Transcription
Advanced Infection Prevention andControl TrainingMay 2018 versionPrevention of catheter-associatedurinary tract infection (CAUTI): studenthandbookIntroductionWelcome to the “Prevention of catheter-associated urinary tract infections (CAUTI)”module. This advanced module is part of a broader infection prevention and control(IPC) training package targeting advanced IPC focal points working in low-resourcesettings. It is designed to support the implementation of the WHO Guidelines on corecomponents of infection prevention and control programmes at the national andacute health care facility level1 as part of a multifaceted approach to capacitybuilding.Target audienceThis training module is designed for individuals and teams who are intending tooccupy a senior leadership position in IPC at the national, subnational or healthfacility level. Trainees are expected to possess at least basic experience andcompetence in IPC. They could include IPC professionals, IPC hospital teams,facility administrators, hospital epidemiologists, microbiologists and other relevanthealth care professionals, among others. The package complements a basic trainingpackage intended for all front-line health care workers.Learning objectives of the moduleThe module aims to equip the advanced IPC focal point to: explain the problem of CAUTI; explain catheter use, occurrence of CAUTI and related risk factors; recognize CAUTI and understand management principles; explain evidence-based (multimodal) implementation strategies for CAUTIprevention including appropriate catheter insertion, maintenance and removal.Purpose and content of the student handbookThe module comprises a blend of PowerPoint presentations, videos and group work(including case studies and interactive question-and-answer sessions). The studenthandbook contains supplementary information to support learning, handouts that willbe referred to during the training, reflective reading for homework and group workinstructions. Together with the PowerPoint slides it will form a valuable resource forstudents.The table below sets out the module’s sessions and lists the associated resourcescontained within the handbook.1Guidelines on core components of infection prevention and control programmes at the national and acutehealth care facility level. Geneva: World Health Organization; 2016 ns/ipc-components-guidelines/en/, accessed 23 January 2018).1
Advanced Infection Prevention andControl TrainingMay 2018 versionSession1. The problem of CAUTIResource Handout 1. Key points to note Page3Handout 2. My 5 Moments for HandHygiene – Focus on caring for a patientwith a urinary catheterHandout 3. IFIC basic concepts ofinfection control, Chapter 18: Preventionof catheter-associated urinary tractinfections4 Handout 4. Quiz 1Handout 5. Supplementary informationrelated to quiz 11415 Handout 6. Guide for Foley catheter usein hospitalized medical patientsHandout 7. Types of catheterization andcatheters16 Handout 8. Common microorganismscausing CAUTI193. Recognizing CAUTI andunderstandingmanagement principles Handout 9. Collecting a catheterspecimen of urine from the sampling port204. Implementing evidencebased (multimodal,quality improvementinformed) strategies forCAUTI prevention duringcatheter insertion,maintenance and removal Handout 10. Four key IPC principles andpractices21 Handout 11. Multimodal strategy triggerquestionsHandout 12. Aseptic Non TouchTechnique (ANTT) posterHandout 13. Two case studies – Kenyaand United States of AmericaHandout 14. Additional reading list23 2. Catheter use, occurrenceof CAUTI and related riskfactors 6182527282
Advanced Infection Prevention andControl TrainingMay 2018 versionHandout 1. Key points to note Avoid urinary catheterization if possible! When feasible, use a two-person team to perform insertion. Use sterile equipment and aseptic technique during insertion andaftercare/maintenance. Review the need for the catheter daily and remove as soon as possible when nolonger needed (ideally within 48 hours). Hand hygiene is critical (especially moment 2 before an aseptic/clean procedureand moment 3 after blood and body fluid exposure). Don’t change the catheter routinely if it is functioning properly. Maintain closed drainage. Bladder irrigation/washout and use of antiseptics/antimicrobial agents does notprevent CAUTI: do not use! Empty drainage bag regularly into a clean receptacle used only on one patient. The clean receptacle should be changed daily.3
Advanced Infection Prevention and Control TrainingMay 2018 versionHandout 2. My 5 Moments for Hand Hygiene – Focus oncaring for a patient with a urinary catheterThe hand hygiene poster is available to download from: hygiene/workplace reminders/en/4
