Transcription
STERILE DRAPING:FUNDAMENTAL PRACTICES1963
1963STERILE DRAPING:FUNDAMENTAL PRACTICESSTUDY GUIDEDisclaimerAORN and its logo are registered trademarks of AORN, Inc. AORN does not endorse any commercial company’s products orservices. Although all commercial products in this course are expected to conform to professional medical/nursing standards,inclusion in this course does not constitute a guarantee or endorsement by AORN of the quality or value of such products or ofthe claims made by the manufacturers.No responsibility is assumed by AORN, Inc, for any injury and/or damage to persons or property as a matter of product liability,negligence or otherwise, or from any use or operation of any standards, recommended practices, methods, products, instructions,or ideas contained in the material herein. Because of rapid advances in the health care sciences in particular, independentverification of diagnoses, medication dosages, and individualized care and treatment should be made. The material containedherein is not intended to be a substitute for the exercise of professional medical or nursing judgment.The content in this publication is provided on an “as is” basis. TO THE FULLEST EXTENT PERMITTED BY LAW, AORN,INC, DISCLAIMS ALL WARRANTIES, EITHER EXPRESS OR IMPLIED, STATUTORY OR OTHERWISE, INCLUDINGBUT NOT LIMITED TO THE IMPLIED WARRANTIES OF MERCHANTABILITY, NONINFRINGEMENT OF THIRDPARTIES’ RIGHTS, AND FITNESS FOR A PARTICULAR PURPOSE.This publication may be photocopied for noncommercial purposes of scientific use or educational advancement. The followingcredit line must appear on the front page of the photocopied document:Reprinted with permission from The Association of periOperative Registered Nurses, Inc.STERILE DRAPING: FUNDAMENTAL PRACTICESCopyright 2013 AORN, Inc.All rights reserved by AORN, Inc.2170 South Parker Road, Suite 400Denver, CO 80231-5711(800) 755-2676www.aorn.orgVideo produced by Cine-Med, Inc127 Main Street NorthWoodbury, CT 06798Tel (203) 263-0006 Fax (203) 263-4839www.cine-med.com2
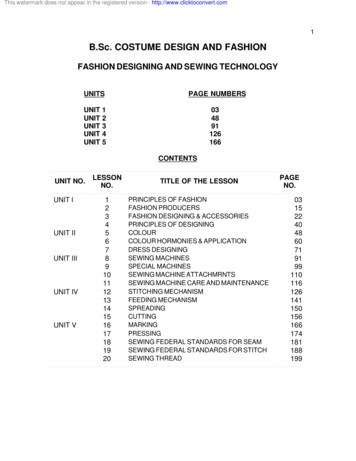
S TERILE D RAPING : F UNDAMENTAL P RACTICESSterile Draping:Fundamental PracticesTABLE OF CONTENTSPURPOSE/GOAL/OBJECTIVES.4OVERVIEW .5HISTORICAL REVIEW .5SELECTING DRAPING MATERIALS .5ESSENTIAL PRINCIPLES OF DRAPING.6USING DRAPES TO ESTABLISH A STERILE FIELD .8Laparotomy.8Draping equipment .8DRAPING FOR SPECIFIC OPERATIVE PROCEDURES.9Extremity Procedures .9Lithotomy Procedures.10Head and Face Procedures.11Robotic Procedures .11SUMMARY.12REFERENCES .13POST-TEST.14POST-TEST ANSWERS .163
S TERILE D RAPING : F UNDAMENTAL P RACTICESPURPOSE/GOALThe purpose of this study guide and companion video is to review techniques for sterile draping, which is a fundamental aspectof sterile technique.OBJECTIVESAfter viewing the video and completing the study guide, the participant will be able to:1.2.3.4.Explain the rationale for using sterile drapes to establish the sterile field.Describe methods to drape equipment located next to or within the sterile field.Discuss basic techniques for draping patients.Identify proper ways to drape patients for four types of surgical procedures.4
S TERILE D RAPING : F UNDAMENTAL P RACTICESOVERVIEWThis study guide reviews concepts and practices related tosterile surgical drapes and draping, which are fundamentalcomponents of sterile technique.The textile industry later began developing limitedperformance standards and methods to test products for barrierefficacy; however, manufacturers did not adapt or followconsistent protocols for these practices. Reusable drapes, inparticular, were tested with a variety of methods. Theseinconsistencies made it difficult to compare the quality andperformance of different products. In addition, as recently asthe 1980s, there were no standards for flammability or fibercontent, and numerous woven and nonwoven materialsremained on the market.3Surgical drapes are used to create a sterile field around thesurgical site and establish a physical barrier that reduces therisk of surgical site infections (SSIs) by decreasing themovement of microorganisms from unsterile to sterile areas.1AORN recommends that perioperative team members usesterile surgical drapes on the patient, OR furniture, andequipment that are to be included in the sterile field, and thatpersonnel handle surgical drapes in ways that preventcontamination.Recently, these problems have drawn additional scrutinybecause of increasing rates of bloodborne pathogen infections.These infections can be transmitted during surgery and otherinvasive procedures when