Transcription
Stop SmokingBehavioural SupportPractitionersHandbook
Tobacco control and smoking cessationUnderstanding the full range of activities that form a comprehensive tobacco controlprogramme, and how smoking cessation fits within this, will help you to work effectivelywith other agencies involved in tobacco control at local and national level.Local stop smoking services are part of a much wider tobacco control strategy that aims to:* Make smoking less attractive to young people;* Encourage and support as many smokers as possible to try to stop;* Make tobacco less affordable;* Reduce exposure to environmental tobacco smoke;* Prevent the tobacco industry from promoting its products;* Provide effective communications for tobacco control.In order for you to be able to provide accurate information to others, and better understandthe context within local stop smoking services operate, it is important you understandcurrent government policy on tobacco control.Tobacco control strategiesOne of Public Health England's priorities is to accelerate efforts to promote tobacco controland reduce the prevalence of smoking.The Public Health Outcomes Framework (PHOF) includes three specific tobacco relatedindicators:* Adult smoking prevalence;* Smoking prevalence amongst 15 year olds;* Smoking status of mothers at time of delivery.The Department of Health's strategy for tobacco control is called ‘Healthy Lives, HealthyPeople: A Tobacco Control Plan for England and was published in March 2011’.The plan had three key ambitions, which were to reduce smoking prevalence amongst:* Adults - to reduce prevalence from 21.2% to 18.5% or less by the end of 2015;* Young people - to bring regular smoking among 15 year olds down from 15% to 12% orless by the end of 2015;* Women who are pregnant - to reduce smoking prevalence from 14% to 11% or less by theend of 2015.Page 1
The strategy supports tobacco control in England across the six internationally recognisablestrands:* Stopping the promotion of tobacco;* Making tobacco products less desirable* Effective regulation of tobacco products;* Helping tobacco users to quit;* Reducing exposure to second hand smoke;* Effective communications for tobacco control.Parliament debated a new tobacco strategy in October 2015 and a new plan is awaited.The role of stop smoking servicesAlmost three quarters of smokers say they would like to quit. Over one third (39%) go on tomake a quit attempt each year but only a small proportion - about 5% - quit successfully.Smokers who stop smoking with specialist support and medication are up to four timesmore likely to successfully stop compared to smokers who stop without any form ofsupport. This means stop smoking services deliver life-saving interventions and play a role inhelping achieve the national tobacco control targets with regard to smoking prevalence.Marketing and recruitmentStop smoking services significantly improve quit rates, yet despite this most smokers still donot know what their local service can offer.Understanding the opportunities and challenges posed by the need to recruit smokers intotreatment will help you to inform the development of recruitment strategies in your areaand contribute to the set-up and monitoring of local referral systems.Formal referral systems for key settings (such as primary and secondary care) will ensurethat smokers are routinely recruited from the broader health and social care system.Informal self-referral systems should also be in place to encourage, and make it easy, forsmokers to get help to stop.It is important that services evaluate the effectiveness and cost-effectiveness of innovativemethods of generating referrals, such as stop smoking shops and outreach campaigns.National marketing and communications campaigns are effective at getting more people touse the local stop smoking services.Strategies for promoting stop smoking services should be based on local intelligencewherever possible, but will be enhanced by integration with national and regionalcampaigns.Page 2
Cost effectivenessThe work of stop smoking practitioners has great value to the NHS, the wider economy andto the general public.Smoking cessation interventions have been shown to be one of the most cost-effective of alllife-saving treatments provided within healthcare systems - savings have been calculated tobe somewhere in the region of 1,000 per life year gained, compared with more than 15,000 for the average life-saving treatment.The current level of tobacco use is estimated to cost the NHS around 2.7 billion every year.Understanding these costs to society, and the benefits of stop smoking services, should helpyou to persuade others of the importance of local stop smoking services within the contextof the local health economy.Smoking in the populationUnderstanding who smokes, what effect smoking has, why people smoke, and how best tohelp them stop, is central to the role of a stop smoking practitioner as this provides thecontext for your professional practice.Key facts* In December 2013 smoking