Transcription
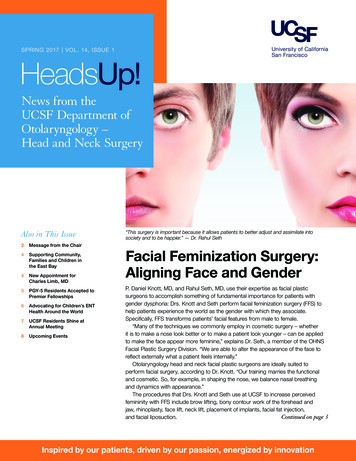
10/13/20Department of Otolaryngology- Head and Neck SurgeryDysphagia Evaluation inHNC PopulationsBrian Peterson, MA, CCC-SLPOctober 2020CHANGING MEDICINE.CHANGING LIVES. 1Objectives Learners will:– Gain information related to overarching goals of dysphagiamanagement in HNC population– Gain information on the impact of various surgical managementoptions on swallow function– Gain information on the UIHC SLP C/RT dysphagia clinical pathway– Gain information regarding the support for SLPs in the multidisciplinaryHNC teamDepartment of Otolaryngology- Head and Neck Surgery2HNC Dysphagia Can be related to:– Tumor burden– Result of surgical resection and reconstruction– Acute effects of C/RT– Late-onset tissue fibrosis– Cranial nerve neuropathiesDepartment of Otolaryngology- Head and Neck Surgery31
10/13/20HNC Dysphagia Regardless of treatment approach for HNC, swallowfunction will rarely return to normal, without ANY longterm side effects Goals need to be patient-centered, realistic, andevidence-based May need to shift mindset, becoming “okay” with someaspiration with strategies to maximize swallowfunction/PO while limiting risk for aspiration relatedcomplicationsDepartment of Otolaryngology- Head and Neck Surgery4Goals of Assessment(s) Know as much as possible prior to start of treatment– Single modality vs multi-modality– Surgical plan and/or op note, if available– Radiation plan- at least # of treatments and areas targeted Be involved prior to treatment– Educate regarding possible/anticipated challenges– Initiate prophylactic strategies/exercises as indicated Assess for dysphagia and develop treatment plansDepartment of Otolaryngology- Head and Neck Surgery5Impact of Surgery62
10/13/20Tracheostomy Artificial airway placed through anterior neck into tracheaDepartment of Otolaryngology- Head and Neck Surgery7Tracheostomy &Dysphagia Presence of tracheostomy tubecan affect swallowing:– Reduced hyolaryngealelevation/excursion– Reduced subglottic airpressure– Reduced upper airwaysensitivityDepartment of Otolaryngology- Head and NeckSurgery8Tracheostomy & Dysphagia Passy-Muir Valve– One-way, closed position valve– Re-directs air up through larynx/pharynx– Re-establishes “closed system”Department of Otolaryngology- Head and Neck Surgery93
10/13/20Impact of Surgery Extent of dysphagia after surgery depends on what/where/howmuch resected Depends on manner of resection– Open procedure– Robotic Surgery– Laser Depends on manner of closure– Primary closure– ReconstructionDepartment of Otolaryngology- Head and Neck Surgery10Impact of SurgeryOral surgery mayresult in dysphagiad/t resection andreconstructionTongue surgery lingual range ofmotion, control,and strength maybe effecteddepending on theextent of thesurgeryDepartment of Otolaryngology- Head and Neck Surgery11Oral Surgery Therapeutic Strategies– Head position (chin tuck/chin extension)– Super-Supraglottic Swallow– Adaptive utensils/dishesDepartment of Otolaryngology- Head and Neck Surgery124
10/13/20PartialLaryngectomy Dysphagia varies based on the area/extent ofreconstruction and resection13Partial Laryngectomy Therapeutic Strategies– Head Turn– Super-supraglottic swallow– Swallow, cough, re-swallow– Liquid modifications– Diet modifications BioFEESback can be very beneficial for these patientsDepartment of Otolaryngology- Head and Neck Surgery14Total Laryngectomy Larynx and supraglottic structures surgically removed (truevocal folds, ventricular folds, epiglottis, hyoid bone) Neopharynx created with primary closure or reconstruction Trachea re-routed to the anterior neck to form a stomaDepartment of Otolaryngology- Head and Neck Surgery155