products fail during surgery orwhen appropriate infection-prevention guidelines are notfollowed.Proper selection and correct use of sterile surgical drapes areessential practices for establishing and maintaining a sterilefield. Sterile drapes must be handled properly to optimize theirfunction and prevent contamination. They must also be placedcorrectly depending on the invasive procedure to beperformed.This guide first reviews basic principles of drape selection anduse, and then describes proper draping methods forlaparotomy, extremity surgery, lithotomy, and surgeriesrequiring facial exposure and robotic surgery.The American National Standards Institute, and theAssociation for the Advancement of Medical Instrumentationhave published a common system for classifying drapes andprotective apparel used in health care facilities, and have alsopublished labeling requirements for these items.4 Thisguidance is based on standardized testing that assesses liquidbarrier performance. The AORN recommendations emphasizethe importance of consistent classification and labeling ofsurgical drapes by manufacturers.HISTORICAL REVIEWSELECTING DRAPING MATERIALSSelecting appropriate, high-quality draping materials is animportant step in protecting patients from surgical-site andother health-care-associated infections.1 Several factors meritconsideration during this process.Standards for surgical drapes have evolved over time asresearchers have studied and improved the physical barrierfunction of draping materials.Reusable woven fabrics have been used to protect the surgicalsite since the turn of the last century.2 Initially, the mostfrequently used material for draping was muslin, a looselywoven cotton fabric; however, muslin was later observed tolose its barrier efficacy when wet. Because of this, muslineventually was replaced with other woven, reusable materialsand with nonwoven, single-use disposable surgical drapes.Drapes should be intact and of sufficient quality to withstandexposure to blood, body fluids, and other potentially infectiousmaterials, as well as other liquids, rips, and abrasions. Drapeswith holes, wear, or tears can allow microorganisms to passthrough, increasing the risk of surgical site and other healthcare-associated infections. In addition, the wicking of liquid5
S TERILE D RAPING : F UNDAMENTAL P RACTICESthrough a surgical drape can facilitate the passage of microbes.Excess pressure or stretching on a drape can also facilitatemicrobial transfer, if the force applied to the drape exceedsthe material’s inherent resistance.Finally, AORN recommendations state that drapes shouldhave an acceptable cost-benefit ratio. However, cost shouldnot be the main consideration when choosing surgical drapeproducts.For these reasons, perioperative personnel should select drapeproducts that are as resistant to penetration by blood, otherbody fluids, and tear force from hands and surgicalinstruments, as necessary, based on the specifics of theinvasive procedure for which drapes will be used. AORNfurther recommends that manufacturers provide data on theability of their materials to resist passage of microbes,particulates, and fluids, and that end users review this data.ESSENTIAL PRINCIPLES OF DRAPINGMaximal sterile barrier precautions should be implemented toreduce the risk of health-care-associated infections. TheCenters for Disease Control and Prevention (CDC)recommends maximal sterile barrier precautions, includingplacement of a full-body drape during placement of centralvenous catheters, peripherally inserted central catheters, andguidewire exchanges.7This recommendation was the result of a randomized,controlled trial of patients undergoing non-tunneled centralcatheter insertion that was conducted at a 500-bed oncologyreferral center. The study found that the use of maximumsterile barrier precautions, which consisted of a full-bodysterile drape plus a sterile gown, gloves, mask, and cap, wasassociated with lower rates of catheter colonization andcatheter-related bloodstream infections as compared with theuse of sterile gloves and a small drape only. The rate ofcatheter-associated septicemia in the control group was 6.3times higher than in the intervention group. A cost-benefitanalysis also favored the use of maximum barrierprecautions.8Drapes should also be nontoxic, nonallergenic, maintainambient and desired body temperature, and be large enoughto conform to the patient’s body.1 Drapes should be low-lintingbecause microorganisms and other particulates can attach tolint and settle in the surgical site or wound, causing