Transcription
Ann Otol Rhinol Laryngol 108:1999COMPARISON OF NERVE BANKING TECHNIQUES IN DELAYEDLARYNGEAL REINNERVATIONK. LINNEA PETERSON, MDSEATTLE, WASHINGTONROBERT J. ANDREWS, MDLos ANGELES, CALIFORNIAMING YE, MDLos ANGELES, CALIFORNIAJ O E L A. S E R C A R Z ,MDKEVIN KEVORKIAN,Los ANGELES, CALIFORNIAK E I T H E. B L A C K W E L L ,MDMDLos ANGELES, CALIFORNIAGERALD S. BERKE, MDLos ANGELES, CALIFORNIALos ANGELES, CALIFORNIASuccessful laryngeal transplantation will require adequate reinnervation of the larynx to allow phonation, coordinated swallowing, and respiration. A delay between laryngectomy and transplantation would be necessary in oncology patients because of the needfor immunosuppression. In these patients, reinnervation of the donor organ would require "banking" and recovery of dormantrecipient recurrent laryngeal nerves (RLNs). This pilot study was undertaken to compare the effectiveness of RLN storage using 1 of2 techniques: 1) inserting the nerve into a muscle pocket or 2) anastomosing the proximal RLN stump to the ansa cervicalis. Sixmonths following nerve transection and "banking," the proximal anterior branch of the RLN was reanastomosed to the distal anterior segment and the posterior branch was anastomosed directly to the posterior cricoarytenoid muscle. Tensionometry, image analysis, and electromyographic data were collected 1 year later. Results show reinnervation of adductors and abductors with both techniques. Banking of the RLN branches during total laryngectomy is effective and should permit delayed physiological reinnervationfollowing laryngeal transplantation.KEY WORDS — delayed reinnervation, laryngeal reinnervation, laryngeal transplantation.innervate the musculature. Once the larynx has beentransplanted, 6 to 12 months must pass before thefunctional outcome is known. In the interim, the patient requires tracheostomy and must depend on alternative methods of communication, such as use of anelectrolarynx.INTRODUCTIONLaryngeal transplantation remains an elusive goalof laryngologiste. Several criteria must be met in order for laryngeal transplantation to be successful. Thedonor organ must work as a dynamic functional unitthat allows phonation, coordinated swallowing without aspiration, and an adequate airway diameter.These functions must be equal to or better than thoseof patients with a total laryngectomy and excellenttracheoesophageal fistula speech.Techniques and outcomes of laryngeal reinnervation have varied. Methods include direct anastomosis,1'2 nerve grafting3 with nerves such as the vagusand phrenic, laryngeal nerve-muscle pedicle,4 andnerve-muscle pedicle reinnervation with a branch ofthe ansa.5 Outcome has been contradictory at times,with some investigators reporting poor outcome withlittle evidence of reinnervation6 and others reporting moderate to good results.5·7·8 More recent techniques have involved selective reinnervation of theabductor and adductor branches of the recurrent laryngeal nerve (RLN).2-8These results have been promising, achieving reinnervation and function whileminimizing the problem of synkinesis9 and paradoxical vocal cord motion. However, each of these studies was done with immediate repair or grafting.Immunosuppression must be adequate to allow organ survival without significant compromise of thepatient's overall health or oncological result. Unlessmore targeted immunosuppression is developed, patients with malignancies will require a delay betweenlaryngectomy and transplantation in the range of 1to 2 years in order to reduce the likelihood of recurrence. This delay adds complexity to an already challenging task, requiring return of appropriate function of a recipient nerve that has been dormant foran extended period of time. The nerve must haveadequate axon sprouting into the donor larynx to re-From the Division of Head and Neck Surgery, University of California, Los Angeles School of Medicine, Los Angeles, California. This workwas supported by