10/13/201617TL & Dysphagia Impairments related to total laryngectomy may include:– Reduced BOT-PPW contraction– Reduced neopharyngeal contraction – especially in cases requiring flapreconstruction– Reduced UES opening Compensatory Strategies:– Moist/slick foods– Utilize liquid wash– Head turn to one side or the other “Silver Lining”– Unless a fistula develops, patient can no longer aspirate*– Many patients return to a fairly normal dietDepartment of Otolaryngology- Head and Neck Surgery186
10/13/20Impact of Surgery Regardless of type of surgical procedure, important to getinstrumental swallow study to establish new swallow functionbaseline, risk of aspiration, and potential benefit ofcompensatory strategiesDepartment of Otolaryngology- Head and Neck Surgery19Impact of Radiation /- Chemo20DysphagiaAssociatedwith RT /Chemo A common effect with estimatedprevalence of 39-64% after RT or CRT(Hutcheson, 2013) A common complication for patientsboth acutely and long after treatmenthas ended (Kotz et al., 2012) Evidence to support that severity ofdysphagia depends on dose torelevant swallowing structures (i.e.,pharyngeal constrictors, esophagealinlet, glottic and supraglottic larynx) (K.Wopken et al., 2018)Department of Otolaryngology- Head and Neck Surgery217
10/13/20Importance ofSLPInvolvement Evidence to support that multidisciplinarycare for patients with HNC can result inbetter patient outcomes (Messing et al,2019) SLP’s involvement throughout thecontinuum of patient care promotes bestfunctional outcomes and best practices inHNC (Starmer & Edwards, 2019)– Enhance buy-in by providingpatient/caregiver counseling and rationale aswell as potential benefits to exercise regimen(Paleri et al, 2014)– Can positively impact patient attendance andadherence to swallowing recommendations(Starmer, 2014)Department of Otolaryngology- Head and Neck Surgery22UIHC SLP RT /- Chemo DysphagiaProtocol Pre- treatment:– Initial swallowing evaluation/education During treatment:– Weekly/Bi-weekly follow-up (max. 30 minutes) sessions Post-treatment:– Coordinated follow-ups with return appts to other teams– Repeat clinical assessments and instrumental assessments, asindicated– Therapy and/or appropriate referrals as indicatedDepartment of Otolaryngology- Head and Neck Surgery23RT /- ChemoDysphagiaManagement –Pre-treatment Goals:– Establish relationship/rapport prior toinitiation of treatment Establish patient goals– Assess baseline swallow function,functional nutritional status, patientperceived dysphagia Poor correlation between measurabledysphagia and patient perception (Starmer,2014)– Provide education and managementstrategies re: anticipated treatment-relatedtoxicities affecting swallow function and POintake as well as swallow exercisesDepartment of Otolaryngology- Head and Neck Surgery248
10/13/20InitialSpeechLanguagePathologyVisit Chart review:– Type, stage, location– Previous treatment – surgery, RT /Chemo If RT /- Chemo, treatment plan (i.e., dose,treatments, targeted areas) Patient interview: Reported dysphagia,need to modify foods/liquids, need forsupplemental shakes/enteral nutrition Gather quantitative data regardingpatient-reported dysphagia and POintakeDepartment of Otolaryngology- Head and Neck Surgery25Patient Self-Assessment ToolsEAT-10 (Belafsky et al., 2008)Department of Otolaryngology- Head and Neck Surgery26Patient Self-Assessment ToolsMD Anderson DysphagiaIndex (MDADI)Department of Otolaryngology- Head and Neck Surgery279
10/13/20Clinician-Rated AssessmentsDepartment of Otolaryngology- Head and Neck Surgery28Clinician-Rated AssessmentsPerformance Status Scale- HNC(PSS-HNC)Department of Otolaryngology- Head and Neck Surgery29InitialSpeechLanguagePathologyVisit Oral mechanism exam Clinical/bedside swallow study Possible instrumental swallow study viaOropharyngeal Motility Study (OPMS) orFiberoptic Endoscopic Evaluation ofSwallowing (FEES)– May be recommended initially based on tumorlocation and/or stageDepartment of Otolaryngology- Head and Neck Surgery3010