SSIs.5Several important practices should be implemented tomaintain sterility of surgical drapes and optimize theirperformance.First, sterile drapes should be handled and moved as little aspossible.1 Extraneous movement creates air currents, whichincreases the risk of contamination with airbornemicroorganisms and particles (e.g., lint and dust) thatsubsequently could enter the surgical site. In one study,researchers confirmed the presence of airborne contaminantsin an OR by using a personal cascade impactor samplingReusable drapes should be made from materials that areappropriate for the sterilization method used by the health carefacility.1 Workers should not resterilize unused single-usedrapes, unless they follow U.S. Food and Drug Administration(FDA) guidelines, or the specific written instructions of themanufacturer.6
S TERILE D RAPING : F UNDAMENTAL P RACTICESdevice to identify airborne lint and bacterial pathogens (e.g.,Staphylococcus aureus) near the surgical field during vascularsurgery.5Second, because microbial contamination is time-dependent,the amount of time between creation of the sterile field andthe start of surgery should be kept as short as reasonablypossible.1To secure cables, tubing, and other surgical equipment to thedrape, non-perforating tools should be used.1 Perforating thedrape while attaching equipment to it increases the risk ofmicrobial contamination and exposure to blood, body fluids,and other potentially infectious materials. It is preferred thatsterilized instruments and tools added to the sterile fieldshould be passed to a scrubbed team member instead of beingplaced on the draped sterile field.In addition, surgical drapes must be held so they cannot comein contact with unsterile surfaces.1 When draping the patient,the team members placing the drapes should begin at thesurgical site and move toward the peripheral areas. Thisprevents drapes from dragging particles and microbes into thesterile field. Drapes also should be positioned so that whenscrubbed team members lean over the sterile field during aprocedure, the front of their surgical gowns do not touchunsterile surfaces.Finally, the upper part of the C-arm drape should beconsidered contaminated.1 This recommendation is based onresults from a prospective study of the sterility of C-armdrapes used during spinal surgery.9 Preoperative (control) andpostoperative cultures were performed of swabs taken fromfive different sites on standard fluoroscopic C-arm drapes.Postoperative contamination was confirmed for all the sitestested, but contamination was highest at the top of the C-armdrape (56% of drapes contaminated) and the upper front ofthe receiver (28% contaminated). In contrast, the controldrapes had a contamination rate of only 4%.Only the top of a draped table is considered sterile.1 Any partof the drape that falls below the table edge is regarded asunsterile and must not be moved back to the sterile zone.Likewise, if a sterilized item extends beyond the sterileboundary, it should be considered contaminated.Contaminated items must be removed and not returned to thesterile field.7
S TERILE D RAPING : F UNDAMENTAL P RACTICESUSING DRAPES TO ESTABLISH A STERILEFIELDThis section reviews correct practices for laparotomy.6 Manyaspects of draping for laparotomy also apply to drapingpatients for other types of surgery.LaparotomyThe AORN guidelines recommend that unsterile equipment(e.g., Mayo stands) be fully covered with sterile barriersbefore they are brought into the sterile field.1 Sterile-barriermaterial should also cover the parts of equipment that arepositioned immediately adjacent to the sterile field. Inaddition, drapes should be controlled in a way that preventsDraping Equipment them from moving and creating unnecessary air currents ortouching unsterile surfaces before or during an invasiveprocedure.Sterile towels are used to outline the prepared surgical site.The folded laparotomy sheet is then placed on the prepped patient.The fenestration (opening) of the sheet should be directly on top of the surgical site. The fenestration is reinforced foradditional protection and control of seepage of blood, body fluids, and other potentially infectious materials.The sterile gloves of the scrub person are protected by keeping them under the cuff of the folded laparotomy sheet.The drape is unfolded over the sides of the patient and the procedure or operating table or bed.The upper part of the sheet is unfolded toward the head of the bed and draped over the anesthesia screen.The bottom of the sheet is draped over the foot of the bed.8
