specialist)— Mr David Sandoe OAM (PCFA)— Ms Jennifer Siemsen (Prostate Cancer Specialist Nurse)— Ms Sue Sinclair (Cancer Australia)— Mr Alex Sloss (Consumer)ISBN 978-0-9945028-2-7— Mr John Stubbs (CanSpeak)Supporting men with prostate cancer through evidence-basedresources and support is a Cancer Australia initiative, funded by theAustralian Government.— Ms Julie Sykes (PCFA)— Ms Kyla Tilbury (Urology Nurse)— Ms Glenice Wilson (Continence Advisor)— Dr Tim Wong (PCFA)— Associate Professor Henry Woo (Urologist)Editor:Ms Helen SignyMedical Illustration:Mr Marcus Cremonese
Contents1Introduction22Your prostate and bladder: the connection33How is urine function controlled?44What is urinary incontinence?55What causes urinary problems?56Common reactions to urinary side effects from treatment67Urinary side effects following treatment— Surgery— Radiotherapy68Where can I find help?99Looking after yourself1210 GlossaryWelcome. We hope youfind the following contentinformative and clear.14
UNDERSTANDING URINARY PROBLEMS FOLLOWINGPROSTATE CANCER TREATMENT1IntroductionThis book is for men who have made a decision to have a specifictreatment or have already received treatment for prostate cancer.It contains information to help you understand important issuesabout urinary problems following prostate cancer treatment. Itmay also be helpful for significant people in your life (e.g. yourpartner, family and friends) to read this booklet. Urinary problemsare common after treatment for prostate cancer. However,with the right advice (and understanding), side effects can bemanaged and in many cases, resolved.The cancer journey is your personal experience of cancer.It’s not the same for everybody, even with the same type ofcancer. Depending on your stage of prostate cancer and otherunderlying conditions, your experience may be quite different.As the diagram Your cancer journey shows, it can be usefulto think of the journey in stages that may include detection,diagnosis, treatment, follow-up care and survivorship. For some,it may include end of life care. Take each stage as it comes soyou can break down what feels like an overwhelming situationinto smaller, more manageable steps.Your cancer journeyAfter being diagnosed with prostate cancer, it’s common for youto see a number of health professionals with different expertisewho work together as a team, called a multidisciplinary team(also known as a healthcare team). Best practice treatmentand supportive care for people with cancer involves a teamof different health professionals. Each team member bringsdifferent skills that are important in managing care and in makingdecisions around your individual needs. The team includeshealth professionals who are involved in diagnosing your cancer,treating your cancer, managing symptoms and side effects andassisting you with your feelings or concerns during your cancerexperience.For some men, the impact of treatment may be minimal orquickly resolved. For others, this impact can be more difficult,requiring further support and help. The aim of this booklet is toprovide you with information that you can then use as a guideto further discussions with your doctor and healthcare teamabout your situation. Being informed enables you to participatein decisions about your care and leads to improved experiencesand better care.This booklet contains information on:—p ossible urinary side effects of some treatmentsfor prostate cancer—w hy urinary problems can occur following treatment— helpful strategies for managing these problems— people and resources that can help.YOUR CANCER JOURNEYMulti-disciplinary Care TeamSurvivorshipDetectionDiagnosisTreatmentand managingside effectsFollow-upcareEnd of life careSupportive Care2
UNDERSTANDING URINARY PROBLEMS FOLLOWINGPROSTATE CANCER TREATMENT2Your prostate and bladder:the connectionTo understand your urinary problems, it is important to knowhow the prostate and bladder are connected, and how yourprostate cancer treatment affects them both.BLADDER AND PROSTATEProstate glandSeminalvesicle— The prostate gland is normally the size of a walnut but mayenlarge as you age. It is located between the bladder and thepenis and sits in front of the rectum.Vas deferensUrinary bladder— The main function of the prostate gland is to produce fluidthat nourishes and protects sperm. During ejaculation, theprostate squeezes this fluid into the urethra (urine tube) andit is expelled with the sperm as semen.— The urethra is the thin tube that runs through the centre ofthe prostate from the bladder to the penis. It is the passageused for urine and semen.UrethraRectumAnusEjaculatoryductI needed more informationon dedicated physiotherapyinterventions to controlincontinence.3TesticleScrotumPenis
