Transcription
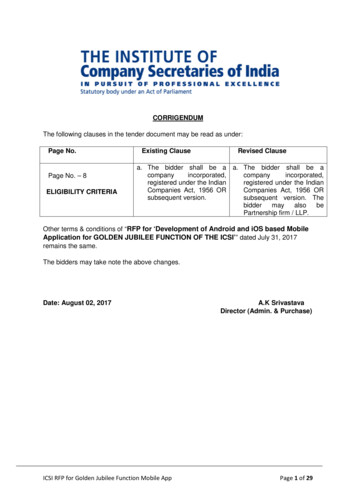
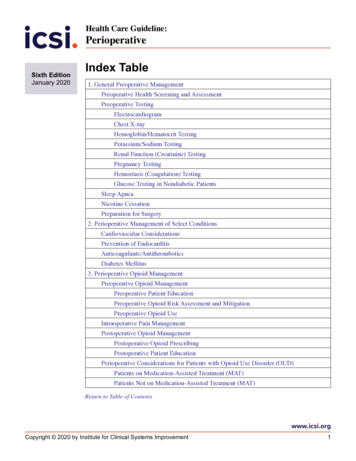
Health Care Guideline:PerioperativeSixth EditionJanuary 2020Index Table1. General Preoperative ManagementPreoperative Health Screening and AssessmentPreoperative TestingElectrocardiogramHemoglobin/Hematocrit TestingChest X-rayPotassium/Sodium TestingRenal Function (Creatinine) TestingPregnancy TestingHemostasis (Coagulation) TestingGlucose Testing in Nondiabetic PatientsSleep ApneaNicotine CessationPreparation for Surgery2. Perioperative Management of Select ConditionsCardiovascular ConsiderationsPrevention of EndocarditisAnticoagulants/AntithromboticsDiabetes Mellitus3. Perioperative Opioid ManagementPreoperative Opioid ManagementPreoperative Patient EducationPreoperative Opioid UsePreoperative Opioid Risk Assessment and MitigationIntraoperative Pain ManagementPostoperative Opioid ManagementPostoperative Opioid PrescribingPostoperative Patient EducationPerioperative Considerations for Patients with Opioid Use Disorder (OUD)Patients on Medication-Assisted Treatment (MAT)Patients Not on Medication-Assisted Treatment (MAT)Return to Table of Contentswww.icsi.orgCopyright 2020 by Institute for Clinical Systems Improvement1
PerioperativeSixth Edition /January 2020Table of ContentsPerioperativeGuideline WorkGroup LeaderMayo ClinicNicole Varela, MDAnesthesiologyPerioperativeGuideline WorkGroup MembersAllina HealthJoshua Mueller, MDInternal MedicineEntira Family Clinics(formerly of)Hannah Degallier, PA-CFamily MedicineEssentia HealthMark Grimm, MDAnesthesiologyFairview HealthServicesDeborah Mielke, MDFamily MedicineJoan Kane, APNL,CRNANursing/AnesthesiaHealthPartnersLouis Millman, MDInternal MedicineRebekah Roemer,PharmD, BCPSPharmacyMayo ClinicAdam Jacob, MDAnesthesiologyNathaniel Miller, MDFamily rsAllina HealthJustin Hora, PharmDPharmacyEntira Family ClinicsDavid Thorson, MDFamily Medicine/SportsMedicineEssentia HealthJoseph Bianco, MDInternal MedicineMark Grimm, MDAnesthesiologyHealthPartnersAnne Pylkas, MDInternal Medicine/Addiction MedicineIsaac Marsolek, MDPhysical Medicine &RehabilitationRebekah Roemer,PharmD, BCPSPharmacyHennepin HealthcareCharles Reznikoff, MDInternal Medicine/Addiction MedicineMayo ClinicAdam Jacob, MDAnesthesiologyAnnotations. 1–59Index Table.1Evidence Grading.3Recommendations Table. 4–9Foreword.10–11Introduction. 10Scope and Target Population. 11Aims. 11Implementation Recommendations Highlights. 11Related ICSI Scientific Documents. 11Definitions. 11Annotations.12–59Quality Improvement Support.60–63Aims and Measures. 61Implementation Recommendations. 62Implementation Tools and Resources. 62Implementation Tools and Resources Table. 63Supporting Evidence.64–76References.65–75Appendix. 76Appendix A: Literature Search Description. 76Disclosure of Potential Conflicts of Interest.77–80Acknowledgements. 81Document History and Development.82–84Document History. 83ICSI Document Development and Revision Process. 84ICSISenka Hadzic, MPHFacilitatorNicole Varela, MDAnesthesiologyJodie Dvorkin, MD,MPHCo-FacilitatorNorth Memorial HealthSarah Lippert, MDGeneral SurgeryAudrey Hansen, MA,BSNCo-FacilitatorUniversity of Minnesota(formerly of)Kathleen Harder, PhDHuman Factorswww.icsi.orgInstitute for Clinical Systems Improvement2
PerioperativeSixth Edition /January 2020Evidence GradingLiterature SearchA consistent and defined literature search process is used in the development and revision of ICSI guidelines.See Appendix A for literature search parameters and search terms. In addition to the literature searches,articles were obtained by work group members and ICSI staff. Those vetted by the work group were includedin the guideline when appropriate.MethodologyICSI utilizes the Grading of Recommendations Assessment, Development and Evaluation (GRADE) methodology system. GRADE involves systematically evaluating the quality of evidence (high, moderate, low,very low) and developing a strength of recommendation (strong, weak). For more detailed information onGRADE, please visit http://www.gradeworkinggroup.org/. In addition, when GRADE methodology couldnot be applied, the work group developed consensus recommendations.Return to Table of Contentswww.icsi.orgInstitute for Clinical Systems Improvement3