S TERILE D RAPING : F UNDAMENTAL P RACTICESprepared. For procedures that require the use of largequantities of fluid (e.g., arthroscopy, wound irrigation), it isimportant to use drapes that do not permit soaking.1DRAPING FOR SPECIFIC OPERATIVEPROCEDURESThis learning guide next reviews aspects of draping forextremity, lithotomy, head and face, and robotic procedures.Another option to consider is the use of specially-designedsterile, disposable drapes that have fenestrations for the upperand lower limbs.When preparing for extremity surgery, the patient’s limbshould be draped after he or she is positioned and the skin isExtremity ProceduresThese steps should be followed6: A sheet is placed under the extremity.A towel is placed around the extremity, above the intended surgical site, and secured with a non-perforating towelclip.The extremity is covered with a sterile stockinette.The stockinette is an impervious, cylindrical drape that the scrubbed team member rolls up the arm or leg.A sheet is placed above the surgical area and secured with non-perforating towel clips.The extremity is drawn through the opening of a fenestrated drape.9
S TERILE D RAPING : F UNDAMENTAL P RACTICESspecifically designed to cover the legs and the surgical site.When practicing this method, two scrubbed team membersare required to open the folds and position the leggings overthe legs.Perioperative personnel may use either a single fenestrateddrape or multiple drapes during a lithotomy procedure.6Lithotomy ProceduresThe single-drape method uses a one-piece drape that isThese steps should be followed: First, the under-buttocks sheet is placed beneath the patient. The perineal area may be outlined with sterile towels. The drape is brought down between the legs so that the perineal fenestration can be seen. Placing gloved hands in the cuff, each legging is opened and drawn over a leg. The drape is unfolded toward the head. The armboard covers are then extended laterally. Surgical lines and tubing are then inserted through the tube holders and pouches on the drape.When using multiple drapes: First, the under-buttocks sheet is placed beneath the patient.The perineal area may be outlined with sterile towels.Then the triangular lithotomy leggings are unfolded and drawn over the legs.Next, a fenestrated sheet is placed over the lower abdomen so that the opening is just above the pubic bone, exposingthe genitals and perineum.A plain, non-fenestrated sheet is used for an anesthesia screen.10
S TERILE D RAPING : F UNDAMENTAL P RACTICESSome procedures require that the patient’s face be exposed(e.g., nasal surgery, blepharoplasty).Head and Face ProceduresTo adequately drape the patient, these steps should be followed: After the patient is positioned and the skin prepared, the scrubbed person should place a sterile towel on a sterilesheet.The center of the towel edges should be set approximately 2 inches in from the center of the sheet.The scrubbed team member’s gloved hands should remain within a protective cuff as the towel and drape are placedunder the patient’s head.The patient’s head is elevated by an unscrubbed team member as the scrubbed person places the drape.The towel is brought up and around the patient’s head, over the forehead to the hairline, first one side and then theother.The towel is secured with a small, non-perforating towel clip.The surgical site is framed with 2 to 3 additional towels.A fenestrated, U-shaped drape is placed just below the surgical site.The sides of the drape are brought up to overlap the drape that is under the head.The bottom half of the operating bed is covered with an additional sheet.When preparing for robotic surgery, the robotic system shouldbe draped in sequence to implement and maintain sterility. Thegeneral sequence for draping is as follows6:Use of robots during invasive procedures is becoming morecommon as technologies expand and are adapted for specificmedical conditions.6 Robotic surgeries offer severaladvantages, including the potential for smaller incisions;decreased bleeding; less tissue trauma, inflammation, andpostoperative pain; and shorter hospital stays and recoverytimes.Robotic Procedures Methods of draping patients for robotic surgeries depend onthe particular procedure being performed. For gynecologicprocedures, for example, the patient should be draped usingthe same practices as for laparoscopic surgery.611The ports, instruments, and arm clutching are draped.Then, the instrument arm is draped.Next, the touch screen monitor and the camera armare draped.The endoscope and assembly are draped last.