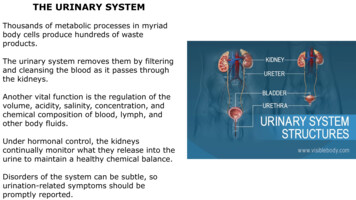
UNDERSTANDING URINARY PROBLEMS FOLLOWINGPROSTATE CANCER TREATMENT3How is urine function controlled?Urination is controlled by two urinary sphincters, which aremuscles acting like valves. The internal sphincter is locatedwhere the bladder and urethra join, called the bladder neck.The external sphincter sits below the prostate near the pelvicfloor.The pelvic floor muscles also play a part in bladder control.The floor of the pelvis is made up of muscle layers and tissues.The layers stretch like a hammock from the tailbone at the backto the pubic bone in front. Your pelvic floor muscles support yourbladder and bowel. The urethra (urine tube) and rectum (backpassage) pass through the pelvic floor muscles.These two sphincter muscles act together, and control urine byopening and closing around the bladder neck and urethra. Whenthey get permission from the brain, the sphincters relax to allowthe bladder to empty. At the same time, the bladder musclescontract and squeeze urine out of the bladder. When you havefinished urinating, the sphincter muscles contract and closewhile the bladder relaxes.INTERNAL AND EXTERNAL URINARY SPHINCTERSB) Emptying bladderA) Full bladderBladderProstaticurethraExternal sphincterInternalsphincterProstate4
UNDERSTANDING URINARY PROBLEMS FOLLOWINGPROSTATE CANCER TREATMENT45What is urinary incontinence?What causes urinary problems?Urinary incontinence is the accidental leaking of urine and apossible side effect in men who have had surgery or radiotherapyfor treating their prostate cancer. The amount of leakage can varyfrom a drop to total emptying of the bladder.Before your prostate cancer treatment, you may or may nothave experienced urinary problems. The main cause for urinaryproblems before treatment is an enlarged prostate causingobstruction (blockage) to the bladder. After treatment, if thereare urinary problems, they are usually related to the effects thattreatment has had on your urinary system, which are unwantedand can be unpleasant. These are known as urinary side effects.For example, surgery will physically change your urinary system,while radiotherapy can cause irritation, inflammation and swellingto the bladder, prostate, urethra and rectum (back passage).For some men, urinary problems may not occur or are quicklyresolved. For other men, they can be more problematic, requiringfurther support and help from members of their healthcareteam who specialise in prostate cancer and urinary problems.It is important to talk to your healthcare team about any urinaryproblems you are experiencing because they understand yourindividual situation, and are able to give you the most relevantadvice.Understanding urinary side effects can help you when you areseeking support and advice.There are different types of urinary incontinence.— Stress urinary incontinence is the loss or leaking of urine whenthere is an increase in abdominal pressure. For example, whenyou cough, laugh, sneeze, change position or are physicallyactive.— Urge urinary incontinence is the sudden intense need tourinate without the ability to delay, resulting in the loss orleaking of urine before you reach the toilet. Urgency or urgeincontinence occurs when your bladder is overactive orcontracting without you wanting it to.— Mixed incontinence is a combination of urinary problemsrelated to both stress and urge urinary incontinence.— Overflow incontinence is when your bladder never completelyempties, causing urine to leak. This can occur in men withprostate enlargement, scarring of the urethra caused bytreatment or at the neck of the bladder due to injury orinfection.It is important to talk toyour healthcare team aboutany urinary problems youare experiencing.5