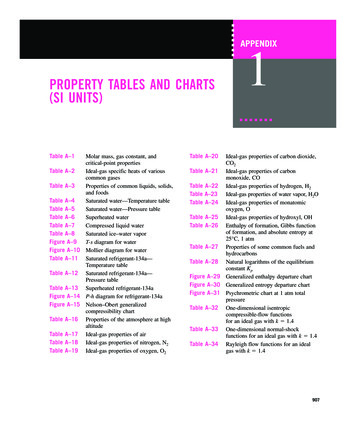
PerioperativeSixth Edition /January 2020Recommendations TableThe following table is a list of evidence-based recommendations for the Perioperative Guideline based on thereview of primary literature and secondary references (in instances where primary literature was not found).TopicPreoperativeHealthScreening andAssessmentPreoperativeTestingQuality ofEvidenceRecommendation(s)LowDo not routinely test all patientsundergoing elective, noncardiacsurgery.NotapplicableChest X-rayLowHemoglobin/HematocritTestingLowA preoperative health screeningand assessment that includesa focused medical history andappropriate physical examinationshould be completed for all patientsundergoing a surgical procedure,regardless of setting (unless theprocedure involves mild sedation,or local/topical anesthesia).The need for testing should beguided by individual patient’sclinical risk factors (based onmedical history and physicalexamination) and the risk of majoradverse cardiac event (morbidityor mortality) associated with theplanned procedure.Do not routinely perform chestX-rays preoperatively unlessindicated by the review of medicalhistory and physical examination.Do not routinely test forhemoglobin preoperatively inhealthy, asymptomatic patients.Testing for preoperative hemoglobinlevel should be considered in:1. Patients with a history of anemiaor history suggesting recentblood loss or anemia and theplanned procedure may leadto significant blood loss orphysiologic stress or2. Patients with prior or plannedanticoagulation (expertconsensus).Strength ofRelevant ResourcesRecommendationConsensusFleisher, 2014(Guideline); Apfelbaum,2012b (Guideline)StrongKeay, 2019 (SystematicReview); Johansson,2013 (SystematicReview); Munro, 1997(Systematic Review)StrongJohansson, 2013(Systematic Review);Joo, 2005 (SystematicReview)StrongFowler, 2015 (MetaAnalysis); Johansson,2013 (SystematicReview); Munro, 1997(Systematic Review)Return to Table of Contentswww.icsi.orgInstitute for Clinical Systems Improvement4
PerioperativeSixth Edition /January 2020Recommendations TableTopicPotassium/Sodium TestingRenal Function(CreatinineTesting)PregnancyTestingQuality ofEvidenceLowLowNotApplicableRecommendation(s)Do not routinely test for potassiumor sodium level preoperatively inhealthy, asymptomatic patients.Testing may be indicated in:1. Patients who are on diuretictherapy,2. Patients with kidney disease(stages 3–5),3. Patients on potassiumreplacement therapy, or4. Patients undergoing bowelpreparation.Do not routinely test for creatininelevels in healthy, asymptomaticpatients.Testing may be indicated in patientswith known kidney disease orpatients with a comorbid condition(e.g., diabetes, hypertension) thatcarries increased risk of acutekidney injury or kidney disease.Do not routinely conduct urine testsfor pregnancy. However, patients ofchildbearing age should be asked ifthere is a possibility they might bepregnant.Pregnancy testing is indicated in:1. Patients planning to undergosurgeries involving theuterus (e.g., hysterectomy,myomectomy),2. Uterine cavity surgery(e.g., dilation and curettage,endometrial ablation), or3. Surgery that impacts blood flowto the uterus (e.g., endovascularsurgeries that disrupt aorticblood flow, procedures involvingthe uterine arteries).Strength ofRelevant ResourcesRecommendationStrongJohansson, 2013(SystematicReview); Wahr,1999 (ObservationalStudy); Munro, 1997(Systematic Review)StrongKork, 2015(Observational Study),Johansson, 2013(Systematic Review)ConsensusACOG, 2019 (JointStatement with ASA);ASA, 2016 (Statement);NICE, 2016(Guideline); Apfelbaum,2012b (Guideline)Return to Table of Contentswww.icsi.orgInstitute for Clinical Systems Improvement5
