Transcription
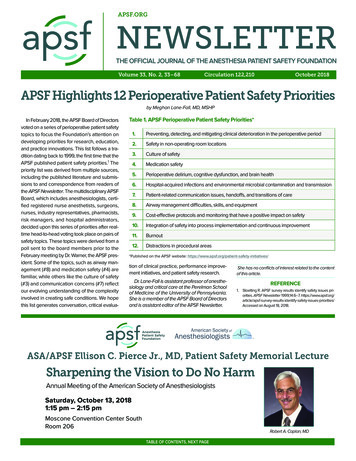
APSF.ORGNEWSLETTERTHE OFFICIAL JOURNAL OF THE ANESTHESIA PATIENT SAFETY FOUNDATIONVolume 33, No. 2, 33–68Circulation 122,210October 2018APSF Highlights 12 Perioperative Patient Safety Prioritiesby Meghan Lane-Fall, MD, MSHPIn February 2018, the APSF Board of Directorsvoted on a series of perioperative patient safetytopics to focus the Foundation’s attention ondeveloping priorities for research, education,and practice innovations. This list follows a tradition dating back to 1999, the first time that theAPSF published patient safety priorities.1 Thepriority list was derived from multiple sources,including the published literature and submissions to and correspondence from readers ofthe APSF Newsletter. The multidisciplinary APSFBoard, which includes anesthesiologists, certified registered nurse anesthetists, surgeons,nurses, industry representatives, pharmacists,risk managers, and hospital administrators,decided upon this series of priorities after realtime head-to-head voting took place on pairs ofsafety topics. These topics were derived from apoll sent to the board members prior to theFebruary meeting by Dr. Warner, the APSF president. Some of the topics, such as airway management (#8) and medication safety (#4) arefamiliar, while others like the culture of safety(#3) and communication concerns (#7) reflectour evolving understanding of the complexityinvolved in creating safe conditions. We hopethis list generates conversation, critical evalua-Table 1. APSF Perioperative Patient Safety Priorities*1.Preventing, detecting, and mitigating clinical deterioration in the perioperative period2.Safety in non-operating room locations3.Culture of safety4.Medication safety5.Perioperative delirium, cognitive dysfunction, and brain health6.Hospital-acquired infections and environmental microbial contamination and transmission7.Patient-related communication issues, handoffs, and transitions of care8.Airway management difficulties, skills, and equipment9.Cost-effective protocols and monitoring that have a positive impact on safety10.Integration of safety into process implementation and continuous improvement11.Burnout12.Distractions in procedural areas*Published on the APSF website: on of clinical practice, performance improvement initiatives, and patient safety research.She has no conflicts of interest related to the contentof this article.Dr. Lane-Fall is assistant professor of anesthesiology and critical care at the Perelman Schoolof Medicine of the University of Pennsylvania.She is a member of the APSF Board of Directorsand is assistant editor of the APSF Newsletter.1. Stoelting R. APSF survey results identify safety issues priorities. APSF Newsletter 1999;14:6–7. dentify-safety-issues-priorities/Accessed on August 18, 2018.REFERENCEASA/APSF Ellison C. Pierce Jr., MD, Patient Safety Memorial LectureSharpening the Vision to Do No HarmAnnual Meeting of the American Society of AnesthesiologistsSaturday, October 13, 20181:15 pm – 2:15 pmMoscone Convention Center SouthRoom 206Robert A. Caplan, MDTABLE OF CONTENTS, NEXT PAGE
APSF NEWSLETTER October 2018PAGE 34TABLE OF CONTENTSARTICLES:APSF Highlights 12 Perioperative Patient Safety Priorities for 2018. CoverEarly Warning Systems: “Found Dead in Bed” Should be a Never Event. Page 35Is a Concussed Brain a Vulnerable Brain? Anesthesia after Concussion. Page 39Catch Me If You Can: Patient Falls in the Anesthesia Workplace. Page 41Anesthesia Professional Burnout—A Clear and Present Danger. Page 43APSF Recognizes Best Practices for Safe Medication Administration during Anesthesia Care. Page 45Multimodal Analgesia and Alternatives to Opioids for Postoperative Analgesia. Page 46Medication Safety Alerts for Anesthesia Professionals. Page 48Safe Use of High-Flow Nasal Oxygen (HFNO) With Special Reference to DifficultAirway Management and Fire Risk. Page 51Successful Implementation of a Two-Hour Emergency Manual (EM)Simulation Instructor Training Course for Anesthesia Professionals in China. Page 60Obesity and Robotic Surgery. Page 65DEAR SIRS: urette Malpositioned Shut Off Valve Could Lead to Venous Air Embolism. Page 49BLTA Tip Breaks in Patient’s Airway. Page 56Potential Burn Hazard from General Electric MRIs. Page 58Defective Central Venous Catheter Introducer Needle. Page 62Volatile Anesthetic Unintentionally Not Delivered. Page 64LETTER TO THE EDITOR:A Novel Approach to Eliminating Wrong-Site Blocks. Page 63APSF ANNOUNCEMENTS:ASA/APSF Ellison C. Pierce Jr., MD, Patient Safety Memorial