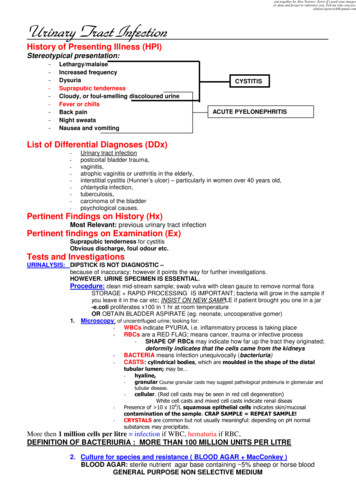
My 5 Moments for Hand HygieneFocus on caring for a patientwith a Urinary CatheterCLEAN YOUR HANDS WHEN HANDLING A URINARYCATHETER AND DRAINAGE SYSTEM3O4AFTERTOUCHINGA PATIENTDAFT E R BO UFLUOSRIS I D E X PKCLEAN YOUR HANDS WHEN HANDLING A URINARYCATHETER AND DRAINAGE SYSTEMImmediately after any task involving the urinary catheteror drainage system that could lead to urine exposure, such as:3a. Collecting a urine sample3b. Emptying the drainage bag3c. Removing the urinary catheterWHY?To protect the patient against harmful germs,including the patient's own, from entering his/her body.YEBEFORETOUCHINGA PATIENTWHY?R1BEFCL OREAPRE ASEPTIC/N E D U REC2Immediately before any manipulation of the urinary catheteror drainage system that could lead to contaminationof the sterile urine, such as:2a. Inserting or applying an indwelling, intermittent straight,or condom catheter; immediately before putting on sterile gloves2b. Accessing the drainage system to collect a urine sampleor to empty the drainage bag5AFTERTOUCHING PATIENTSURROUNDINGSTo protect yourself and the health-careenvironment from harmful patient germs.5 KEY ADDITIONAL CONSIDERATIONS FOR A PATIENT WITH A URINARY CATHETER Make sure that there is an appropriate indication for the indwelling urinary catheter.Use a closed urinary drainage system, and keep it closed.Insert the catheter aseptically using sterile gloves.Assess the patient at least daily to determine whether the catheter is still necessary.Patients with indwelling urinary catheters do not need antibiotics (including for asymptomatic bacteriuria),unless they have a documented infection.No Action TodayNo Cure TomorrowAll reasonable precautions have been taken by the World Health Organization to verify the information contained in this document. However, the published material is being distributed without warranty of any kind,either expressed or implied. The responsibility for the interpretation and use of the material lies with the reader. In no event shall the World Health Organization be liable for damages arising from its use.WHO acknowledges for their active participation in developing this material the VA Ann Arbor Healthcare System & University of Michigan’s Patient Safety Enhancement Program (www.catheterout.org),Ann Arbor, MI, United States, and Infection Control and Human Factors Laboratories, University Hospital Zurich, Zurich, Switzerland (www.humanlabz.org).
Advanced Infection Prevention and Control TrainingMay 2018 versionHandout 3. IFIC basic concepts of infection control, Chapter18: Prevention of catheter-associated urinary tract infectionsThe chapter is available to download from: TI 2016.pdf6
Prevention of Catheter-Associated Urinary Tract InfectionsChapter 18Prevention of CatheterAssociated Urinary TractInfectionsNizam DamaniKey PointsUrinary catheterisation should be avoided if possible. If needed, then catheter should be reviewedon a daily basis and removed as soon as clinically possible, preferably within 5 days.Urinary catheterisation should be performed using sterile equipment and aseptic technique shouldalways be maintained during insertion and aftercare procedures.Hands must be properly washed before and after procedure and during daily management.Catheters should not be changed routinely as this exposes the patient to increased risk of bladderand urethral trauma.Maintain a closed drainage system; open systems should be avoided if at all possible.Bladder irrigation or washout and instillation of antiseptics or antimicrobial agents does not prevent catheter-associated urinary tract infection and should not be used.The drainage bag should be emptied at least once per nursing session into a clean receptacleused only on one patient. International Federation of Infection Control1
IFIC Basic Concepts of Infection Control, 3rd edition, 2016Introduction1-4Urinary tract infections (UTI) are the commonest healthcare-associated infections (HAI), accountingfor up to 40% of all HAIs. Most involve urinary drainage devices, such as bladder catheters. The risk of a catheterised patient acquiring bacteriuria increases with the duration of catheterisation, the daily rate is 5% sothat by 4 weeks almost 100% of patients are bacteriuric. One to four percent of patients with bacteriuria willultimately develop clinically significant infection, e.g., cystitis, pyelonephritis, and septicaemia.Therefore, urinary catheters must only be inserted when there are clear medical indications ( SeeTable 18.1). They should be removed as soon as no longer needed. In suitable patients, clean intermittenturinary catheterisation or external condom catheters should be considered, as these have a lower risk