PerioperativeSixth Edition /January 2020Recommendations TableTopicHemostasis(Coagulation)TestingGlucose Testingin NondiabeticPatientsQuality ofEvidenceLowNotApplicableRecommendation(s)Do not routinely performcoagulation tests before surgeryunless indicated.Indications for testing may includethe following:1. Patients with potential bleeding/clotting problem,2. Patients with a known history ofbleeding/clotting abnormalities,3. Patients with recent historysuggesting the potential forbleeding/clotting problems,4. Patients who are currently takinganticoagulant therapy, and5. Patients who may needpostoperative anticoagulation(where a baseline may beneeded).Consider glucose testing inpatients with risk factors fordiabetes (as defined by USPSTFrecommendations), or if a primarycare provider feels that diagnosisof diabetes would alter the plan forsurgery.Strength ofRelevant ResourcesRecommendationStrongJohansson, 2013(Systematic Review);Munro, 1997(Systematic Review)ConsensusUSPSTF, 2015(Guideline)Return to Table of Contentswww.icsi.orgInstitute for Clinical Systems Improvement6
PerioperativeSixth Edition /January 2020Recommendations TableTopicSleep ApneaNicotineCessationQuality ofEvidenceRecommendation(s)LowSmoking cessation intervention(brief or intensive) should beinitiated before elective surgery.NotapplicableStrength ofRelevant ResourcesRecommendation1. Clinicians should use a validated Consensusstandardized screening tool toscreen patients for suspectedsleep apnea (risk factors orpatient reporting problems) orsleep apnea symptoms, andcommunicate to the surgicalteam. Major risk factors forsleep apnea include obesity,increased neck size ( 37 cmin men, 35 cm in women),craniofacial abnormalities, olderage and male sex.2. Clinicians should remindpatients who have been formallydiagnosed with obstructive sleepapnea and have an oral applianceor continuous positive airwaypressure equipment to bringtheir appliance or equipmentwith them on the operative dayfor use during the recovery fromanesthesia or sedation.3. Patients with suspected sleepapnea in the perioperativeperiod should have a follow-upevaluation, typically in concertwith the patient’s primaryprovider (if one is available),and/or referral to sleep center.4. Patients with known sleep apneaor suspected sleep apnea at apreoperative evaluation shouldhave this communicated to thesurgical and anesthesiology teamand the patient made aware thismay increase the surgical risk.StrongChung, 2016(Guideline); Gross,2014 (Guideline)Bayfield, 2018 (MetaAnalysis); Nolan, 2017(Observational Study);Nolan, 2015 (SystematicReview); Thomsen,2014 (SystematicReview)Return to Table of Contentswww.icsi.orgInstitute for Clinical Systems Improvement7
PerioperativeSixth Edition /January 2020Recommendations TableTopicHbA1c Testingin Patients withDiabetes duringPreoperativeClinic VisitQuality rativeGlycemicControl Targetsfor Patients withDiabetesPreoperativeNotOpioid Tapering ApplicableRecommendation(s)Consider obtaining a preoperativeHbA1c test value, if not done in thepast three months, on patients withknown diabetes during preoperativeclinic visit.Strength ofRelevant ResourcesRecommendationConsensusEstablish a plan for managementof diabetes prior to surgery. Thedecision to proceed with surgeryor postpone surgery based onpreoperative HbA1c test valueshould be based on individualpatient-centered factors such asurgency of planned surgery, overallmortality/morbidity risks, risks ofperioperative infections, concernsfor postoperative glucose control,and patient compliance.Consider a glycemic target rangeWeakbetween 140-180 mg/dL for surgicalpatients with diagnosed diabetesduring the intraoperative andpostoperative periods.Additional considerations:1. For patients with diabetes withglucose levels typically 140, donot treat to 140.2. Consider risk for hypoglycemiaif necessary to treat for glycemictargets lower than 140.An individualized approach fortapering in patients who are onopioids preoperatively (includingpatients with chronic opioid use)should be taken.A decision on whether to taperpreoperatively needs to be madewell in advance of surgery.However, if a significant medicalconcern about opioid use isrecognized closer to the surgerydate that could