10/13/20OROPHARYNGEALMOTILITY STUDY(OPMS)AKA: “COOKIESWALLOW” Instrumental evaluation of swallowingusing videofluoroscopy Administer barium of varyingconsistencies to assessoropharyngeal swallow function, riskof aspiration, and inform treatmentplanning Allows view of function in oral,pharyngeal, and esophageal phasesbefore, during, and after swallowDepartment of Otolaryngology- Head and Neck Surgery31OROPHARYNGEALMOTILITY STUDY(OPMS)AKA: “COOKIESWALLOW” Not a “pass/fail” evaluation– Martin-Harris, et al (2000): reviewof 608 swallow studies-10.4%normal, 32.4% with aspiration,57.2% abnormal but noaspiration Used as a therapeuticinstrument to test benefit ofcompensatory strategies Used as a tool to maximizeefficiency and safety of swallowfunctionDepartment of Otolaryngology- Head and Neck Surgery32Fiberoptic Endoscopic Evaluation ofSwallowing (FEES) Instrumental assessment using flexible laryngoscope Administer real food consistencies dyed an artificialcolorto assess oropharyngeal swallow function, risk ofaspiration, and inform treatment planning Allows for view of anatomical structures and tissue Allows for view of presence/absence of pooledsecretions Cannot view pharynx/larynx during a “normalswallow”Department of Otolaryngology- Head and Neck Surgery3311
10/13/20Fiberoptic Endoscopic Evaluation ofSwallowing (FEES) Not a “pass/fail” evaluation Used as a therapeutic instrumentto test benefit ofcompensatory strategies Used as a tool to maximizeefficiency and safety ofswallow functionDepartment of Otolaryngology- Head and Neck Surgery34Not a ”pass/fail” evaluation! Goal is to limit risk of aspiration-related complications, not JUSTto eliminate aspiration Attempt strategies and/or maneuvers to maximize safety andefficiency– Chin tuck, chin extension– Head turn L, R ( /- chin tuck)– (Super)Supraglottic Swallow– Double swallow– Effortful swallow– Swallow/cough/re-swallowDepartment of Otolaryngology- Head and Neck Surgery35Not a ”pass/fail” evaluation! Educate other participants in the study about the rationale forcontinuing despite observed aspirationDepartment of Otolaryngology- Head and Neck Surgery3612
10/13/20InitialSpeechLanguagePathologyVisit Oral mechanism exam Clinical/Bedside swallow study Possible instrumental swallow study via Fiberoptic EndoscopicEvaluation of Swallowing (FEES) or Oropharyngeal Motility Study(OPMS)– May be recommended initially based on tumor location and/orstage Provide PO recommendations based on results and anticipatedchanges during treatment course – NPO as last resort Provide education regarding 3 main RT toxicities likely to affectswallowing/PO intake during treatment course– Odynophagia (painful swallowing)– Dysgeusia/hypogeusia (taste changes/reduced taste)– Xerostomia (dry mouth)Department of Otolaryngology- Head and Neck Surgery37InitialSpeechLanguagePathologyVisit Oral mechanism exam Clinical/Bedside swallow study Possible instrumental swallow study viaFiberoptic Endoscopic Evaluation of Swallowing(FEES) or Oropharyngeal Motility Study(OPMS)– May be recommended initially based on tumorlocation and/or stage Provide recommendations based on results andanticipated changes during treatment course Educate regarding 3 main RT toxicities likely toaffect swallowing/PO Teach prophylactic swallowing exercisesDepartment of Otolaryngology- Head and Neck Surgery38 Less PO intake less resistive load onswallow musculature, proactive swallowtherapy aims to maximize use of swallowmusculature during RT or CRT (Hutcheson,2013) Targeting swallowing habilitation vsrehabilitation Swallowing exercise program targets areas ofimpairment and/or areas most likely to beaffected based on RT treatment planProphylacticSwallowingExerciseProgram Start prior to or as close to beginning oftreatment as possibleDepartment of Otolaryngology- Head and Neck Surgery3913