UNDERSTANDING URINARY PROBLEMS FOLLOWINGPROSTATE CANCER TREATMENT67Common reactions to urinaryside effects from treatmentUrinary side effects followingtreatmentFor many men, coping with urinary side effects after prostatecancer treatment can be challenging. If you are experiencingurinary side effects, particularly incontinence, you may be feelingemotions such as embarrassment, anxiety, frustration and socialisolation. Fear of leakage can be enough to stop men from takingpart in their normal social activities.SURGERYWhen your prostate gland is removed entirely by surgery, aprocedure called radical prostatectomy (open, laparoscopicor robotic), two things occur during the surgery that can causeurinary side effects.—A gap is created between the bladder and urethra, which isthen surgically reconnected.If you have someone you trust (e.g. your partner, close friend),talking with them, and seeking help and advice from membersof your healthcare team can help you cope with possible urinaryside effects.— The bladder neck (where the bladder and urethra join) canbe affected and this can cause urinary problems. Also, theexternal sphincter may be weakened, or very rarely, damagedduring surgery, and this can cause urinary problems as well.This is why pelvic floor exercises before your surgery, andafter removal of your catheter, which can strengthen theexternal sphincter, can help with managing possible urinaryproblems after surgery. (Note: do not perform pelvic floorexercises while the catheter is in place, this allows the surgicalarea time to recover).Urinary side effects can be managed, and in many cases,resolved.Understanding urinaryside effects can help youwhen you are seekingsupport and advice.Some urinary side effects that you might experience followingsurgery include:— incontinence (accidental leaking of urine)— i ncomplete emptying (a feeling of not fully emptying yourbladder)—h esitancy (difficulty beginning your urinary stream)— i ntermittency (a stop/start urinary stream)— dribbling (slight urinary leakage after urinating is completed)—w eak urinary stream (slow flow with minimal force)— s training (having to push or strain to begin your urinary stream)— f requency (needing to urinate every two hours or less)—u rgency (strong sudden urge to urinate and inability to delay it)— nocturia (need to urinate overnight)—p ain (any discomfort, such as burning, stinging or pain whileurinating).Stress urinary incontinence is the most common urinary sideeffect following prostate cancer surgery.For some men, these side effects start improving soon after thecatheter is removed, while for others it can take 6 to 12 monthsafter surgery for normal bladder function to fully return andurinary side effects resolve. A small percentage of men willexperience permanent incontinence. There are treatment optionsavailable for permanent incontinence. Discuss your situation withyour healthcare team if it applies to you.6
UNDERSTANDING URINARY PROBLEMS FOLLOWINGPROSTATE CANCER TREATMENT7Urinary side effects followingtreatmentURINARY CATHETERA urinary catheter is a thin plastic tube that runs from yourbladder through your penis and drains urine into a bag on theoutside of your body. The catheter is held in place by an inflatedballoon inside your bladder. Generally a catheter is left in placefor 1 week following your surgery but this may vary based onyour individual situation.Many factors can affect continence following surgery such asyour weight, the stage of your cancer, the surgical techniquerequired for your individual situation, or if you were experiencingany urinary problems before your surgery. For older men (over70 years old), it may be slower initially for them to regain theircontinence, but there is some evidence that by 3-6 months, thereis no difference between younger and older men in terms of urinecontrol after surgery.RESOURCESPCFA has resources on side effects of treatments for prostatecancer. For further information, please see www.pcfa.org.au.Very rarely, the bladder neck (where the bladder joins theremainder of the urethra) can develop a narrowing known asbladder neck stenosis (or stricture).Problems caused by a stenosis may include:— a weak urinary stream— hesitancy— a feeling of incomplete emptying of your bladder— spraying of urine when urinating— urinary retention.BEFORE SURGERYSeminalvesiclesVasdeferensRectumTumourAFTER SURGERYBladderProstateUrethraSphincterPenis7
UNDERSTANDING URINARY PROBLEMS FOLLOWINGPROSTATE CANCER TREATMENT7Urinary side effects followingtreatment— urinary stricture (narrowing of the urethra due to scarringthat can cause side effects already mentioned).RADIOTHERAPYThere are two main types of radiotherapy – external beamradiotherapy (EBRT) and brachytherapy. The differenceis whether the treatment is applied from outside the body(EBRT) or delivered from within the prostate (brachytherapy).While urinary incontinence may occur after radiotherapy, thisside effect is less common than after surgery. Pelvic floorexercises can help. Talk to members of your healthcare teamfor information (e.g. Continence nurse).External beam radiotherapyExternal beam radiotherapy (EBRT) uses high energy X-raybeams that are directed