Veterans Administration Merit Review Grant 0001. This study was performed in accordance with the PHS Policy on HumaneCare and Use of Laboratory Animals, the NIH Guide for the Care and Use of Laboratory Animals, and the Animal Welfare Act (7 U.S.C. etseq.); the animal use protocol was approved by the Institutional Animal Care and Use Committee (IACUC) of the University of California, LosAngeles.Presented at the meeting of the Pacific Coast Oto-Ophthalmological Society, San Diego, California, June 21-24, 1997. Winner of the 1997Resident Research Award of the Pacific Coast Oto-Ophthalmological Society.CORRESPONDENCE — K. Linnea Peterson, MD, Virginia Mason Medical Center, Dept of Otolaryngology, X10-ON, 1100 Ninth Ave, Seattle,WA98111.689
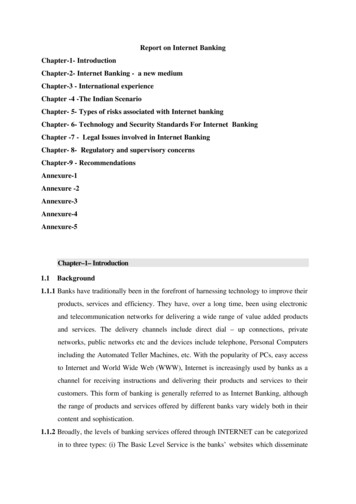
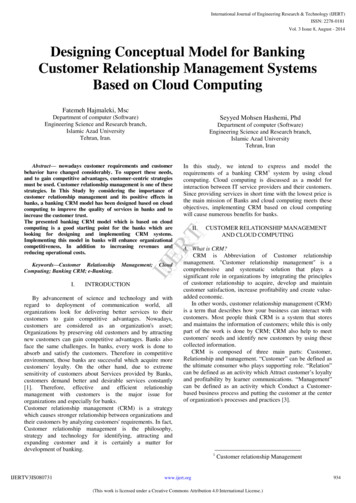
690Peterson et al, Delayed Laryngeal Reinnervation\lAnterior branchAnterior branchFig 1. Schematic of surgical procedure for ansastorage. A) Stage 1 procedure with anastomosisof proximal anterior and posterior branches to ansacervicalis branches. B) Stage 2 procedure withanastomosis of proximal anterior branch to distalsegment of anterior branch, and placement of posterior segment into pocket of posterior cricoarytenoid (PCA) muscle. RLN — recurrent laryngealnerve.Anterior branchAnterior branchRLNBThe current study was undertaken to address theoutcome of "banking" nerves for later transplantation, to minimize degeneration of the nerve. Two different methods were used and results were comparedin this preliminary study. Neural storage, or anastomosis to a branch of the ansa, was compared to theuse of a nerve-muscle pedicle or a nerve-muscle"pocket."MATERIALS AND METHODSExperimental Model. Two male mongrel dogs (25and 35 kg) were studied. The first dog underwentdivision of the anterior and posterior branches of theRLN with anastomosis of the proximal segments tothe ansa cervicalis. The second dog underwent division of these branches with use of a nerve-musclepedicle to the stemothyroid muscle for the posteriorbranch, with the anterior branch being tucked directlyinto a muscle pocket of this same muscle.Methods. Each dog was anesthetized with intravenous pentobarbital sodium and placed supine on anoperating table. Direct laryngoscopy was performedto confirm normal laryngeal anatomy. The animalwas intubated with a 7.0 endotracheal tube under direct visualization, and kept under general anesthesiawith inhalation of halothane in the range of 1 % to1.5%, with oxygen at 4 L/min.A midline incision was made from the upper border of the thyroid cartilage to just below the cricoidcartilage. Trie superior laryngeal nerve was identified and preserved. The inferior border of the cricopharyngeus was cut to allow access to the distal portion of the RLN at the point of bifurcation into anterior and posterior branches, and the branches werethen isolated on the left side. In the first experimen-tal dog, branches of the ansa cervicalis were identified and cut. The proximal segments of the anteriorand posterior branches of the RLN were then anastomosed to distal segments of the ansa (Fig 1). Thesecond experimental animal had a muscle pediclecut from the posterior cricoarytenoid (PCA) musclefor the posterior branch of the RLN. This musclepedicle was sutured to the stemothyroid muscle. Theanterior branch was cut, and the proximal neural endwas placed into a pocket in the strap muscle and secured (Fig 2). The wounds were then closed, and theanimals were recovered.The dogs were kept for 6 months and then returnedto the operating room for a second procedure, atwhich time the anterior and posterior branches ofthe RLN were reanastomosed or placed into targetmuscles. By the same protocol, the dogs were placedunder general anesthesia. Via the same approach, theanterior and posterior branches of the RLN were isolated. The proximal and distal ends of the anteriorbranches were identified and reanastomosed; in thefirst dog, this