ofinfection. Urinary incontinence is not an indication for urinary catheterisation; use napkins or absorbent padsinstead.Table 18.1. Indications for the use of indwelling urinary cathetersExamples of appropriate uses of indwelling cathetersPatient with acute and/or chronic urinary retention or bladder outlet obstructionMaintain a continuous outflow of urine for patients with voiding difficulties (as a result of neurological disorders that cause paralysis or loss of sensation affecting urination)Need for accurate measurements of urinary output in critically ill patientsPerioperative use for selected surgical procedures, e.g., patients undergoing urological surgery orother surgery on contiguous structures of the genitourinary tractAnticipated prolonged duration of surgery catheters inserted for this reason should be removedin theatre recovery unitPatients anticipated to receive large-volume infusions or diuretics during surgery or need for intraoperative monitoring of urinary outputTo assist in healing of open sacral or perineal wounds in selected incontinent patientsPatient requiring prolonged immobilisation, e.g., potentially unstable thoracic or lumbar spine ormultiple traumatic injuries such as pelvic fracturesTo improve comfort for end of life care if neededExamples of inappropriate usesDon’t use indwelling catheters as a substitute for nursing care of the patient or resident with incontinenceDon’t use as a means of obtaining urine for culture or other diagnostic tests when the patient canvoluntarily voidDon’t use for prolonged postoperative duration without appropriate indicationsPathogenesisUnder normal circumstances urethral flora, which tends to migrate into the bladder, is constantlyflushed out during urination. When a catheter is inserted, this flushing mechanism is circumvented and perineal and urethral flora can pass up into the bladder in the fluid layer between the outside of the catheter andthe urethral mucosa or in the urine in the catheter lumen (i.e., endogenous). Because of this, bladder colonisation is inevitable if catheters are left in place for prolonged periods.In addition, bladder infection can be caused by bacterial reflux from contaminated urine in thedrainage bag. Closed drainage systems reduce onset of infection by limiting access of bacteria to the urine.Hands of personnel may also contaminate the urinary catheter system during insertion or management (i.e.,exogenous). See Figure 18.1.MicrobiologyA UTI is usually caused by endogenous microorganisms from the patient's own bowel. In community-acquired infections, the commonest microorganisms are E. coli and Proteus spp. International Federation of Infection Control2
Prevention of Catheter-Associated Urinary Tract InfectionsFig 18.1. Main sites through which bacteria may reach the bladder of a patient with an indwelling urethralcatheter.Source: Maki DG, Tambyah PA. Emerg Infect Dis 2001;7:1-6.Healthcare-associated UTIs are more resistant to antibiotics. This is because hospitalised patients become colonised with resistant microorganisms, a process encouraged by an increased length of stay and exposure to antibiotics. In communities where indiscriminate antimicrobial use is common, multi-resistant Gramnegative bacteria (e.g., extended spectrum beta-lactamase producers [ESBL] and carbapenem-resistant Enterobacteriaceae [CRE]) are also common colonisers of the human bowel.E. coli is the most frequent cause of catheter-associated UTI (CAUTI). However, increasingly, CAUTIs arecaused by more resistant Gram-negative species, including Klebsiella and Pseudomonas, as well as resistant E.coli. Similarly, ampicillin-resistant Enterococcus and vancomycin-resistant E. faecium (VRE) are becoming common. With additional antibiotic exposure, infections occur with multiply drug resistant bacteria (e.g., ESBL,CRE, VRE).Resistant microorganisms may also be acquired by transfer from other patients, most commonly viacontaminated staff hands, but sometimes from environmental sources. Urine and urinary catheter systemsshould be carefully disposed of, bottles and jugs cleaned and disinfected, and hands properly washed and decontaminated during insertion and management.Definitions and SurveillanceSurveillance of CAUTI can be performed in selected groups of patients, e.g., patients in intensive careunits or specific types of surgical patients. A definition for CAUT
Urinary tract infecons (UTI) are the commonest healthcare-associated infecons (HAI), accounng for up to 40% of all HAIs. Most involve urinary drainage devices, such as bladder catheters. The risk of a cath-eterised pa ent acquiring bacteriuria increases with the dura on of catheterisa on, the daily rate is 5% soFile Size: 3MBPage Count: 28