at the prostate from the outside todestroy cancer cells.BrachytherapyBrachytherapy is when radioactive material is given directlyinto the prostate at either a low dose rate (LDR) or high doserate (HDR). LDR and HDR relate to the speed with which thedose is delivered, not the actual dose itself.Urinary side effects following EBRT can be described as‘early’ or ‘late’. Early side effects are those that occur duringor shortly after radiotherapy treatment, and usually settle afew weeks after treatment finishes. Late side effects are thosethat take months or years to develop, and can be permanent.These side effects can vary from mild to more severe formsand be age-related rather than due to the treatment. However,most men experience mild forms of these side effects andmany have none.— Low Dose Rate: It is given by implanting permanentradioactive seeds directly into the prostate. The seeds giveoff a focused amount of radiation to the prostate with theaim of destroying the cancer cells.— High Dose Rate: It is also given by inserting radioactivematerial directly into the prostate but, unlike LDR seeds,the placement of the material is temporary and for shorterperiods – usually for a day or two at a time.If you are already experiencing urinary problems beforestarting EBRT, these problems may get worse. Please talkto members of your healthcare team about concerns youhave about existing or possible urinary problems followingtreatment.Urinary side effects following brachytherapy may occur dueto the effect this treatment can have on surrounding areassuch as the bladder and urethra. Similar to EBRT, urinary sideeffects following brachytherapy can be described as ‘early’ or‘late’.Possible early urinary side effects of EBRT include:— urgency (strong sudden urge to urinate and inability todelay it)The early and late side effects of brachytherapy are the sameas those listed in the EBRT section.— frequency (needing to urinate everytwo hours or less)Most men will experience urinary side effects followingLDR. These may be minimal or mild, and usually peak atapproximately 6 to 8 weeks, after which side effects thengradually ease and resolve. A small percentage of men stillmay experience urinary side effects 6 months or longerfollowing implantation. For men who had HDR, urinary sideeffects usually peak between 1 to 3 weeks and improve atapproximately 4 to 6 weeks following treatment.— pain (any discomfort such as burning, stinging or pain whileurinating)— nocturia (need to urinate overnight)— intermittency (a stop/start urinary stream)— dribbling (slight urinary leakage after urinating iscompleted)A small number of men may experience urinary retention (theinability to urinate) due to the swelling of the prostate followingbrachytherapy. You may be given medication to assist withthis immediately following your treatment. The swelling cancause obstruction to your urinary flow from the bladder.Occasionally, a urinary catheter is required to continuouslydrain your bladder for a short period until the swellingresolves.— straining (having to push or strain to begin your urinarystream).Possible late urinary side effects of EBRT include:— weak urinary stream (slow flow with minimal force)— nocturia (need to urinate overnight)— urgency (strong sudden urge to urinate and inability todelay it)Blood in the urine can occur both immediately afterbrachytherapy or long term after all forms of radiotherapy.As a result of the brachytherapy procedure, some bleedingmay occur. This should settle within 24 to 48 hours after theprocedure. Blood in the urine that occurs more than 6 monthsafter all forms of radiotherapy could be a new problem as itmay not be related to the treatment, and should be discussedwith your healthcare team.— intermittency (a stop/start urinary stream)— dribbling (slight urinary leakage after urinating iscompleted)— straining (having to push or strain to begin your urinarystream)8