be made safe with ataper, the patient, the provider andthe surgical team should discusswhether delaying the surgeryin order to treat the underlyingcondition is appropriate.ConsensusADA-Diabetes Carein the Hospital,2019 (Guideline);van den Boom, 2018(ObservationalStudy); NICE, 2016(Guideline); Yang, 2016(Observational Study);Gustafsson, 2009(Observational Study)Nair, 2016(Observational Study);Sathya, 2013 (MetaAnalysis); Buchleitner,2012 (SystematicReview); Gandhi,2007 (RandomizedControlled Trial); Ata,2010 (ObservationalStudy); Ramos, 2008(Observational Study)Jain, 2019(ObservationalStudy); Nguyen, 2016(Randomized ControlledTrial); Hassamal, 2016(Case Series)Return to Table of Contentswww.icsi.orgInstitute for Clinical Systems Improvement8
PerioperativeSixth Edition /January 2020Recommendations TableTopicPostoperativeOpioidPrescribingQuality ofEvidenceNotApplicableRecommendation(s)Strength ofRelevant ResourcesRecommendationThe postoperative prescribed opioid Consensusdoses at discharge should be thelowest effective dose of short-actingopioids.Hill, 2018(ObservationalStudy); Koehler,2018 (SystematicReview); Mark, 2018(Observational Study);Bicket, 2017 (SystematicReview); Osmundson,2017 (ObservationalStudy); Thiels, 2017(ObservationalStudy); Ray, 2016(ObservationalStudy); Miller, 2015(ObservationalStudy); Dhalla, 2009(Observational Study)The ICSI Work Group did not review primary literature and instead reviewed the recommendations fromthe relevant societies on the following topics (see specific section for the recommendations and ICSI workgroup’s decision on endorsement): Electrocardiogram testing Cardiovascular diseases Cardiovascular medications Preoperative fasting Prevention of endocarditis Insulin therapy regimens in diabetes mellitusReturn to Table of Contentswww.icsi.orgInstitute for Clinical Systems Improvement9
PerioperativeSixth Edition /January 2020ForewordIntroductionThe ICSI Perioperative Guideline has been enhanced to include a new section – Perioperative OpioidManagement – that was developed by a separate subgroup and reviewed and approved by the PerioperativeGuideline work group. The new section addresses the entire continuum of perioperative opioid management(preoperative, intraoperative and postoperative).The Perioperative Guideline addresses and includes recommendations on the following topics:Section 1: General Preoperative Management1. Preoperative Health Screening and Assessment2. Preoperative Testing (Electrocardiogram, Chest X-ray, Hemoglobin/Hematocrit, Potassium/Sodium,Creatinine, Pregnancy, Hemostasis, and Glucose in Nondiabetics)3. Sleep Apnea4. Nicotine Cessation5. Preparation for SurgerySection 2: Perioperative Management of Select Conditions6. Cardiovascular Considerations: Review of Select Recommendations from American College ofCardiology/American Heart Association Guidelines7. Prevention of Endocarditis: Endorsement of Recommendations from American College of Cardiology and American Heart Association Guidelines8. Anticoagulants/Antithrombotics9. Diabetes MellitusSection 3: Perioperative Opioid Management10. Preoperative Opioid Management11. Intraoperative Pain Management12. Postoperative Opioid Management13. Perioperative Considerations for Patients with Opioid Use Disorder (OUD)Return to Table of Contentswww.icsi.orgInstitute for Clinical Systems Improvement10
PerioperativeSixth Edition /January 2020ForewordScope and Target Population Adults (aged 18 years and older) undergoing elective surgery.Return to Table of ContentsAims1. Increase the percentage of surgical patients undergoing elective surgery who have preoperative healthscreening and assessment.2. Increase the percentage of surgical patients undergoing elective surgery who are smokers who havesmoking addressed prior to surgery.3. Increase the percentage of surgical patients undergoing elective surgery with any risk factor forobstructive sleep apnea (OSA) who are screened for OSA prior to surgery.4. Increase the percentage of surgical patients undergoing elective surgery who have education on preoperative hair