S TERILE D RAPING : F UNDAMENTAL P RACTICESSUMMARYEvidence supports the use of sterile surgical drapes to protectperioperative personnel and patients during surgical and otherinvasive procedures. Perioperative professionals play animportant role in using surgical drapes to create and protectthe sterile field. Draping is most effective when perioperativeteam members plan the process carefully, evaluate sizes andcharacteristics of drapes based on the requirements forparticular procedures and individuals, and follow standardizeddraping practices that maximize both patient safety andfacility resources.12
S TERILE D RAPING : F UNDAMENTAL P RACTICESREFERENCES1. Recommended practices for sterile technique. In: Perioperative Standards and Recommended Practices. Denver,CO: AORN, Inc; 2013: 91-119.2. Belkin NL. Barrier drapes and their impact on surgical site infections. Infection control today. May 1, al-site.aspx.Accessed March 14, 2013.3. Belkin NL. Surgical gowns and drapes as aseptic barriers. Am J Infect Control. 1988;16(1):14-18.4. Association for the Advancement of Medical Instrumentation. AAMI PB70: liquid barrier performance andclassification of protective apparel and drapes intended for use in health care facilities. Arlington, VA: Associationfor the Advancement of Medical Instrumentation; 2012.5. Edmiston CE Jr, Sinski S, Seabrook GR, Simons D, Goheen MP. Airborne particulates in the OR environment.AORN J. 1999;69(6):1169-1172, 1175-1177, 1179 passim.6. JC Rothrock, ed. Alexander’s Care of the Patient in Surgery. 14th ed. St. Louis, MO: Mosby-Elsevier; 2011.7. Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR; Centers for Disease Control and Prevention (CDC)Hospital Infection Control Practices Advisory Committee. Guideline for prevention of surgical site infection, 1999.Am J Infect Control. 1999;27(2):97-132.8. Raad II, Hohn DC, Gilbreath BJ, et al. Prevention of central venous catheter-related infections by using maximalsterile barrier precautions during insertion. Infect Control Hosp Epidemiol. 1994;15(4)(Pt 1):231-238.9. Biswas D, Bible JE, Whang PG, Simpson AK, Grauer JN. Sterility of C-arm fluoroscopy during spinal surgery.Spine (Phila Pa 1976). 2008;33(17):1913-1917.10. Webster J, Alghamdi AA. Use of plastic adhesive drapes during surgery for preventing surgical site infection.Cochrane Database Syst Rev. 2013 (1);CD006353. doi:10.1002/14651858.CD006353.13
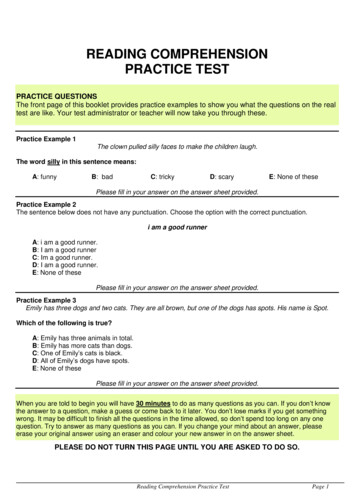
S TERILE D RAPING : F UNDAMENTAL P RACTICESPOST-TESTSTERILE DRAPING: FUNDAMENTAL PRACTICESMultiple choice. Please choose the word or phrase that best completes the following statements.5. When using a single drape for a lithotomy, thefollowing instructions are correct, EXCEPT:a. place the drape so the edge is 2 inches from theperineumb. use the drape to cover the legs and surgical sitec. unfold the drape toward the head, with thearmboard covers extended laterallyd. bring the drape between the legs so that theperineal fenestration is visible1. Which of the following is NOT an effective practiceto optimize the performance and safety of sterilesurgical drapes?a. Resterilizing an unused, single-use drape onlyafter consulting the manufacturer’s labelingdirections and FDA guidelinesb. Using a drape that is sized to conform closelyto a patient’s bodyc. Selecting drapes based on the seepage, tearforce, and duration expected for a