UNDERSTANDING URINARY PROBLEMS FOLLOWINGPROSTATE CANCER TREATMENT78Urinary side effects followingtreatmentWhere can I find help?As noted earlier, while uncommon, radiotherapy forprostate cancer may cause urinary stricture. Men who hadbrachytherapy (high dose rate) are at higher risk of a stricture.Problems caused by a stricture may include:It’s important for you to learn about the possible urinary sideeffects from prostate cancer treatment because occasionallythey may require urgent medical attention. Please talk tomembers of your healthcare team for more information.— a weak urinary streamPossible urinary side effects that require immediate attentioninclude:— hesitancy— spraying of urine when urinating—a urinary tract infection (symptoms include fever, pain,burning, stinging while urinating, pain into the kidney area,feeling unwell, smelly or cloudy urine)— urinary retention.—b lood in the urine— a feeling of incomplete emptying of your bladder— inability to urinate.Your general practitionerYour GP can help coordinate your care and provide you and yourfamily with support and information to help you make informedchoices about treatment. Your GP can help you and thoseclose to you manage your physical and emotional health needsthroughout the cancer journey, including help with managingyour urinary problems.There are a range of thingsyou can do to improve,and help you cope with,your urinary side effects.Your healthcare teamGenerally, there is a member of the healthcare team who will beyour main contact person. This person might change during yourcancer journey. If you’re unsure who this person is, ask one of thehealth professionals you’re seeing. Your contact person can talkwith other health professionals on your behalf and can make sureall your health care needs are met.The benefits to you in having a healthcare team include:— improved communication, coordination and decision makingbetween health professionals about your care— improved treatment planning because all treatment types andoptions are considered by a range of health professionals— i mproved coordination of services— improved delivery of services— improved quality of life.When working with your healthcare team, you may see thefollowing health professionals:— GP: Your first port of call who can provide referrals to otherspecialists and who will monitor your health— Urologist*: A specialist in treating diseases of the urinary tractsystem and male reproductive organs— Radiation Oncologist*: A specialist in the treatment of cancerusing radiation therapy— Medical Oncologist*: A specialist doctor who uses differentdrugs to treat cancer (such as chemotherapy)— Endocrinologist*: A doctor who specialises in hormones, bodychemistry and bone density* T hese health professionals also use hormone therapy, also known asandrogen deprivation therapy (ADT), as part of their treatment.9
UNDERSTANDING URINARY PROBLEMS FOLLOWINGPROSTATE CANCER TREATMENT8Where can I find help?— Pathologist: Conducts tests to assess the stage andaggressiveness of cancerHealth professionals who can help to manage urinaryproblems— Radiologist: A specialist doctor who examines scans, X-rayand other imaging results‘ I needed more information on dedicated physiotherapyinterventions to control incontinence.’— Nurse (also known as Urology or Prostate Care Nurse):Provides treatment, support and assistance through alltreatment stagesThere are specialist healthcare professionals who can assist withurinary problems you may be experiencing.It can be helpful for you to talk with your urologist about yoururinary side effects from prostate cancer treatment. Thereare medical treatments, including surgery, to help managecontinence (e.g. artificial urinary sphincters and male slingsurgery).— Cancer Nurse Coordinator: Guides you, your family and theperson you are caring for through cancer treatments andliaises with other care providers— Continence Nurse: Helps you manage any problems related tocontinence (urinary or bowel) care after treatmentContinence nurses and continence physiotherapists fromyour healthcare team can advise you on all matters to do withincontinence. Continence Nurse Advisors can be contactedthrough your healthcare team or Continence Foundation ofAustralia has listings of where to find your local advisor (www.continence.org.au).— Pharmacist: Dispenses medications and offers medicationadvice— Dietitian: Recommends the best eating plan while in treatmentand recovery— Physiotherapist: Specialises in movement and function of thebody, advises on resuming normal physical activitiesContinence Nurse Advisors can assist with:— Exercise Physiologist: Specialises in the benefits of exercisesto help people get fitter for overall health or help people with amedical condition through exercise— toileting practices during recovery from treatment— pelvic floor exercise education— continence product assistance for managing symptoms— Occupational Therapist: Helps with the physical side of dailylife by providing rehabilitation exercises— assistance and education with self-help techniques— financial assistance advice (you may qualify for local or federalfunding schemes)— Social Worker: Advises on