required transection of the RLN-ansasegment. The new anastomosis may have containeda portion of the ansa graft. The posterior branch wascut, again possibly with some ansa graft, and the endwas inserted into a pocket of the PCA muscle. In thesecond dog, the proximal portion of the anteriorbranch was cut just prior to its insertion into the strapmuscle. The distal end of the anterior branch waslocated, and the nerve ends were reanastomosed. Theposterior branch was cut just as it entered the strapmuscle, and the proximal end was tucked into thePCA muscle. The dogs were again recovered, withsuture removal at about 2 weeks.One year later, the dogs were returned for a third
691Peterson et al, Delayed Laryngeal ReinnervationAnterior branchFig 2. Schematic of surgical procedure for muscle storage. A)Stage 1 procedure with bankingof anterior branch into pocket ofsternothyroid muscle and musclepedicle of posterior branch intostrap muscle. B) Stage 2 procedure with anastomosis of proximal and distal ends of anteriorsegment, and placement of posterior segment into pocket in PC Amuscle.PCASternothyroidAnterior branchBsurgery, at which time tensionometry, video, andelectromyography (EMG) data were collected. Thesame protocol for general anesthesia was followed.A midline incision was made from the superior endof the thyroid cartilage to just above the sternal notch.A distal tracheostomy was placed, and the oral endotracheal tube was removed. A mouth gag was usedto allow direct visualization of the larynx. A buttonwas placed through the epiglottis to suspend the epiglottis out of the field of view. Videolaryngoscopyand tensionometry were performed with obstructiverespiratory dyspnea. Electromyography was performed under conditions of obstructive respiratorydyspnea and pharyngeal stimulation, recording signals from the PCA and thyroarytenoid (TA) muscles,respectively. The first dog, with muscle banking, developed bilateral tension pneumothoraces during theexperiment and was unable to be resuscitated. Tensionometry data are not available for this animal.The RLNs were dissected out bilaterally, and rubber electrodes (monopolar, flexible, conductive neoprene with silicone, coated by insulating siliconeKE45 W) were applied. Videolaryngoscopy and tensionometry data were collected with nerve stimulation. Finally, the animals were humanely euthanizedaccording to the Animal Care and Use protocol. Theanterior and posterior branches, as well as the maintrunk, of the left RLN were harvested from both animals. The larynx was also removed. All tissue wasplaced in 10% formalin for fixation.Equipment. For videolaryngoscopy, a 0 Storz endoscope was placed through the mouth and abovethe vocal cords. A video camera was used to recordimages on a Sony U-matic Vidéocassette Recorder,model VO-9850 (Sony, Japan). Analysis was per-formed with ImagePro for Windows 3.1 software(Media Cybernetics, NJ) on a Zeos 486 PC, with aFlashPoint ISA (Version 2.0, Integral Technologies,Indianapolis, Ind) color frame grabber. Measurements were made of vocal cord excursion under thegiven conditions, to compare the relative excursionof each side against the midline. Measurements weremade of glottal area in the relaxed state and withmaximal abduction. Measurements with nerve stimulation were compared from separate trials.Abductory force measurements were made by a"tensionometer," as described by Nasri et al,10 byplacing a straight rod with a plate with a surface areaof 3.06 mm2 just lateral to the midportion of the arytenoid. The tensionometer was adapted with a digital force gauge (DF-0.5R, Shimpo, Japan). Adductorymeasurements were made with the same rod, by placing the plate medial to the true vocal cord, just anterior to the anterior border of the arytenoid. Comparative measurements were made for abductory and adductory force under each set of conditions. Five sequential measurements of abduction or adductionwere made for each trial. Zero and peak readingswere recorded, and the zero settings were subtractedout.A constant current nerve stimulator was used (WRMedical Electronics Co, St Paul, Minn, model S2LH)for RLN stimulation. The frequency and duration ofstimuli were 80 Hz and 1.5 milliseconds' duration,respectively. The stimulus levels for abduction measurements were set by finding the threshold levelfor maximal abduction. The adductory measurementswere made at the threshold for complete glottal closure.Electromyography was performed with the Nicolet