10/13/20“Pharyngocise” – Carnaby-Mann, Crary, Schmalfuss, Amdur, 2012 One of the first RCT of systematic program of swallowingexercises during CRT 58 HNC Patients– Oropharyngeal cancer– External beam radiation planned– No hx of non-oral feeding for cancer-related illness– Able to undergo MRIDepartment of Otolaryngology- Head and Neck Surgery40“Pharyngocise” – Carnaby-Mann, Crary, Schmalfuss, Amdur, 2012 Primary Outcome– Muscle size and composition determined by t2 –weighted MRI Secondary Outcomes– Functional swallowing ability, dietary intake, chemosensory function,salivation, nutritional status, occurrence of dysphagia-relatedcomplicationsDepartment of Otolaryngology- Head and Neck Surgery41“Pharyngocise” – Carnaby-Mann, Crary, Schmalfuss, Amdur, 2012 3 groups– ”Usual Care”– Sham– High-intensity swallow therapy group (“Pharyngocise”)Department of Otolaryngology- Head and Neck Surgery4214
10/13/20“Pharyngocise” – Carnaby-Mann, Crary, Schmalfuss, Amdur, 2012 Primary Outcome Results– All groups demonstrated muscle deterioration during treatment, butgreatest preservation noted in Pharyngocise group for genioglossus,hyoglossus, and mylohyoidDepartment of Otolaryngology- Head and Neck Surgery43“Pharyngocise” – Carnaby-Mann, Crary, Schmalfuss, Amdur, 2012 Secondary Outcomes Results– Functional Swallowing- No significant differencebetween groups, however better median score inPharyngocise group– Better maintenance of oral intake/less PEG tubeplacement in Pharyngocise vs usual care– Less decline in taste and smell in Pharyngocisegroup– Significant preservation of salivary flow inPharyngocise group– Weight loss not significantly different between groups– No significant associations between dysphagiarelated complications and treatment groupDepartment of Otolaryngology- Head and Neck Surgery44“Pharyngocise” – Carnaby-Mann, Crary, Schmalfuss, Amdur, 2012–Conclusion Results suggest participation in swallow exerciseprogram during C/RT yield better maintenance ofhead and neck musculature and improved functionalswallowing outcomes Interestingly, benefits were seen in both Pharyngociseand sham groupsDepartment of Otolaryngology- Head and Neck Surgery4515
10/13/20“Use it or Lose it”- Hutcheson, et. al 2013 Retrospective observational study 497 HNC patients– Pharyngeal cancer (oropharyngeal or hypopharyngeal)– Treated with RT or CRTDepartment of Otolaryngology- Head and Neck Surgery46“Use it or Lose it”- Hutcheson, et. al 2013 Swallowing end-points:– Final diet after RT or CRT– Length of PEG dependence Independent variables:– Oral intake at the end of RT or CRT (no oral intake, partial intake, fullintake)– Adherence to swallow exercise programDepartment of Otolaryngology- Head and Neck Surgery47“Use it or Lose it”Hutcheson et al 2013 Final diet results– Eat Exercise 92%regular diet at 24months s/p fin– NPO no exercise 65% regular diet at24 months s/p finDepartment of Otolaryngology- Head and Neck Surgery4816
10/13/20“Use it or Lose it”Hutcheson et al 2013 PEG DependenceResults– NPO no exercise median 222 days (33– 1781)– Partial PO exercise median 111 days (0– 2029)Department of Otolaryngology- Head and Neck Surgery49Take Home Messages – Rad /- Chemo Involvement of SLPs can be beneficial to patient outcomes indysphagia associated with C/RT management of HNC Ideal for patients to take full PO diet and full regimen ofswallowing exercises during C/RT, but some is better than none Ongoing research is warranted to define/refine best practiceguidelines for best patient outcomesDepartment of Otolaryngology- Head and Neck Surgery50Take Home Messages Dysphagia related to surgical management depends on avariety of factors and visualization of swallow function is critical Dysphagia related to radiation /- chemo therapy is commonand our involvement can be very beneficial Patient-centered care is important and overarching goals needto be centered on maximizing PO and limiting risk of aspirationrelated complicationsDepartment of Otolaryngology- Head and Neck Surgery5117