removal, bathing, fasting and oral hygiene prior to surgery.Return to Table of ContentsImplementation Recommendations HighlightsThis section highlights general recommendations and tips on setting up organizational infrastructure toimplement the recommendations from this guideline. Refer to the section for more information.Return to Table of ContentsRelated ICSI Scientific Documents Pain: Assessment, Non-Opioid Treatment Approaches and Opioid ManagementReturn to Table of ContentsDefinitionsSurgical care team – includes surgeon, anesthesiologist, nursing staff, and opioid prescriber involved inpatient care.Primary care provider – a provider who performs preoperative health screening and assessment andconducts postoperative follow-up in primary care.Return to Table of Contentswww.icsi.orgInstitute for Clinical Systems Improvement11
PerioperativeSixth Edition /January 2020Annotations1. General Preoperative ManagementPreoperative Health Screening and AssessmentConsensus RecommendationA preoperative health screening and assessment that includes a focused medical history andappropriate physical examination should be completed for all patients undergoing a surgicalprocedure, regardless of setting (unless the procedure involves mild sedation, or local/topicalanesthesia).Benefit:Obtains current information on patient’s medical status to assess for medical conditions that could potentiallylead to adverse perioperative outcomes, and thus mitigate that risk.Harm:None.Benefit-Harms Assessment:Preoperative health screening and assessment is key to obtaining patient’s current medical status to helpclinicians determine if patient is at risk of adverse perioperative outcomes and to mitigate that risk.Relevant Resources:Fleisher, 2014 (Guideline); Apfelbaum, 2012b (Guideline)Preoperative health screening and assessment should be performed before all surgical procedures unless theprocedure involves mild sedation or a local/topical anesthesia. The goal is to identify and manage medicalconditions that may impact perioperative morbidity and mortality.Preoperative health screening and assessment should include a focused review of medical history and appropriate physical examination. Additional testing including laboratory, electrocardiogram (ECG) and furthercardiopulmonary evaluation should be based on medical history and physical exam and in consideration ofsurgical procedure risk for adverse cardiac event (see “Preoperative Testing” section for details).Specifically, focused medical history and physical examination should include (by the expert consensusof the ICSI work group): Medical historyIndication for surgical procedureAllergies and adverse reactions to medications (specify reaction type)Anesthesia related complications or adverse events (personal and family history)History of a difficult airway or intubationMedical history and active medical problemsSurgical historyCurrent medications, over-the-counter remedies, herbal and dietary supplementsImplantable devices (cardiac devices, spinal stimulator, pain pumps etc.)Return to Index TableReturn to Table of Contentswww.icsi.orgInstitute for Clinical Systems Improvement12
PerioperativeSixth Edition /January 2020AnnotationsFocused review of issues pertinent to the planned anesthesia and procedure: -Current status of pertinent known medical issues-Cardiac status-Pulmonary status-The ability to perform four or more METs-Personal or family history of abnormal bleeding and history/at risk for anemia-Pregnancy status-Smoking, alcohol history and illicit drugs-Risk factors for development of surgical site infection (e.g., smoking, diabetes, obesity, malnutrition, chronic skin disease)-Risk factors for development of venous thromboembolism (VTE). VTE is a common andpotentially fatal perioperative complication. All surgical patients should undergo risk assessmentfor the development of VTE and have appropriate measures taken to prevent both clotting andbleeding abnormalities in the perioperative period.