692Peterson et al, Delayed Laryngeal ReinnervationTABLE 1. TENSIONOMETRY DATA FOR ANSASTORAGE ANIMALRightLeftPCA (abduction)Tube occlusion1.95 0.712.42 0.24RLN stimulation2.72 0.081.98 0.40TA (adduction)RLN stimulation4.50 0.254.38 0.50Data are in grams (mean SD).PCA — posterior cricoarytenoid, RLN — recurrent laryngeal nerve,TA — thyroarytenoid.Viking IV system (Nicolet, Madison, Wis). Concentric needle electrodes (26 gauge, 3.7 cm long, recording area 0.068 mm2; Nicolet) were used, with theneedles placed into the respective muscles via a transoral approach.All animal protocols were approved by the UCLAAnimal Care and Use Committee and were performed in compliance with the local, state, and federal regulations for the humane use of animals in research.Statistical Analysis. Statistical analysis was performed by a 1-way, repeated-measures analysis ofvariance comparing sides under each set of conditions. Tensionometry data were assessed to compareabductory and adductory force on sides under conditions of nerve stimulation and obstructive respiratory dyspnea. The data were analyzed with SYSTATsoftware. Glottal images obtained from nerve stimulation were analyzed to compare vocal cord excursions on each side. These data are reported in termsof mean and standard deviation.RESULTSTensionometry. Tensionometry data are availableonly for the dog that underwent ansa storage (Table1 and Fig 3). The results show no significant difference between the left side and the right for abductory QTABLE 2. IMAGE ANALYSIS COMPARINGEXCURSIONS OF RIGHT VERSUS LEFT CORDSAND GLOTTAL AREA IN ANSA STORAGE ANIMALVERSUS MUSCLE STORAGE ANIMALRightLeftTube occlusionAnsa57.13 1.9942.87 1.99Muscle61.80 2.3238.20 2.32Stimulation of RLNMuscle33.79 6.6637.22 4.13After SLN transectionMuscleData are percent (mean SD)SLN — superior laryngeal nerve.*Relaxed state to maximal abduction.Changein Area*36.97 4.4230.89 3.8815.89 4.21force under conditions of tube occlusion. With stimulation of the posterior branch of the RLN, abductoryforce was greater on the right than the left, with astatistically significant difference: p .05, F(l,4) 25.35. With stimulation of the main trunk of the RLN,there was nearly equal force of adduction and no statistically significant difference.Image Analysis. Video data demonstrated vocalcord excursion from midline of right versus left vocal cords, as well as change in glottal area from therelaxed state to full abduction under varying conditions (Table 2 and Fig 4). These results show theexcursion on the right to be approximately 57% ofthe glottal width, versus 43% for the left under conditions of tube occlusion for the animal with ansa storage (SD 1.99%). This 43% for the left represents75% of the excursion demonstrated on the right. Theanimal with muscle storage had 62% for the rightversus 38% for the left, under the same conditions(SD 2.32% for both sides). This is 62% of the expected excursion, or the excursion found on the right.The change in glottal area from the relaxed state tofull abduction with tube occlusion shows a 36.97%change (SD 4.42%) in total area with ansa storage,6Ansa- Nerve stimulation, rightAnsa- Nerve stimulation, left541 D4--Ansa-Tube occlusion, rightAnsa-Tube occlusion, leftAnsa-Nerve stimulation, rightAnsa-Nerve stimulation, left33"2"BFig 3. Ansa storage. A) Force of adduction with nerve stimulation, right versus left. B) Force of abduction,tube occlusion versus nerve stimulation, right versus left.