Lecture . CoverGuide for Authors. Page 34Get Social With Us. Page 38Grant Application Announcement. Page 38International Forum on Perioperative Safety & Quality (ISQ). Page 38Corporate Advisory Council. Page 382018 Corporate Giving Opportunities. Page 54APSF Donor Page. Page 55APSF Grant Alumni Academy Workshop . Page 57ASA/APSF Featured Session: APSF Panel. Page 60APSF Newsletter Guide for AuthorsThe APSF Newsletter is the official journal of the Anesthesia Patient Safety Foundation. It is widely distributedto a variety of anesthesia professionals, perioperativeproviders, key industry representatives, and risk managers. It is published three times a year (February, June,and October). Deadlines for each issue are as follows:1) February Issue: November 15th, 2) June Issue:March 15th, 3) October Issue: July 15th. The content ofthe newsletter typically focuses on anesthesia-relatedperioperative patient safety. Decisions regarding content and acceptance of submissions for publication arethe responsibility of the editors. Some submissions maygo in future issues, even if the deadline is met. At thediscretion of the editors, submissions may be considered for publication on our APSF website and socialmedia pages.Types of articles include:(1) Review articles or invited pro-con debates are original manuscripts. They should focus on patient safetyissues and have appropriate referencing (see https://www.apsf.org/authors-guide.php). The articlesshould be limited to 2,000 words with no more than25 references. Figures and/or tables are stronglyencouraged.(2) Q&A articles are anesthesia patient safety questionssubmitted by readers to knowledgeable experts ordesignated consultants to provide a response. Thearticles should be limited to 750 words.(3) Letters to the editor are welcome and should be limited to 500 words. Please include references whenappropriate.(4) Dear SIRS is the “Safety Information ResponseSystem.” The purpose of this column is to allow expeditious communication of technology-related safetyconcerns raised by our readers, with input andresponse from manufacturers and industry representatives. Dr. Jeffrey Feldman, current chair of the Committee on Technology, oversees the column andcoordinates the readers’ inquiries and the responsefrom industry.(5) Invited conference reports summarize clinically relevant anesthesia patient safety topics based on therespective conference discussion. Please limit theword count to less than 1000.Commercial products are not advertised or endorsed bythe APSF Newsletter; however, upon exclusive consideration from the editors, articles about certain novel andimportant safety-related technological advances maybe published. The authors should have no commercialties to, or financial interest in, the technology or commercial product.If accepted for publication, copyright for the acceptedarticle is transferred to the APSF. Except for copyright, allother rights such as for patents, procedures, or processes are retained by the author. Permission to reproduce articles, figures, tables, or content from the APSFNewsletter must be obtained from the APSF.Individuals and/or entities interested in submittingmaterial for publication should contact the editor-inchief directly at greenberg@apsf.org. Please refer tothe APSF Newsletter link: https://www.apsf.org/authors-guide.php for detailed information regardingspecific requirements for submissions.NEWSLETTERThe Official Journal of theAnesthesia Patient Safety FoundationThe Anesthesia Patient Safety Foundation Newsletteris the official publication of the nonprofit AnesthesiaPatient Safety Foundation and is published threetimes per year in Wilmington, Delaware. Individualsubscription– 100, Cor por ate– 500. Contri butionsto the Foundation are tax-deduct ible. Copy right,Anesthesia Patient Safety Foundation, 2018.The opinions expressed in this Newsletter are notnecessarily those of the Anesthesia Patient SafetyFoundation. The APSF neither writes nor promulgates standards, and the opinions expressed hereinshould not be construed to constitute practice standards or practice parameters. Validity of opinions presented, drug dosages, accuracy, and completenessof content are not guaranteed by the APSF.APSF Executive Committee 2018:Mark A. Warner, MD, President, Rochester, MN; DanielJ. Cole, MD, APSF Vice President, Los Angeles, CA;Matthew B. Weinger, MD, Secretary, Nashville, TN;Douglas A. Bartlett, APSF Treasurer, Boulder, CO; Mariavan Pelt, CRNA, PhD, Director At-Large, Boston, MA.APSF Newsletter Editorial Board 