Transcription
MALNUTRITIONThe Changing Landscape of DocumentationSzilvia Kovacs MS, RD, LDN
DisclosureI do not have any affiliation and have not received any financialsupport from any organization that could potentially bias thispresentation.
ObjectivesThis presentation will:1. Define and discuss malnutrition as it relates to hospitalized patients.2. Review the impact of malnutrition on quality outcomes.3. Identify steps to implement a malnutrition documentation program.4. Discuss the newest changes to malnutrition criteria and what thesechanges may mean for clinical nutrition practice.5. Provide tools for audit readiness and review a potential auditprocess for malnutrition documentation.
“The recognition and the understanding of how todiagnose and treat malnutrition could likely change thefuture of health care not just in this country but aroundthe world.”Dr. Paul Wischmeyer
DefinitionMalnutrition is inadequate intake of energy and/orprotein over a period of time resulting in weight loss,lean body mass loss, loss of fat stores and diminishedfunctionality.5
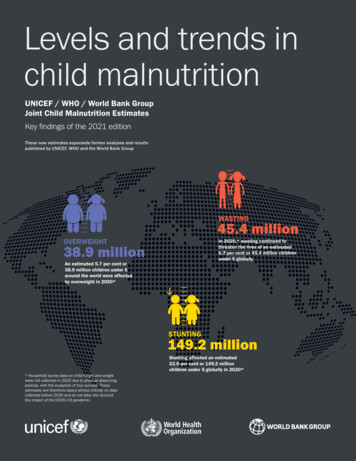
Prevalence of MalnutritionHeathcare SettingPrevalenceHospital (1 in 3 patients)20-50%Long-term care21-51%Outpatient/Homecare13-30% Older adults 65 : as much as 65% can be malnourished in the hospitalsetting. 31% of malnourished patients and 38% well nourished patients experiencenutritional decline during their hospital stay.References 2,5,66
Implications of Malnutrition Delayed wound healing Dehydration Pressure ulcers Alteration in gait/balance, increasedrisk of falls and fractures Functional decline Susceptibility to infections Decreased muscular strength andaerobic capacity leading to chronicfatigue Depression Decreased lean body mass Delayed recovery from illness Deterioration in overall quality of life Difficulty in swallowing Dependence on others Cognitive declineQuality Metrics
Malnutrition and Patient Outcomes
Healthcare TransformationFrom FEE FOR SERVICE payment model Provider is paid based onvolume of service QUALITY BASED payment methodologies Promotes quality of careand better outcomes.Example: Risk Adjustment Factor – methodology predict healthcare cost Takes into account chronic conditions Insurance company receives compensation if enrolling greater thanaverage number of individuals w/ high risk.
ICD – 10 Coding Structure
Hierarchical Condition Categories
Historical Dilemma Providers not identifying and capturing the diagnosis of malnutrition. Variation in clinical criteria used by providers to diagnosemalnutrition No standardization of criteria for malnutrition among providers andinterdisciplinary team Lack of criteria to determine severity of malnutrition -mild, moderateor severe protein calorie malnutrition Providers not aware of National Best Practice Guidelines to diagnosemoderate and severe protein–calorie malnutrition and uncertain ofhow and when to use diagnosis
Malnutrition InitiativeGOAL: Collaboration and consistency in documentation** To apply best practice guidelines via multidisciplinary route whenidentifying, diagnosing &treating malnutrition to promote positive patient outcomes.1. Early identification & intervention for patients identified with malnutritionand post-discharge care planning2. Accurate patient profiling/clinical documentation Better patient careand outcomes Quality Reporting (*establish baseline prevalence)3. Reduce risk of error, potential audit issues, red flags etc.13
Implementation Process1. Enlistadministrative support Best practice, evidence-based Improvement in quality reporting Reimbursement impact2. Build multidisciplinary team – Educate, Educate, Educate!– RD– HIM – CDI and Coding– Information Systems– Ancillary departments – Nursing and Integrated Case Management– Physician Champions3. Electronic communication tool between RD and Provider – best practice!4. Medical Executive Committee approval of hospital-wide criteria and electroniccommunication tool.