prevalence in England was 19.5%. Latest figures (September2016) show it has fallen to 18.4%;* Prevalence differs according to age, socio-economic group and ethnicity;* Smoking is declining at the same rate across all socio-economic groups; although until veryrecently the drop in smoking rates among lower-income groups was much slower.Demographics and prevalenceIt is important to have an understanding of smoking demographics and prevalence because:* It helps when it comes to understanding smokers' chances of quitting, and tailoring theway that you interact with them;* If you work in an area with a specific population of smokers, it is important to understandwhat impact this may have on referral and attendance to stop smoking services.Smoking and genderAlthough teenage girls are more likely to smoke than teenage boys, by the time theybecome adults smoking prevalence is slightly higher in men than in women.Page 3
A lot of people think women find it harder to stop smoking than men, this is not normallytrue. Men and women find it equally difficult to quit smoking. However, women are morelikely than men to access stop smoking services.Although women report smoking for weight control more than men and are concernedabout weight gain once they quit, it is not a common reason for relapse back to smokingonce they make a quit attempt.Smoking and ageStudies have consistently shown that, in the UK:* Smoking prevalence peaks in the mid-twenties;* Younger smokers are more likely to try to stop smoking but less likely to succeed;* Older smokers are more likely to have switched to lower tar cigarettes.Smoking and ethnicitySmoking prevalence is not uniform across all ethnic groups: smoking prevalence is muchhigher in Bangladeshi men, and slightly higher in Pakistani men than 'white British' men.Smoking prevalence is much lower in women of all minority ethnic groups than 'whiteBritish' women.Use of smokeless tobacco such as Paan is common among people of South Asian origin.Use of waterpipes (shisha or hooka) is also common among people of South Asian origin, inpeople of Arabic origin and is growing amongst young people irrespective of their ethnicity.Asian and African-Caribbean smokers use the local stop smoking services about as much as'white British' smokers.Smoking and socio-economic groupSmoking prevalence is higher in more deprived socio-economic groups: 26% for routine andmanual occupations compared with 14% in managerial and professional groups.Smoking is the biggest single cause of inequalities in death rates between rich and poor inthe UK.It is extremely important to understand that people from more deprived backgrounds donot lack motivation to stop or make less quit attempts than more affluent smokers, but mayneed more help to quit.Page 4
Quit attemptsAbout 4 out of every 10 smokers (39%) have tried to quit in the previous 12 months, butonly about 5% of these succeed.Over half of all smokers (52%) say that they are 'cutting down' on their smoking.There is no difference between 'lighter' (less dependent) and 'heavier' (more dependent)smokers in their attempts to stop, but less dependent smokers are more likely to succeed.The main times for trying to quit are January (because of New Year resolutions), March(because of No Smoking Day) and, since 2012, October (because of Stoptober).These seasonal fluctuations impact upon the number of smokers attending local stopsmoking services.Smoking and healthSmoking is the single most important preventable cause of death and illness.It causes over 100,000 deaths per year in the UK, 5 million worldwide, and results in thepremature death of half of smokers who do not manage to stop.Smoking is the cause of long-term illness and disability in many smokers, including thosethat ultimately die from something else other than their smoking.The main causes of death attributable to smoking are:* Cancer;* Cardiovascular disease;* Lung disease.CancerIn the UK, smoking causes over 37,000 people to die from cancer each year, 34,000 of thesefrom lung cancer.The risk of lung cancer is 15 times greater for a smoker than a non-smoker. The riskaccumulates over time and is directly related to daily cigarette consumption and how longsomeone has been smoking.About one in eight smokers who do not quit will die of lung cancer.As carcinogens in cigarette smoke are ingested, dispersed and eliminated throughout thebody, smoking is linked to a large number of cancers other than lung cancer, including:* Throat and mouth cancer;* Bladder cancer;Page 5