2018:Steven B. Greenberg, MD, Editor-in-Chief, Chicago, IL;Edward A. Bittner, MD, PhD, Associate Editor, Boston,MA; Jennifer M. Banayan, MD, Assistant Editor, Chicago, IL; Meghan Lane-Fall, MD, Assistant Editor, Philadelphia, PA; Trygve Armour, MD, Rochester, MN; JWBeard, MD, Wilmette, IL; Joan M. Christi.e., MD, St.Petersberg, FL; Heather Colombano, MD, WinstonSalem, NC; Jan Ehrenwerth, MD, New Haven, CT; JohnH. Eichhorn, MD, San Jose, CA; Nikolaus Gravenstein,MD, Gainesville, FL; Joshua Lea, CRNA, Boston, MA;Bommy Hong Mershon, MD, Baltimore, MD; Tricia A.Meyer, PharmD, Temple, TX; Glenn S. Murphy, MD, Chicago, IL; Brian Thomas, JD, Kansas City, MO; Jeffrey S.Vender, MD, Winnetka, IL; Wilson Somerville, PhD, Editorial Assistant, Winston-Salem, NC. Please see thelinks of international editors at /APSF-InternationalEditors.pdfAddress all general, contributor, and sub scriptioncorrespondence to:Stacey Maxwell, AdministratorAnesthesia Patient Safety FoundationCharlton 1-145Mayo Clinic200 1st Street SWRochester, MN 55905maxwell@apsf.orgAddress Newsletter editorial comments, questions,letters, and suggestions to:Steven B. Greenberg, MDEditor-in-Chief, APSF Newslettergreenberg@apsf.orgEdward A. Bittner, MD, PhDAssociate Editor, APSF Newsletterbittner@apsf.orgJennifer M. Banayan, MDAssistant Editor, APSF Newsletterbanayan@apsf.orgMeghan Lane-Fall, MDAssistant Editor, APSF Newsletterlanefall@apsf.orgSend contributions to:Anesthesia Patient Safety FoundationCharlton 1-145Mayo Clinic200 1st St SWRochester, MN 55905, U.S.A.Or please donate online at www.apsf.org.
APSF NEWSLETTER October 2018PAGE 35Early Warning Systems: “Found Dead in Bed”Should be a Never Eventby Bradford D. Winters, MD, PhD, FCCMA PATIENT SAFETY PROBLEMClinical deterioration on the general hospitalwards is common and all too often results inpatients progressing to cardiopulmonary arrest,which carries significant morbidity and mortality.1-5 Occasionally, this progression is not witnessed or perhaps even worse, observed butunrecognized,1,6 resulting in an unmonitored/unwitnessed arrest. These events are currentlycategorized as a serious adverse event (AE) byseveral reporting metrics including the American Heart Association’s Get with the Guidelines 7 and the Agency for Healthcare Researchand Quality’s (AHRQ) Patient Safety Indicators(PSIs).8 Surgical patients may be prone to cardiopulmonary arrest due to their underlying diseases (especially conditions such as obstructivesleep apnea and cardiac disease), the surgicalprocedure, and the administration of opioidscoupled with residual anesthesia.9,10 This is amajor concern for anesthesia professionals whohelp determine if the patient is safe to go to anunmonitored floor or should request a monitoredbed which may be a limited resource.THE RAPID RESPONSE SYSTEM AS APATIENT SAFETY INTERVENTIONIn the mid-1990s, Rapid Response Systems(RRS) were implemented to address this patientsafety problem.4,11,12 RRSs are composed of twomain elements. The most visible element is theteam that responds to the call for help for thedeteriorating patient. These teams are often,though not always, made up of intensive careunit providers and are referred to as the “efferent limb” of the response. The “afferent limb”refers to the process and criteria by which clinical deterioration is recognized and a rapidresponse team is activated. The afferent limbuses activation criteria, education programs,and policy changes to encourage providers toactivate the efferent limb whenever a patient’scondition appears to be deteriorating. Understanding and developing effective and validactivation criteria is perhaps the most crucialcomponent of the RRS2, even though the rapidresponse team (efferent limb) is essential to thesuccess of these systems. Therefore, theseactivation criteria have evolved over time into awide range of Early Warning Scores (EWS).Beginning in the early 1990s, common predictors of clinical deterioration were identifiedfrom the medical records of patients that hadarrested on the general ward.2,5,6 The predictors identified were primarily physiologicalchanges (elevated heart rate, low blood pres-sure, or mental status change) and were oftenfound to be present for many hours prior to thearrest event. The ability to identify thesechanges indicated potential opportunities forearly intervention. Presumably, the earlier warning signs are recognized, the more effective theintervention could be. Even though RRS havebeen successful in reducing in-hospital mortality and unanticipated cardiopulmonary