-Chronic pain and/or chronic opioid use; plan for postoperative pain management-Discharge plan following surgery that includes social support-Need for assistive devices following surgery (e.g., walker, hospital bed)Physical examinationWeight, heightVital signs – blood pressure, pulse (rate and regularity), respiratory rateCardiovascular examPulmonary examOther exams pertinent to surgical procedure and planned anesthesia such as:-Skin exam for signs of infection-Neurologic exam-Musculoskeletal-Airway exam including dentitionPrimary care provider communication with the surgical teamThe primary care provider should provide pertinent information to the anesthesiologist and surgeon on resultsof preoperative health screening and assessment in advance of anticipated day of scheduled procedure for allpatients undergoing elective surgery. The report should include a comprehensive assessment, any adjunctiveevaluation and specific recommendations. The ICSI work group acknowledges that regulatory agenciesmay have their own requirements for documentation of completion and timing of provision of information.In instances that a review of the current history and focused physical examination is required on the day ofsurgery prior to the procedure, it may be done by the provider performing the procedure.Return to Index TableReturn to Table of ContentsInstitute for Clinical Systems Improvementwww.icsi.org13
PerioperativeSixth Edition /January 2020AnnotationsPerioperative medication managementEnsure medication reconciliation, preoperatively. Navigating the topic of medications to stop or continuein the perioperative period can be complicated, especially as new medications come to market frequently.Working with a pharmacist to help develop and implement perioperative plans regarding medication management (medications to stop or continue) can be beneficial. The pharmacist can also perform medicationreconciliation, guide medications decisions and oversee medication dispensing.Return to Index TableReturn to Table of ContentsPreoperative TestingRecommendationQuality of EvidenceDo not routinely test all patients undergoing elective noncardiacsurgery.Quality of Evidence: LowThe need for testing should be guided by individual patient’sclinical risk factors (based on medical history and physicalexamination) and the risk of major adverse cardiac event(morbidity or mortality) associated with the planned procedure.Strength of Recommendation: StrongBenefit: Ensures only tests of value for patients who need it are performed. Decreases unnecessary perioperative costs for both patients and the health care system.Harm: A possibility of missing an important diagnosis.Benefit-Harms Assessment:Given the low likelihood that routine testing of healthy, asymptomatic patients will uncover issues that mightlead to adverse outcomes during perioperative period, only those patients who would benefit from additionaltesting should undergo it.Relevant Resources:Keay, 2019 (Systematic Review); Johansson, 2013 (Systematic Review); Munro, 1997 (Systematic Review)A 1997 systematic review of case series studies found no evidence to support routine preoperative tests(chest X-ray, electrocardiogram, hemostasis, blood counts, hemoglobin, potassium, creatinine, glucose andurine testing for pregnancy) in healthy, asymptomatic adults. Very few patients went on to have a changein management of the condition prior to surgery. (Munro, 1997)A systematic review of three randomized trials and 98 cohort studies found no evidence that preoperativetesting is beneficial in healthy adults undergoing noncardiac surgery. (Johansson, 2013)Large studies have found no evidence to support routine testing in low risk surgeries such as cataract surgery.A systematic review of three randomized controlled trials including 21,531 cataract surgery patients foundroutine preoperative medical testing did not reduce the risk of intraoperative or postoperative ocular adverseevents when compared to selective or no testing. (Keay, 2019)The need for preoperative testing should be guided by preoperative screening and assessment of clinical riskfactors based on patient’s pertinent medical history and physical exam, and in consideration of risk of majoradverse cardiac event (morbidity or mortality) associated with the planned procedure. Consultation withthe surgeon or proceduralist may be necessary to clarify relative procedural risk for the planned procedure.Return to Index TableReturn to Table of Contentswww.icsi.orgInstitute for Clinical Systems Improvement14