* Kidney cancer;* Stomach cancer;* Pancreatic cancer.Cardiovascular disease (CVD)Cardiovascular disease (such as heart attacks and strokes) account for over one-quarter ofall smoking-related deaths.The average smoker has approximately twice the risk of developing heart diseaseprematurely compared to someone who has never smoked, and even light smokers have asubstantially increased risk of cardiovascular disease.Chronic Obstructive Pulmonary Disease (COPD)The term COPD encompasses chronic bronchitis and emphysema. In both diseases the lungslose their capacity to transfer oxygen to the bloodstream.About 23,000 people die from COPD as a consequence of smoking, accounting for over onefifth of all smoking-related deaths each year.COPD is easy to detect at an early stage through spirometry (a test to measure lungfunction), and its progress can be slowed dramatically by stopping smoking.There are numerous other diseases and conditions, many of which are fatal, caused or madeworse by smoking. A stop smoking practitioner needs to be able to inform smokers aboutthese other health consequences of smoking:* Age-related hearing loss;* Crohn’s disease and inflammatory bowel disease;* Type 2 diabetes;* Osteoporosis;* Smokers undergoing surgery are at an increased risk of complications from anaesthesia;* Smokers are more vulnerable to post-surgical complications and delayed wound healing.Environmental tobacco smokeIt is essential that smokers have accurate information on how their smoking can impact onthe health of others.There is good evidence to show that exposure to environmental tobacco smoke, also knownas 'second-hand smoke' or 'passive smoking', increases the risk of:* respiratory disease;* lung cancer;* coronary heart disease.Page 6
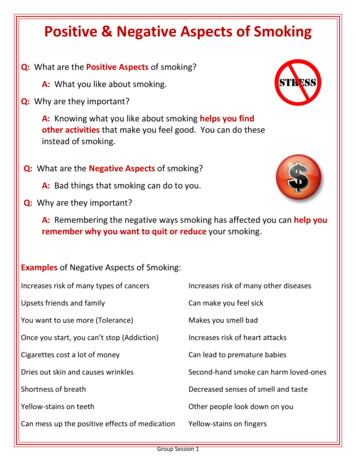
Exposure to second-hand smoke in pregnancy has been shown to reduce birth weight whichcan have serious consequences for the baby's health and childhood development.Babies and children who live with parents who smoke have a greater risk of respiratoryillness, ear disease and cot death (Sudden Unexplained Death in Infancy); plus they aremore likely to grow up to be smokers themselves.'Protective effects' of smokingSmokers may have heard media reports about the 'positive effects' of smoking, and it isimportant to be able to confidently address any false beliefs.There is actually some evidence to suggest that cigarette smoking may reduce the risk ofcertain conditions:* Pre-eclampsia;* Morning sickness during pregnancy;* Ulcerative colitis;* Parkinson’s disease.However, smoking does not completely protect against these conditions.It is also important to inform smokers that the health benefits of stopping smoking faroutweigh the loss of any 'protective effects' which may occur.Although many people have heard that smoking is protective against Alzheimer’s disease,this is not true.Health benefits of stopping smokingIt can be motivating for smokers to have information on the benefits of stopping, and it isimportant to communicate to smokers that quitting is the best thing they can do for theircurrent and future health.It is important for young smokers to realise that they have most to gain by stopping now.Stopping smoking increases life expectancy at every age but the earlier the smoker stops thebetter; quitting at age 35 adds an average of 10 years, while quitting at 65 adds 3 years oflife.Stopping smoking at any age will lead to improvements in physical and mental health.Key facts that you can tell smokers include:* The risk of lung cancer stops increasing when smokers quit;Page 7
* The increased risk of heart disease diminishes by 50% within the first year of stopping;* The rate of progression for COPD is drastically slowed once a smoker stops smoking;* Ex-smokers report being healthier, happier and having greater life satisfaction thansmokers;* The average smoker saves over 1,500 per year if they quit.Special PopulationsThe special populations covered in this training course are smokers who:* Are pregnant;* Have mental health problems;* Are drug and alcohol dependent.Pregnancy and smokingSmoking makes it harder to conceive, irrespective of which partner smokes.In men, smoking is linked to reduced sperm count, less mobile sperm and higher incidenceof impotence. In women, smoking is linked with hormonal changes that reduce thelikelihood of pregnancy.Smoking can reduce the likelihood of success of assisted reproductive techniques (e.g., invitro fertilization, IVF).It is essential to be aware of the special circumstances that arise with pregnant smokerswhen determining how best to recruit them to local stop smoking services, and how to bestsupport them to successfully stop smoking.One in eight (12%) mothers reported that they continued to smoke throughout theirpregnancy (down from 17% in 2005). About 25% of women who smoke succeed in quittingwhen they learn they are pregnant, but many more would like to stop.Teenage smokers and smokers from deprived backgrounds are far less likely to succeed instopping despite being motivated to stop smoking.The percentage of women who stop in their first pregnancy is greater than the percentagestopping in later pregnancies.Women can be reluctant to admit to being a smoker when asked by health professionals, fora range of reasons including fear of social stigma.All pregnant smokers should be made aware that smoking increases the risk of bothmiscarriage and stillbirth.Page 8