arrest,they have failed to achieve their full potential.4,9,10 Failure of health care professionals torecognize the deteriorating patient and theinability of existing data systems to trigger anappropriate response in a timely manner remainpervasive.ADDRESSING AFFERENT LIMB FAILUREUSING EARLY WARNING SCORESEfforts to address deficiencies in early identification of clinical deterioration (i.e., afferentlimb failure) have taken several approachesincluding education programs, nurse empowerment initiatives, and increasingly the use ofdata-driven systems to improve clinicalresponse. Initially, hospitals used single vitalsign parameter thresholds in combination with“clinical concern” about the patient by the bedside nursing staff as activation criteria and manystill do. Many hospitals subsequently developed and implemented “early warning scores”(EWSs) that attempt to integrate vital signs andlaboratory data (e.g., lactic acid) to improve thesensitivity and specificity for earlier detection.Some studies of EWSs have shown improve-ment in patient outcomes compared with singleparameter vital signs systems while others haveshown little difference in outcomes.3,13-36 Thesedifferences in study findings may result fromuse of overly strict or loose criteria for signalinga deterioration (e.g., extreme heart-rate cutoffs),use of nonequivalent outcomes (such as totalcardiac arrest rate vs. non-ICU cardiac arrestrate), ineffective education programs to encourage appropriate RRS activation, lack of policies tosupport the intervention, poor project implementation, and variable acceptance in the medicalcare culture, among others.A number of EWSs are worth focusing on.One of the earliest published in the literaturewas by Subbe et al. in 2003.13 This groupdeveloped a manual multiparameter scoringsystem, which assigned points based on thedegree of abnormality of each parameter. TheirEWS included mental status in addition tophysiologic vital signs. When patients exceededa threshold score ( 4), they were referred forclinical evaluation. Unfortunately, its initialimplementation did not show an improvementin outcomes. In 2006, Green and Williamsreported the results of an “Early Warning ClinicalMarker Referral Tool,” which incorporated singleparameter vital signs. While the authors wereunable to demonstrate improved outcomes withthe EWS, it did result in patients being referred forICU admission with fewer markers of instabilityand illness suggesting that such a score couldSee “Early Warning Systems,” Next Page
APSF NEWSLETTER October 2018PAGE 36A Variety of Early Warning Systems Are AvailableFrom “Early Warning Systems,” Preceding PageNational Health Service. When ViEWS wasapplied to previously collected datasets, itsability to predict cardiac arrest and death wassuperior to other existing EWSs.17,19 A simplifiedversion of ViEWS was then validated in aCanadian regional hospital on actual patientswhere it was found to be effective for generalward medical and surgical patients.16 Table 1includes a list of several clinically evaluatedEWSs.lead to earlier recognition of deterioration. Inanother study, Rothschild et al.18 implementeda single parameter EWS for patients ongeneral medical wards. They found that whileearly warning conditions used to activate RRSteams were only fair predictors of acutedeterioration, early signs of respiratory failureduring routine monitoring were stronglyassociated with future life-threatening adverseevents. In that same year, Prytherch et al.described an EWS called ViEWS (VitalPAC EWS, Sussex Place, London).17 This dataaggregated and weighted “track and trigger”system was developed to potentially becomea national standard in the United Kingdom’sA 2014 systematic review of the EWS literaturefor use on general ward patients included 1randomized controlled trial and 20 observationalstudies that evaluated 13 different EWS systems.Some EWSs used in the studies consisted ofsingle parameters systems while others usedintegrated scoring systems. Some sought toidentify specific clinical conditions such assepsis. Eight studies (all observational) examinedthe ability of an EWS to predict death orcardiopulmonary arrest. Collectively, thesestudies showed that EWSs perform well forprediction of cardiac arrest and death within 48hours. Thirteen studies examined the impact ofEWS on health outcomes and resourceutilization with mixed results.37 This suggests thatEWSs’ impact on outcome is uncertain, but theymay be able to identify deteriorating patients.More recently, predictive algorithms