693Peterson et al, Delayed Laryngeal Reinnervation1008060100 Ansa- Tube occlusion, right0Ansa- Tube occlusion, left-,ΘGMuscle- Tube occlusion, rightMuscle- Tube occlusion, leftS 80- 7090CO(DΦH1 60co-5 500)σ 4 040COΐ20ϋaD. Ansa- Tube occlusion0Muscle- Tube occlusion-3020-10BFig 4. Image analysis. A) Relative excursion with tube occlusion, ansa versus muscle storage, right versusleft. B) Percentage change in area with tube occlusion, ansa versus muscle storage.versus only a 30.89% change (SD 3.88%) with muscle storage. The results for RLN stimulation show a33.79% change (SD 6.66%) in area with stimulationon the right versus a 37.22% change (SD 4.13%)with stimulation on the left in the dog with musclebanking. No RLN stimulation data are available forthe ansa storage dog.Electromyography. The EMG data for the 2 animals showed evidence of selective reinnervation ofthe TA and PCA muscles (Figs 5 and 6). There wasphysiologically appropriate firing of motor units, thePCA firing with respiration and the TA firing withpharyngeal stimulation and adduction. The dog withansa storage showed a single motor unit for both theTA and PCA muscles. The dog with muscle storagedemonstrated similar signals, although with smallermotor units.DISCUSSIONThe success of laryngeal transplantation for cancer patients requires the coordination of immunosuppression and functional reinnervation. The latter appears to be the most limiting factor, while improvements in immunosuppression have allowed excellent results in solid organ transplantation. Techniquesin reinnervation have evolved, especially over thepast 20 years, with methods to avoid synkinesis. Inour laboratory, selective reanastomosis of the adductor and abductor branches has been successful inachieving reinnervation with functional, physiological motion.2'10200 uV5 nsThe desire to avoid immunosuppression of cancer patients requires a delay in transplantation untilthe risk of cancer recurrence is low. In order for thesepatients to be eligible for future transplantation, theywould need to have their RLNs preserved by "banking" them to prevent nerve degeneration.The results of this study demonstrate return ofphysiological motion following denervation of theanterior and posterior branches of the RLN with a 6month delay between transection and reanastomosis.One year was allowed for neural regeneration priorto data collection. Two different techniques of banking were used: ansa cervicalis storage with neuralanastomosis of the proximal segments of the anterior and posterior branches of the RLN to branches ofthe ansa; and muscle storage with the anterior branchtucked into a pocket in the sternothyroid muscle, anda muscle pedicle of the posterior branch attached tothis same strap muscle.Tensionometry data show good return of forcewith ansa storage, with nearly equal adductory force.Abductory force also had good recovery, with no statistically significant difference between the operatedand control sides with obstructive respiratory dyspnea. With nerve stimulation, there was a significantdifference, with the left being weaker than the right.Tensionometry measures could not be performed inthe muscle banking animal.The image data also support the recovery of bothlaryngeal abduction and adduction. Both animals had100 ns50 uV5 ns100 ns W X»4 *44 π' M " Fig 5. Electromyography with ansa storage. A)PCA muscle with tube occlusion in single motor unit followed by burst of activity with abduction. B) Thyroarytenoid (TA) muscle withglottal closure in single motor unit and activity with adduction. M ,AB
