Transcription
HCC CodingThe Risk Adjustment ProgramDATE: January 2021PRESENTED BY: Monique Vanderhoof, RHIT, CCA, CPC, CRC
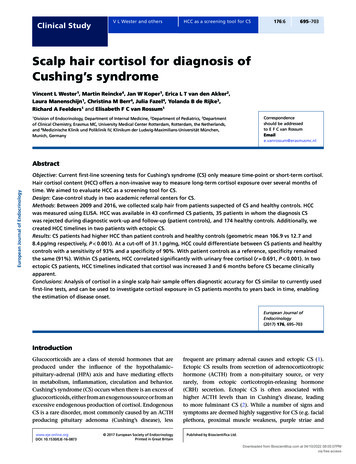
What is Risk Adjustment? Began as part of The Balanced Budget Act in 1997 Payments to health plans and provider groupsbased on a patient’s health status anddemographics. CMS and HHS pay more per month for patientswith a higher disease burden– This is to offset the cost of providing care2
HCC Basics3 HCC stands for Hierarchical Condition Category. An HCC is assigned to a patient based on the ICD- 10-CMcodes submitted on claims throughout the calendar year. Over 9,600 diagnoses fall into different “chronic conditionbuckets.” HCC’s are additive – meaning they are added together tocreate the overall risk score for a patient. The risk score associated with HCC’s resets every year (i.e.,January 1) Not all diagnoses are HCC’s but most chronic conditions are(i.e., DM, CHF, AFIB, etc.). CMS and some insurers pay more per month for patientswith a higher disease burden.
Impact of Annual CaptureFEW Chronic ConditionsCodedSOME Chronic ConditionsCodedALL Chronic ConditionsCoded76 year old female0.43776 year old female0.43776 year old female0.437Medicaid eligible0.151Medicaid eligible0.151Medicaid eligible0.151PVD (I73.9, HCC 108)0.298PVD (I73.9, HCC 108)0.298PVD (I73.9, HCC 108)0.298DM not coded (no HCC)0.0DM (E11.9, HCC 19)0.118DM with PVD (E11.51, HCC18)0.368CHF not coded (no HCC)0.0CHF not coded (no HCC)0.0CHF (I50.9, HCC 85)0.323No interaction0.0No interaction0.0Interaction (DM CHF)0.182Raw RAF Score0.886Raw RAF Score1.004Raw RAF Score1.759Little ReimbursementMore ReimbursementWe are somewhere in-betweenhere4Max ReimbursementWe want to behere!
What is an HCC? HCCs are added to create a risk score for apatient from ALL Face-to-Face visits with an“acceptable provider type”– Inpatient, Outpatient, Observation, ED, Clinic Greater than 40% of HCCs are not CCs or MCCs– Complete coding of all documented diagnosesis important!5
Risk Adjustment ScoringEach HCC category has a series of ICD-10-CM codes thatmap to it.Example :Provider assessment:Pt with Type 2 diabetes with CKD, stage 4Coding:Type 2 diabetes with CKD – E11.22 HCC 18CKD, stage 4 – N18.4 HCC 1377
HCC Model List8
HCC Hierarchy (Trumping) Trumping means to excel, surpass or supersedein rank, value or importance In HCC risk score calculation the most significantconditions trump others in the same categoryHCC Category179HCC DescriptionDiabetes with Acute ComplicationsRisk Score Value0.36818Diabetes with Chronic Complication0.36819Diabetes without Complications0.118
Why are they Important? Risk Adjustment Factor (RAF) scores help drivepayments for risk based contracts, andgovernment based programs. Patient complexity scores drive qualityassessments1010 Some here at OHSU:– OHSU Health– Moda Beacon– Cambia Bridgespan– Medicare Advantage– CPC – Oncology Care Model (OCM)– Bundled Payments
Why OHSU?Audits demonstrated that OHSU was consistently underperforming on patient complexity measures (i.e., RAF Scores).This negatively impacts quality ratings and reimbursement for ourclinics.There are also concerns with clarity of documentation in theambulatory setting, which can affect patient care.Goals:1. Improve patient care via more accurate representation of activemedical problems2. Integrate documentation efforts with growing caremanagement functionalities3. Receive appropriate reimbursement from year to year forrelative costs of care11
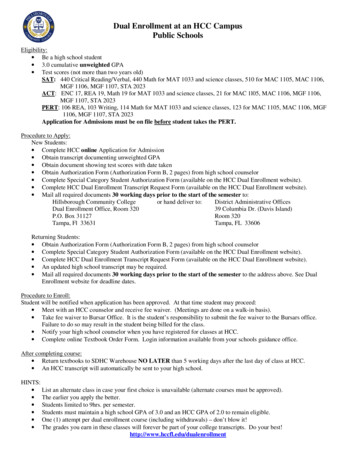
Current Work:All work now inclusive of coders and providers at Hillsboro and cialistsHCC ClinicalDocumentationImprovement4 HCCCertifiedCoders1.Prebill WQ’s(PC and Oncology)2.Provider query fordocumentationclarification3.Problem list updatesProviderEducatorEHR Toolsand DataAnalytics1. HCC audit tools based onbilling & claims data, CEMoniqueVanderhoof,HCC ProgramManager1 coderpositionvacant dueto budgetrestrictions1. Monthly strategymeetingsincluding OHSU,AH, HMC2. Epic tools: BPA SmartSets,Diagnosis Calculators, etc.EducationPopulationHealth3. Webi reports4. HCC BPA refinement1. Monthly/Quarterlyprovider meetings1. Direct Patient Scheduling forPC for HMC and OHSU2. 1:1 provider intensives2. Panel/Care CoordinatorStandard Work3. Coder centric education3. Incentives4. Specialty engagement4. HCC impact for VBCs &MSSP