usingmachine learning and big data have beenproposed and developed, with improved abilitySee “Early Warning Systems,” Next PageTable 1. Table of Selected Early Warning ScoresEWS NameStudy FirstAuthorDate ofpublicationCountrySingle vs.combined scoring# ofparametersEffect on Incidence ofCardiac ArrestEffect on MortalityMEWSO’Dell312002UKcombined5 itemsNot studiedNot studiedMEWSSubbe132003UKcombined5 itemsNot studiedNo statistical changeMEWSSmith332006UKcombined6 itemsNot studiedNot studiedClinical MarkerToolGreen262006Australiacombined7 itemsNot clear*No effectMEWSMaupin282009USAcombined5 itemsNot Clear†Not studiedNoneRothschild182010USAsingle13 itemsNot studiedNot studied“ViEWS”Prytherch172010UKcombined7 itemsNot studiedNot studiedMEWSMitchell292010Australiacombined7 itemsNot studiedNot studiedMEWSAlbert242011USAcombined12 itemsNot studiedNot studied27“PatientTrack”Jones2011UKcombined5 items2 sub-groups showed nochange and one showed asignificant increaseNo statistical changeMEWSPatel322011UKcombined6 itemsNot studiedNo statistical changeMEWSMoon302011UKcombined7 itemsSignificantly improvedSignificantly improvedCART (CardiacArrest RiskTriage)Churpek202012USAcombined4 itemsNot studiedNot studiedMEWSChurpek212012USAcombined5 itemsNot studiedNot ed6 itemsNot studiedNot studiedMEWSDeMeester252012Belgiumcombined6 itemsNot studiedNo statistical changeNEWSSmith192013UKcombined7 itemsNot studiedNot studiedEWSs reported in Systematic Review by Smith et al.36 MEWS—Modified Early Warning Scores. NEWS—UK national EWS. All multiple parameter MEWSused heart rate, blood pressure and respiratory rate. Most also used temperature and one half used oxygen saturation. (*) showed a statistically significantreduction in incidence of arrest events but did not provide denominator data to calculate rates. (†) showed a reduction from 0.77 to .39/1000 patient daysbut did not provide statistics.
APSF NEWSLETTER October 2018PAGE 37Further Research Required to Determine TrueOutcome Benefits Using EWSFrom “Early Warning Systems,” Preceding Page38to predict clinical deterioration. Machine learning is an artificial intelligence process wherebycomputer algorithms “self-learn” and improvetheir performance through training on datasetswithout the need for reprogramming. While conceptually appealing, EWSs need to demonstratethat their implementation can improve clinicaloutcomes.Several explanations have been proposed toexplain the failure of existing EWSs in improvingclinical outcomes. First, the frequency of vitalsign acquisition on the wards may be insufficient to allow detection of clinical deterioration.6A second possible explanation is that vital signvalues may have inaccuracies and audits of vitalsign data confirm this.39 Electronic health records(EHRs) do little to improve this situation as theirperformance is dependent on the intermittentlyand sometimes inaccurately collected datapoints. Third, recognition, response, and communication to the clinical team may not be timelyenough. Therefore, it is not surprising that EWSsand the afferent limb of RRS don’t necessarilylive up to their presumed potential.Surveillance monitoring may be a better wayto collect and act on clinical data for a patientwho is deteriorating on a general ward.40,41Surveillance monitoring is distinguished from“condition monitoring,” which is employed inICUs where the patients are unstable or are atrisk for instability and the staff-to-patient ratio isadjusted accordingly. In contrast, general wardpatients are generally at low risk for instabilityand the staff-to-patient ratio is much lower.Surveillance monitoring seeks to identify theinfrequent occurrence of clinical deterioration inotherwise low-risk patients. General medicalpatients and especially postsurgical patients onthe wards are at risk of a variety of complicationsincluding arrhythmias, myocardial ischemia,sepsis, respiratory insufficiency, and bleedingcomplications. Surveillance monitoring offers thepossibility of improving upon many of the limitingfeatures of existing EWSs that are thought to beat the core of afferent limb failure; it is continuous,relies less on fallible humans, is potentially moreaccurate,and, if automatically linked to anactivation hierarchy such as a pager or mobilephone escalation protocol, may be able tocircumvent the continued lack of appreciation ofthe patient’s developing deterioration.Surveillance monitoring still needs to overcome several hurdles that may be challenging.First, it needs to be mobile and wireless sincegeneral ward patients are usually