Babies born to mothers who smoke are more likely to be born prematurely and with lowbirth weight, which itself causes a number of problems.Babies born to mothers who smoke are twice as likely to die from cot death (SuddenUnexplained Death in Infancy) as babies born to non-smokers.Children born to mothers who smoke are more likely to have:* Behavioural problems;* Learning difficulties;* Respiratory problems.Smoking and mental health problemsSmoking prevalence is higher amongst people with mental health problems than it is in thegeneral population, and is particularly high amongst those with severe mental illness.There has been reluctance from health professionals to address smoking in this group.Studies show desire to stop smoking is just as high amongst people with mental healthproblems as in the general population, and that stopping smoking does not worsen mentalhealth.However, these smokers may need higher levels of support to successfully stop.Smoking and mood disordersSmoking prevalence is higher in people with anxiety and depression.Anxiety levels typically go down when people stop but depression usually remains at thesame level.The vast majority of smokers' report being 'happier' after they have stopped but a fewreport being less happy and these may need additional and more intensive support so thatyou can reassure smokers that stopping smoking won’t worsen their condition, but will infact improve it.You need to be vigilant in monitoring the minority of people who become more miserablewhen they stop smoking and see what long-term help they might need.The majority of people with schizophrenia and other psychotic disorders smoke, and in mostcases they are very heavy smokers withgreatly increased risk of dying from a smoking-related disorder. There is no evidence toshow that smoking helps with psychotic symptoms.Smoking (mostly through the hydrocarbon agents in cigarette smoke, not nicotine)stimulates a liver enzyme responsible for metabolising drugs in the body which results in thefaster clearance of a number of medications including:Page 9
* antipsychotics;* antidepressants;* anxiolytics.This means that smokers may need higher doses of these drugs than non-smokers.Stopping smoking can therefore lead to the doses of some medications needing to bereduced to achieve the same drug level and therapeutic effect.It is essential to realise that there is no medical reason for people with psychotic illness tocontinue to smoke, and that in terms of encouragement to stop they should be treated likeany other smoker. However, there must be the additional understanding that the difficultiesthey face in stopping are greater.People with drug and alcohol dependenceSmoking rates are very high in people who have problematic use of drugs and/or alcohol.Smokers who are also dependent on drugs or alcohol can find it particularly hard to stopsmoking.There is evidence that stopping smoking does not make these other addictions worse, orlead those who have become drug or alcohol free to relapse.You need to be able to reassure people with drug and alcohol addictions that stoppingsmoking will not make their other addictions worse, but they may need additional andintensive support.NicotinePeople's susceptibility to nicotine, and their social and physical environments, both playcrucial roles in keeping them smoking.It is explained here in some detail because it is useful to be able to help smokers understandwhy they are addicted, and why it is difficult to quit smoking.How nicotine worksNicotine in cigarette smoke is a drug that mimics a naturally occurring chemical messengeror 'neurotransmitter' called acetylcholine which is present in many parts of the nervoussystem.Nicotine attaches itself to receptors on nerves in a part of the brain that is important incontrolling our motivation, called the ventral tegmental area. This causes the nerve cells tobecome more active, causing them to release dopamine at the other end of the nerve in anarea of the brain called the nucleus accumbens. This process is important in thedevelopment and maintenance of addiction.Page 10
Nicotine from cigarette smoke is rapidly absorbed through the large surface area of thelungs, this results in a nicotine 'hit' reaching the brain within a few seconds of each puff.Following each cigarette nicotine concentrations in the body fall rapidly, as it is metabolisedand excreted. The concentration falls by half every 90-120 minutes which means that after anight’s sleep most smokers have very little or no nicotine in the body.Awareness of how quickly nicotine concentrations fall in the body allows you to understandthe onset of withdrawal symptoms and why many smokers need to keep topping up theirnicotine levels by smoking regularly throughout the day.It also explains the significance of knowing how long after waking they have their firstcigarette in the morning is as a measure of nicotine dependence.On average, smokers get just over 1mg of nicotine from each cigarette but the dose variesconsiderably between smokers. If a cigarette is smoked as hard as possible, a smoker canget up to 6mg nicotine into their system.It is important