HCC TeamTopic:1313Summary:Goal ofworkgroup/team: Accurately reflect the quality of care we provide Enable OHSU Health to compete effectively in value-based marketplaceCurrentwork/projectsunderway: Looking Ahead: Advancing partnership with Adventist and Hillsboro Medical Center Understanding the impact of HCCs for VBCs such as the IDS and MSSP Defining HCC goals and targets for FY21Barriers: Provider/clinic buy-in difficult to obtain without aligned incentives Dedicated staff to support MWVs and outreach Problem list is the foundation of many epic driven toolsRefining epic tools to aid providers in real time (BPAs & Diagnoses calculators)Pre-bill claim review by HCC coders to confirm accurate coding/documentationWebi reports and Epic registries to understand baseline and opportunityOngoing provider and coder educationPre-bill WQ in OncologyPlans to work with Neurology, Pre-op, Pediatrics
Moving forwardProjects Underway: Refining epic tools to aid providers in real time (BPAs & Diagnosescalculators/Preference Lists) Addition and refinement of HHS HCCs Defining HCC priorities and aligning across OHSU Health System Problem List update by HCC coders Working to better understand HCC impact across system Ongoing work with: neurology(OHSU and HMC), pre-op(OHSU), cardiology(HMC), oncology(OHSU andHMC), endocrinology(HMC) Plans to expand work to Pediatrics early 2021Current Barriers: Provider/clinic buy-in difficult to obtain without aligned incentives Dedicated staff to support MWVs and outreach Problem list is the foundation of many epic driven tools Payer/Epic reporting variances Resource variation across OHSU, HMC, and AH AH Epic system differences
Diagnosis CalculatorHow can we use tools we already have to help providers code better?New diagnoses preference lists were created to identify the correctdiagnosis codes when documenting a visit. The tools assist providers to meetICD-10 coding requirements and accurately capture patient’s complexityscores.Old VersionNew Version
HCC Best Practice Alert16
Epic Workbench Report
Pre-bill Review Work Queue 18HCC coding team is reviewing all primary care charges fromrisk based payers. This ensures all ICD-10 codes are accuratebased on documentation before they are sent to insurancecompanies.
Outcomes CMS average score 1.0Patient populationrepresented here 582 Overall scores increased 13% between 2017 and 2018, andanother 7% in 2019 What if these lives were in a capitated arrangement?– The 18-19 increase would equate to 419,056 ( 59.00 PMPM1919rate using 2021 CMS rate book)
Focus onCorrect Coding &Documentation
Education Provider meetings (group education) quarterly 1:1 provider education Monthly coder education21
Correct coding & documentationIn order to capture HCC’s appropriately providers must: Code all documented conditions that exist at the time ofthe encounter and require or affect patient care,treatment or management Accurately document all chronic diseases, manifestations,and status codes at least once each year Document and code chronic conditions being managedby specialist Document using M.E.A.T. concepts22
M.E.A.T.Documentation must prove that the patient’scondition(s) were:MonitoredEvaluatedAddressedTreated Only one element of M.E.A.T is required. Twoor three are better!23
M.E.A.T.24
Correct coding & documentation A simple list of problems or diagnoses is notacceptable documentation– For RADV purposes a problems list must showevaluation and treatment for each condition thatrelates to a diagnosis code*per Risk Adjustment for Medicare Advantage Organizations Participant Guide A problem list may be useful to initially gain anoverall clinical picture, but conditions that arecurrent must be supported by other documentation25
Correct coding & documentationOfficial ICD-10-CM guidelines state that accuratecoding cannot be achieved without clear, consistent,complete documentation in the medical record.Guidelines further instruct to code all documentedconditions that exist at the time of the encounter, andrequire or affect patient care, treatment ormanagement-26
Frequently overlooked HCC’sCHFAnginaAtrial FibrillationCOPDCompression FxSeizure DisorderPsychosesRheumatoid ArthritisPolymyalgiaRheumatica (PMR) History of Amputation Transplant StatusDialysis enia, etc.Bowel ObstructionDiabetes andcomplicationsMetastasesVentilator dependence
Questions?THANK YOU!!!HCC Program Manager:Monique Vanderhoof, RHIT, CPC, CCA, CRCvandermo@ohsu.eduNext session – February 16, 2021Diagnosis Coding for Wellness Exams
Thank You
Correct coding & documentation Official ICD-10-CM guidelines state that accurate coding cannot be achieved without clear, consistent, complete documentation in the medical record. Guidelines further instruct to code all documented conditions that exist at the time of the encounter, and require or affect patient care, treatment or management-