694Peterson et al, Delayed Laryngeal Reinnervation100 uV5 «15— " - · 200 UV Φίι β ίφφ 5 ms200 ms\BFig 6. Electromyography with muscle storage. A) PCA muscle with tube occlusion in distant single motor unit and tracingshowing phasic activity with respiration. B) TA muscle with glottal closure in single motor unit and tracing showing variationin activity with contraction.appropriate vocal cord motion with obstructive respiratory dyspnea and nerve stimulation. The ansa storage animal had an excursion of 75.04% of expectedfor the operated side with obstructive respiratorydyspnea (42.87% of total glottal excursion on theoperated side versus 57.13% for the nonoperated orcontrol side). The dog with muscle storage achieved61.8% of excursion with tube occlusion. Comparison of changes in glottal area with tube occlusiondemonstrate a greater percentage change from therelaxed state to complete abduction in the animalwith ansa storage versus the muscle banking dog(36.97% change for ansa versus 30.89% change formuscle).Electromyography data also demonstrated reinnervation in both animals, with PCA motor units firingappropriately with respiration under obstructive dyspnea conditions. Thyroarytenoid motor units firedwith light anesthesia and subsequent glottal closure.Overall, results from "banking" the nerves demonstrated functional recovery and reinnervation without synkinesis following 6 months of neural storage. Both methods were successful. Anastomosis toa similar-size nerve such as the ansa cervicalis wouldbe expected to be preferable for nerve preservation,rather than storage in a muscle. Because only 2 animals were studied, additional investigation is necessary to determine whether one method offers a consistent advantage over the other.Moreover, results from this study indicate that current patients who undergo total laryngectomy should,when it is oncologically feasible, undergo bankingof the anterior and posterior RLN branches on at least1 side. It is impossible to predict how immunosuppression techniques will evolve. Total laryngectomypatients with banked nerves will have the potentialto undergo laryngeal transplantation with return ofphysiological function.ACKNOWLEDGMENTS — The authors thank Jody Kreiman, PhD, for her assistance with statistical analysis, Deborah Watson, MD, for herillustrations, and Michael Graves, MD, for his help with electromyography.REFERENCES1. Gordon JH, McCabe BF. The effect of accurate neurorrhaphy on reinnervation and return of laryngeal function. Laryngoscope 1968;78:236-50.6. Takashiro T. Experimental studies on the reinnervationof larynx after accurate neurorrhaphy. Laryngoscope 1972;82:225-36.2. Green DC, Berke GS, Graves MC, Natividad M. Physiologic motion after vocal cord reinnervation: a preliminary study.Laryngoscope 1992;102:14-21.7. Murakami Y, Kirchner JA. Vocal cord abduction by regenerated recurrent laryngeal nerve: an experimental study inthe dog. Arch Otolaryngol 1971;94:64-8.3. Iwamura S. Functioning remobilization of the paralyzedvocal cord in dogs. Arch Otolaryngol 1984;100:122-9.4. Hengerer AS, Tucker HM. Restoration of abduction inthe paralyzed canine larynx. Arch Otolaryngol 1973;97:24750.5. Tucker HM. Human laryngeal reinnervation. Laryngoscope 1976;86:769-79.8. Crumley RL. Selective reinnervation of vocal cord adductors in unilateral vocal cord paralysis. Ann Otol Rhinol Laryngol 1984;93:351-6.9. Crumley RL. Laryngeal synkinesis: its significance tothe laryngologist. Ann Otol Rhinol Laryngol 1989;98:87-92.10. Nasri S, Sercarz JA, Azizzadeh B, Kreiman J, Berke GS.Measurement of adductory force of individual laryngeal musclesin an in vivo canine model. Laryngoscope 1994;104:1213-8.
surgery, at which time tensionometry, video, and electromyography (EMG) data were collected. The same protocol for general anesthesia was followed. A midline incision was made from the superior end of the thyroid cartilage to just above the sternal notch. A distal tracheostomy was placed, and