that you can explain this to smokers to highlight the inaccuracies of cigarettelabelling of products such as 'lighter' brands, and when discussing how NRT works.Dopamine is released into the brain by the action of nicotine on neuro-receptors, and actsas a 'chemical reward' or 'teaching signal'. The brain naturally seeks out more of this'chemical reward' and does so by motivating us to repeat the behaviour that led to thereward - in this case puffing on a cigarette.The dopamine mechanism also creates associations between the nicotine reward and cuessuch as:* Being with smokers;* Times when they would have previously smoked, such as sitting down after a meal;* Being under the influence of alcohol.This link is completely unconscious and undermines the smoker’s ability to make rationalchoices about the behaviour.The rapid excretion of nicotine from the body causes withdrawal symptoms which arequickly relieved by smoking, and this too reinforces their dependence.Smoking causes lasting changes to the brain.This means that smokers are used to regular doses of nicotine and when there is no, or less,nicotine in the brain, dopamine levels in the nucleus acumbens are abnormally low. Thiscreates what is known as an 'abnormal drive state' (much like hunger for food), but in thiscase the target is nicotine.It is experienced as a kind of gnawing hunger for a cigarette or ‘craving’.Page 11
This is in addition to the cravings triggered by smoking cues.Smokers have to 'learn' how to smoke because for many, at first it is usually an unpleasantexperience with feelings of nausea and giddiness.However, repeating smoking becomes a habit. Nicotine taps into a part of the brain thatlearns automatic associations between triggers and actions – the part that learns habits.This means that smokers get automatic impulses to smoke in situations in which they wouldnormally light up, called 'cues'.Being in a situation with other smokers, or experiencing events that have previously beenassociated with smoking, are high risk times for quitters.When smokers encounter a cue, they have the impulse to reach for a cigarette. If theyconsciously resist this, they experience the impulse as an 'urge' to smoke.Most smokers will experience unpleasant effects on their mood and physical wellbeing afterthey quit and this will contribute to their strong desire to smokeThese include:* Depressed mood;* Irritability;* Restlessness;* Difficulty concentrating;* Increased appetite;* Cough;* Constipation;* Weight gain;* Mouth ulcers.Most of these can be helped by using one of the stop smoking medications, although theyare unlikely to be eliminated completely.These withdrawal symptoms mostly last a few weeks, but increased appetite lasts longer,and some weight gain is usually permanent.Behavioural SupportResearch clearly shows that face-to-face behavioural support given over multiple sessionsdoubles the chances of a successful quit attempt.When this support is combined with a smoking cessation medication (NRT, bupropion orvarenicline), the chances of a successful quit attempt are doubled again.Page 12
This means that a smoker who attends a stop smoking service, and uses medication asadvised, has a four times greater chance of stopping smoking than someone going coldturkey in an unsupported attempt.It is this combination of behavioural support, and effective medication that gives the smokerthe best chance of success at stopping.‘Pro-active’ telephone support where the stop smoking specialist calls the smoker accordingto a pre-planned schedule, can also be helpful and can enhance the effect of face-to-facesupport.Behavioural support works by increasing smokers' motivation not to smoke and reducingmotivation to smoke; at the same time building on their capacity and skills to exercise selfcontrol and optimising their medication use.There are a number of evidence-based specific behaviour change techniques (BCTs) involvedin the delivery of effective behavioural support.BCTs, the things that you say and do with smokers, are effective interventions to improvesmokers' chances of quitting.The behaviour change techniques that have been shown to be the most important are:* Establishing a good rapport;* Making sure they have a realistic expectation of stop smoking medications, use thesemedications properly and that they are aware of any potential side effects;* Making sure the smoker knows what to expect in terms of cravings and withdrawalsymptoms;* Helping them to change their routine to avoid smoking;* Using CO monitoring as a motivational tool;*Stressing the importance of the ‘not a puff’ rule and gaining commitment from them;* Supporting them through their quit attempt and giving praise for not smoking;Group supportWanting approval from our peers is a very important motive for a lot of people, andsmokers attending stop smoking groups report that thinking about what they would say tothe group if they smoked was the thing that stopped them from having a cigarette.In order to maximise this effect it is important to make sure that smokers are orientedtowards the group and not towards the facilitator.Group-based support using a 'closed group' format, where the whole group starts togetherand has the same quit date, has the highest success rates of all forms of behaviouralsupport.Page 13