10/13/20Department of Otolaryngology- Head and Neck SurgeryQuestions?Brian Peterson, MA, CCC-SLPSpeech-Language Pathologist IIDepartment of Otolaryngology –Head and Neck Surgerybrian-e-peterson@uiowa.eduuihc.orgCHANGING MEDICINE.CHANGING LIVES. 52References Belafsky, P. C., Mouadeb, D. A., Rees, C. J., Pryor, J.C., Postma, G. N., Allen, J., & Leonard, R. J. (2008).Validity and reliability of the Eating Assessment Tool(EAT-10). The Annals of otology, rhinology, andlaryngology, 117(12), 919–924. Carnaby-Mann, G., Crary, M. A., Schmalfuss, I., &Amdur, R. (2012). "Pharyngocise": randomizedcontrolled trial of preventative exercises to maintainmuscle structure and swallowing function during headand-neck chemoradiotherapy. International journal ofradiation oncology, biology, physics, 83(1), 210–219. Crary, M. A., Mann, G. D., & Groher, M. E. (2005). Initialpsychometric assessment of a functional oral intakescale for dysphagia in stroke patients. Archives ofphysical medicine and rehabilitation, 86(8), 1516–1520.Department of Otolaryngology- Head and Neck Surgery53References Hutcheson, K. A., Bhayani, M. K., Beadle, B. M.,Gold, K. A., Shinn, E. H., Lai, S. Y., & Lewin, J.(2013). Eat and exercise during radiotherapy orchemoradiotherapy for pharyngeal cancers: use itor lose it. JAMA otolaryngology-- head & necksurgery, 139(11), 1127–1134. Kotz, T., Federman, A. D., Kao, J., Milman, L.,Packer, S., Lopez-Prieto, C., Forsythe, K., &Genden, E. M. (2012). Prophylactic swallowingexercises in patients with head and neck cancerundergoing chemoradiation: a randomizedtrial. Archives of otolaryngology--head & necksurgery, 138(4), 376–382.Department of Otolaryngology- Head and Neck Surgery5418
10/13/20References Messing, B. P., Ward, E. C., Lazarus, C., Ryniak, K., Kim, M.,Silinonte, J., Gold, D., Thompson, C. B., Pitman, K. T., Blanco, R.,Sobel, R., Harrer, K., Ulmer, K., Neuner, G., Patel, K., Tang, M., &Lee, G. (2019). Establishing a Multidisciplinary Head and NeckClinical Pathway: An Implementation Evaluation and Audit ofDysphagia-Related Services and Outcomes. Dysphagia, 34(1), 89–104. https://doi.org/10.1007/s00455-018-9917-4 Paleri, V., Roe, J. W., Strojan, P., Corry, J., Grégoire, V., Hamoir,M., Eisbruch, A., Mendenhall, W. M., Silver, C. E., Rinaldo, A.,Takes, R. P., & Ferlito, A. (2014). Strategies to reduce long-termpostchemoradiation dysphagia in patients with head and neckcancer: an evidence-based review. Head & neck, 36(3), 431–443. Starmer, Heather M. Dysphagia in head and neck cancer:prevention and treatment, Current Opinion in Otolaryngology &Head and Neck Surgery: June 2014 - Volume 22 - Issue 3 - p 195200 Starmer, H., & Edwards, J. (2019). Clinical Decision Making withHead and Neck Cancer Patients with Dysphagia. Seminars inspeech and language, 40(3), 213–226.Department of Otolaryngology- Head and Neck Surgery55References Wopken, K., Bijl, H. P., & Langendijk, J. A.(2018). Prognostic factors for tube feedingdependence after curative (chemo-) radiation inhead and neck cancer: A systematic review ofliterature. Radiotherapy and oncology : journalof the European Society for TherapeuticRadiology and Oncology, 126(1), 56–67.Department of Otolaryngology- Head and Neck Surgery5619
Department of Otolaryngology -Head and Neck Surgery Oral surgery may result in dysphagia d/t resection and reconstruction Tongue surgery - lingual range of motion, control, and strength may be effected depending on the extent of the surgery