support, practical and legalmatters, and provides strategies to cope with emotional,social and spiritual challenges— information and resources— homecare matters such as:— Psychologist, Psychiatrist or Counsellor: Provides strategieswith decision making, problem solving, and dealing withpsychosocial issues; including providing emotional andpractical support, and managing anxiety and depressiono w aste disposal, infection control measures such as use ofdisinfectant hand wash, bathing and hygiene in the homeo a dvice on fittings and fixtures commodes, rails to assistin toileting and arranging a home care assessment. If youare eligible you may receive assistance with the cost ofthese home alterations.— Palliative Care Specialist: Expert in pain and symptom controlwho works closely with the treatment team— Sex Therapist: Helps with sexuality issues by identifying thelevel of sexual functioning available, and enhancing sexual andrelationship functioningContinence Physiotherapists can assist with:— pelvic floor exercise education— Fertility Counsellor: Specialises in helping people with fertilityconcerns and issues, and can advise on fertility preservationoptions before starting treatments.— toileting practices during recovery from treatment, particularlycorrect posture— assistance and education with self-help techniques— development of individual pelvic floor and general exerciseprogrammes.10
UNDERSTANDING URINARY PROBLEMS FOLLOWINGPROSTATE CANCER TREATMENT8Where can I find help?It can be helpful for you totalk with your urologist aboutyour urinary side effects.?Questions you could ask Listed below are some questions you might want to askmembers of your healthcare team about urinary problemsfollowing prostate cancer treatment:— What can be done about my urinary problems?What would you recommend?— What are the alternatives to the approach that you’rerecommending?— What are things that I can do to improve urinaryproblems?— What are the lifestyle changes I need to make to improvemy urinary problems?— Are there food, drinks or activitiesI should avoid? What are they? How do they make myurinary problem worse?— If I chose medical treatment to manage my urinaryproblems, how quickly do they work? And are there anyside effects?— Who else could I see to help me with my urinaryproblems?These are not the only questions to ask. There might bequestions you have that are specific to your needs. Theimportant thing to do is to always ask questions that can helpyou understand what can be done about your urinary problemsso you, with support from your healthcare team, can make thebest decision for you.11
UNDERSTANDING URINARY PROBLEMS FOLLOWINGPROSTATE CANCER TREATMENT9Looking after yourselfThere are a range of things you can do to improve, and help youcope with, your urinary side effects. If you require assistance withany of these self-help measures, contact the health professionalsor organisations listed in this section.— Avoid drinks or food that cause bladder irritation: Caffeine(tea, coffee, cola drinks), alcohol, citrus juices, drinks withartificial sweeteners, citrus fruits, tomatoes and tomato-basedproducts, spicy or acidic foods can cause bladder irritation.Water is the most beneficial drink that you can have. You mayneed to plan when to drink your fluids, for example, by cuttingback fluids in the evening to prevent getting up at night.— Continence products: There are a range of continenceproducts to help manage urinary incontinence. Pads are aneffective first choice. Supermarkets and pharmacies stockranges specifically designed for men. Pads are to be wornwith firm-fitting underwear, not boxer shorts. Ensure youchange pads regularly, keeping your skin clean and dry toavoid irritation.— Lose weight if required: Excess body weight puts extrapressure on the bladder, which can increase urgency urinarysymptoms.— Diabetes: If you are diabetic, ensure your blood glucose levelsare regulated. Urinary issues can be affected by unstableblood glucose levels. ‘ There was a continence nurse who explained a lot of thethings that were supplied like the incontinence aids forthe five years since I’ve had the operation, I’ve had to findwhat suits me by experimenting with the products that wer
This book is for men who have made a decision to have a specific treatment or have already received treatment for prostate cancer. It contains information about important issues to help men who need to know about treatment, urine symptom management issues and incontinence. PCFA provides a range of resources to support men, partners and