PerioperativeSixth Edition /January 2020AnnotationsTo help stratify surgical procedure risk, the American College of Cardiology (ACC)/American Heart Association (AHA) estimates the combined surgical and patient characteristics predict a risk of a major adversecardiac event (MACE) of death or myocardial infarction of 1% in low-risk surgeries Procedures with arisk of MACE of 1% are considered elevated risk. (Fleisher, 2014)There is some evidence that older age may be a factor in increasing the risk of adverse cardiac event duringsurgery depending on the type of surgery. An analysis of 2,853 procedures found inpatient mortality rate forhigh-risk procedures in patients 65 years and older was double the rate of patients younger than 65 years.(Schwarze, 2015)To guide perioperative mortality risk determination, the 2014 ACC/AHA Guideline on PerioperativeCardiovascular Evaluation and Management of Patients Undergoing Noncardiac Surgery recommends theuse of a validated risk prediction tool to predict the risk of perioperative major adverse cardiac event inpatients undergoing noncardiac surgery. (Fleisher, 2014) Risk calculators may include the Revised CardiacRisk Index, American College of Surgeons National Surgical Quality Improvement Program (NSQIP)Myocardial Infarction and Cardiac Arrest (MICA), and American College of Surgeons NSQIP SurgicalRisk Calculator. (Fleisher, 2014)Return to Index TableReturn to Table of ContentsElectrocardiogramCardiac arrhythmias and conduction disturbances are common findings in the perioperative period. However,limited evidence does not support routine testing in healthy, asymptomatic individuals. A 1997 systematicreview of case series studies in healthy and asymptomatic adults found routine preoperative electrocardiograms were abnormal in 4.6-31.7% of cases (with the proportion of abnormal tests rising with age andworsening physical status) and led to a change of management in 0-2.2% of patients with unknown effect onpatient outcomes. (Munro, 1997) A literature search by the ICSI Work Group did not find any new studieson relationship of preoperative electrocardiogram testing to perioperative mortality and morbidity outcomes.The ICSI work group AGREES with the 2014 ACC/AHA Guideline on Perioperative CardiovascularEvaluation and Management of Patients Undergoing Noncardiac Surgery recommendation on preoperative electrocardiogram (ECG). (Fleisher, 2014): Routine electrocardiogram is not useful for asymptomatic patients undergoing low-risk surgicalprocedures. Electrocardiogram is reasonable in patients with known coronary heart disease, significantarrhythmia, peripheral arterial disease or other structural heart disease, except for those undergoinglow-risk surgery.Return to Index TableReturn to Table of Contentswww.icsi.orgInstitute for Clinical Systems Improvement15
PerioperativeSixth Edition /January 2020AnnotationsChest X-rayRecommendationQuality of EvidenceDo not routinely perform chest X-rays preoperatively unlessindicated by the review of medical history and physicalexamination.Quality of Evidence: LowStrength of Recommendation: StrongBenefit: Ensures only tests of value for patients who need it are performed. Decreases unnecessary perioperative costs for both patients and the health care system.Harm: A possibility of missing an important diagnosis.Benefit-Harms Assessment:Given t
Review); Johansson, 2013 (Systematic Review); Munro, 1997 (Systematic Review) Chest X-ray Low Do not routinely perform chest X-rays preoperatively unless indicated by the review of medical history and physical examination. Strong Johansson, 2013 (Systematic Review); Joo, 2005 (Systematic Review) Hemoglobin/ Hematocrit Testing