particularinvasive procedured. Development of industry-wide standards bymanufacturers for consistent classification andlabeling of surgical drapes6. When using several drapes for a lithotomyprocedure, which of the following steps is NOTcorrect?a. Place the under-buttocks sheet underneath thepatientb. Unfold the triangular lithotomy leggings all theway down the legsc. Place the fenestrated sheet over the lowerabdomen so that the opening exposes thegenitals and perineumd. Use a second fenestrated sheet for an anesthesiascreen2. Which of the following could compromise thephysical barrier function of a sterile surgical drapeand increase the risk of surgical site infections?a. Blood pooling on the drapeb. Water wicking through the drapec. Excessive pressure or stretching during aprocedured. All of the above7. When draping for an extremity procedure,perioperative personnel should choose surgicaldrapes with increased ability to withstand wickingand pooling.a. Trueb. False3. When draping equipment:a. fully cover Mayo stands after they areintroduced to the sterile fieldb. cover only the part of the equipment that ispositioned next to the sterile fieldc. control the drapes to prevent them from movingand touching unsterile surfaces before or duringan invasive procedured. none of the above8. Which of the following steps is NOT a correct stepin draping for head and face procedures?a. The patient’s head is elevated by a scrubbedteam member as the scrubbed person places thedrape.b. The towel is brought up and around the patient’shead, over the forehead to the hairline, first oneside and then the other.c. The towel is secured with a small, nonperforating towel clip.d. The surgical site is framed with 2 to 3 additionaltowels.4. When draping for a laparotomy, which of thefollowing is NOT an accepted practice?a. Use sterile towels to outline the preparedsurgical siteb. Place the fenestration directly above theprepped surgical sitec. Drape from the edges of the table toward thesurgical sited. Protect the sterile gloves of scrubbed teammembers by keeping them under the cuff of thefolded laparotomy sheet14
S TERILE D RAPING : F UNDAMENTAL P RACTICES9. When draping for a robotic surgery, which order ofdraping should perioperative personnel follow?a. Endoscope and assembly; instrument arm;ports, instruments, and arm clutching; touchscreen monitor and camera armb. Ports, instruments, and arm clutching;instrument arm; touch screen monitor andcamera arm; endoscope and assemblyc. Endoscope and assembly; touch screen monitorand camera arm; instrument arm; ports,instruments, and arm clutchingd. None of the above10. Draping is most effective when perioperative nursesand other health care workers:a. plan the draping process carefullyb. choose types and sizes of drapes by consideringwhat is needed for particular procedures,patients, and team membersc. follow standardized draping practices thatmaximize both patient safety and facilityresourcesd. all of the above15
S TERILE D RAPING : F UNDAMENTAL P RACTICESPOST-TEST ANSWERSSTERILE DRAPING: FUNDAMENTAL PRACTICES10. d9. b8. a7. a6. d5. a4. c3. c2. d1. b16
The purpose of this study guide and companion video is to review techniques for sterile draping, which is a fundamental aspect of sterile technique. OBJECTIVES After viewing the video and completing the study guide, the participant will be able to: 1. Explain the rationale fo