ambulatoryas compared to monitoring of ICU patients,who are much less so. Wireless technologyhas advanced tremendously in the lastdecade, and wireless systems now exist thatmay meet this need.42 Embedded in the use ofthis technology is the need to meet everchanging and more stringent security standards to protect not only patients’ information,but also hospitals’ health information technology systems. A second requirement is theneed for the mobile surveillance monitor tohave adequate battery life. The need for frequent battery changes/recharges would makesuch a system impractical. A third requirementis the need for the monitor to be comfortableand relatively unobtrusive. Ambulatory general ward patients will not likely tolerate wearing heavy or uncomfortable monitoringequipment. Fourth, the vital-sign data collection should be continuous, since use of intermittently collected data may miss early signsof deterioration. Fifth, it needs to have anacceptable accuracy and a manageable falsealarm rate. Condition monitoring in the ICU(e.g., certain ECG alarms) has a high falsealarm rate. These high false alarm rates maylead to alarm fatigue, which is a widely recognized patient safety issue in which alarms areignored or there is a delayed response.43 Anacceptable false alarm rate for clinical monitoring of ward patients is uncertain. However, theneed to control alarm fatigue must be balanced against the potential benefit that maybe derived by obtaining continuous higherfidelity data.Studies of surveillance monitoring are stilllimited but the results are encouraging. Severalstudies have demonstrated success using primarily pulse oximetry surveillance monitoring inpost-surgical patients.44-49 A recent study42examined a multiparameter wireless surveillance monitoring system on a neurological/neurosurgical ward and found that the averagealarm rate for all alarms (SpO2, HR, RR, NIBP)was 2.3 alarms/patient/day and the RRS activation rate was reduced. Other measured outcomes, such as readmission to the ICU, did notshow a statistically significant improvementthough there was a positive trend in the rightdirection. We have tested a similar system on ageneral postsurgical ward and found similartrends.50CONCLUSIONUnrecognized and unattended clinical deterioration on general hospital wards must beavoided. The implementation of RRSs hasreduced the occurrence of such events butbetter methods to predict early deteriorationand to link this to interventions are needed tofurther improve outcomes. Despite improvements in EWS and surveillance monitoring, itwill still be necessary for providers to act in atimely manner, develop an appropriate differential diagnosis quickly, gather additional relevantdata as needed, and institute effective evidence-based therapies including necessarytriage to a higher level of care to improvepatient outcomes.Dr. Winters is the division director for CriticalCare Medicine in the Johns Hopkins Dept. ofAnesthesiology and Critical Care Medicine andco-director of the Surgical Intensive Care Units atthe Johns Hopkins University School of Medicine.He reports no conflicts of interest pertaining to thisarticle.REFERENCES:1. Smith AF, Wood J. Can some in-hospital cardio-respiratory arrests be prevented? A prospective survey.Resuscitation 1998;37:133–137.2. Devita MA, Smith GB, Adam SK, et al. Identifying thehospitalized patient in crisis—a consensus conferenceon the afferent limb of the Rapid Response Systems.Resuscitation 2010;81:375–382.3. Bellomo R, Ackerman M, Bailey M, et al. A controlledtrial of electronic automated vital signs monitoring ingeneral hospital wards. Crit Care Med 2012;40:2349–2361.4. Winters BD, Weaver SJ, Pfoh ER, et al. Rapid responsesystems as a patient safety strategy: a systematicreview. Ann Int Med 2013;158:417–425.5. Herlitz JA, Bang A, Aune S, et al. Characteristics andoutcome among patients suffering in-hospital cardiacarrest in monitored and non-monitored areas. Resuscitation 2001;48:125–135.6. Buist MD, Jarmolowski E, Burton PR, et al. Recognisingclinical instability in hospital patients before cardiacarrest or unplanned admission to intensive care. A pilotstudy in a tertiary-care hospital. Med J Aust 1999;171:22–5.7. Brady WJ, Gurka KK, Mehrin
In February 2018, the APSF Board of Directors . Review articles or invited pro-con debates are origi - nal manuscripts. They should focus on patient safety . Mayo Clinic 200 1st St SW Rochester, MN 55905, U.S.A. Or please donate online at www.apsf.org. NEWSLETTER. APSF NEWSLETTER October 2018 PAGE 35