'Rolling groups' are where people join the group at different stages in their quit attempt butthere is little evidence of their effectiveness.For groups to be effective they need to start with a fairly large number of people, ideally15 and certainly more than 10.This requires a large enough catchment area and a strong recruitment drive. It also requiresyou to be experienced in group support and to know the advantages so that you canovercome people's natural resistance to the idea of a group.It is also important to screen out people who are not suitable because they would adverselyaffect the group process.MedicationsAs a stop smoking practitioner you need to help smokers make an informed choice aboutthe medications available to them and to be able to answer any questions or concerns theymight have.The NCSCT course focuses on those smoking cessation medications approved by theNational Institute for Health and Care Excellence (NICE) to help people stop smoking.We have supplied sufficient information here to allow you to complete the NCSCTassessment but have used our local guidance supporting our contracts for behaviouralsupport and stop smoking medicines (see following pages).Page 14
Smoking Cessation Guidelines - Provision of Stop Smoking MedicinesGeneral Prescribing PointsThe vast majority of trials of smoking cessation drugs include motivated subjects only where intensebehavioural support is available. In order to achieve the best quit rates smokers should receive counsellingfrom smoking cessation behavioural support providers. Intensity of counselling is strongly linked to quit ratesso patients should not simply be issued with pharmacotherapy. If a patient has made a successful quit attemptusing Nicotine Replacement Therapy (NRT), but then relapsed, this is not an indication to try a different drug.Therapy to aid smoking cessation should be chosen according to the smoker’s likely compliance, availability ofcounselling and support, previous experience of smoking cessation aids, contra-indications, adverse effects,patient co-morbidities and the smoker’s preferences.Smoking cessation therapies should not be added to the repeat prescription in primary care.All healthcare professionals must exercise their own professional judgement when using clinical guidance.However any decision to vary from the guideline should be documented to include the reason for variance andthe subsequent action taken.It is recognised that any risks that may be associated with NRT are substantially outweighed by the wellestablished dangers of continued smoking.This guidance therefore focuses on the provision of various options for pharmacotherapy for patients.CONTENTSSECTIONCONTENTSection 1Provision of NRT Pharmacotherapy17Section 2Description of Formulary Options20Section 3Information on the use of varenicline and bupropion26Section 4Characteristics of staff providing behavioural support/pharmacotherapyservices27Appendix 1NRT Pharmacotherapy options for primary care based providers28Page 15PAGE
Contribution ListKey individuals involved in developing the documentNameDesignationAlison RogersHerefordshire CCG Governance PharmacistDr Arif MahmoodConsultant Public Health Herefordshire CouncilProfessor Rod ThompsonInterim Director of Public Health Herefordshire CouncilDr Paul HarrisHerefordshire CCG Primary Care Prescribing LeadCirculated for comments to:NameDateHerefordshire CCG Medicines OptimisationGroup8 February 2016Wye Valley NHS TrustApril 2016 to discuss Formulary within Wye Valley NHSTrustFormulary Working GroupRatified by:NameDateProfessor Rod Thompson11 February 2016Director of Public HealthHerefordshire CouncilSigned:Change HistoryVersion and dateChange detailsFinal Version 1.1 11 February 2016IA EditApproval Committee Name:Reformat and removal of reference to QuitPage 16
Section 1. Provision of NRT PharmacotherapyClinical Indication towhich this guidanceappliesAs an aid to treating tobacco dependence in:Clients receiving specialist advice and support from healthprofessionals e.g. community pharmacies, GP practice staff andnon- clinical providers of stop smoking services.Providers other than community pharmacists will provide NRTrecommendations on a Herefordshire Council voucher system forcommunity pharmacy professional oversight and supply of aproduct from a locally agreed formularyCriteria for inclusion Tobacco users, aged 12 years and over, identified assufficiently motivated t
Smokers who stop smoking with specialist support and medication are up to four times more likely to successfully stop compared to smokers who stop without any form of support. This means stop smoking services deliver life-saving interventions and play a role in helping achieve the national tobacco control targets with regard to smoking prevalence.