SELECTING A SCREENING TOOL
MalnutritionScreeningTool
SELECTING A CRITERIA
ASPEN CriteriaPublished National Guidelines (2011) - the evidenced based criteria developed by theAcademy and ASPEN, to identify and diagnose malnutrition:6 Clinical Characteristics– Insufficient food intake compared with nutrition requirements– Weight loss over time– Loss of muscle mass– Loss of subcutaneous fat mass– Localized or generalized fluid accumulation (may mask weight loss)– Measurably diminished grip strength (result of loss in functional status)**Patient must have two or more of the 6 characteristics**
ASPEN Criteria – widely used
GLIM: The Global Leadership Initiative onMalnutrition Founded in January of 2016 Consists of: leadership from ASPEN, ESPEN and a variety of nutritionsocieties from Asia, Latin America and Australia GOAL/Intent: create a minimum set of malnutrition diagnostic criteria that isendorsed and used globally. Two-Step Model:– Risk Screening (Example - MST)– Diagnosis Assessment (Diagnosis and Severity)
Diagnosis Classification Based On Etiology
Diagnostic Scheme by GLIM
Criteria to UsePhenotypic(Effects and Degree)Etiologic (Drives Interventions) Nonvolitional weight loss:– 5% within past 6 months– 10% beyond 6 months Reduced food intake or assimilation: 50%of ER(energy requirements) for 1 week, orany reduction for 2 weeks, or any chronicGI condition that adversely impacts foodassimilation or absorption. Further definesto consider GI symptoms and malabsorptivedisorders. Low BMI: is different from CDC, USDepartment of Health & HumanServices: NIH definition of underweight 18.5; ICD-10-CM Z68.1 BMI of19.9 or less– 20 if 70 y/o– 22 if 70 y/o Reduced Muscle Mass: GLIM:recommends measure by Dual-energyabsorptiometry, bioelectricalimpedance, ultrasound, computedtomography, MRI, mid-arm muscle orcalf muscle circumference, hand-gripstrength Disease burden/inflammation:– Acute disease/injury: severeinflammation: major infections, burns,trauma, CHI. CRP may be used– Chronic disease-related: mild to modinflammation: malignant dz, COPD,CHF, CRF, or any dz with chronic orrecurrent inflammation. CRP may beused
GLIM Criteria for the Diagnosis of MalnutritionMUST have 1 phenotypic and 1 etiologic criteria to diagnose the PRESENCE ofmalnutrition.Phenotypic CriteriaEtiologic CriteriaWeight Loss (%)Low BMI(kg/m2)Reduced Muscle MassReduced Food Intake orAssimilationInflammation 5% w/in past 6 moor 10% beyond 6 mo 20 if 70 yearsor 22 if 70 yearsReduced by validatedbody compositionmeasuring techniques50% of ER 1 weekorAny reduction for 2 wksorAny chronic GI conditionthat adversely impactsfood assimilation latedAsia: 18.5 if 70 yrsor 20 if 70 yrs
Thresholds for Severity Grading of MalnutritionPhenotypic CriteriaWeight Loss (%)Low BMI(kg/m2)Reduced Muscle MassStage 1/moderate malnutrition(requires 1 phenotypic criterionthat meets this grade)5% 10% w/in the past 6 moor10% 20% beyond 6 mo 20 if 70 yrs 22 if 70 yrsMild-to-moderate deficit(per validated assessmentmethods)Stage 2/severe malnutrition(requires 1 phenotypic criterionthat meets this grade) 10% within the past 6 moor 20% beyond 6 mo 18.5 if 70 yrs Severe deficit (per validated 20 if 70 yrsassessment methods)**For Reduced muscle mass:Dual-energy absorptiometry or corresponding standards using other body composition methods such asbioelectrical impedance analysis, computed tomography, or magnetic resonance imaging. When notavailable or by regional preference, physical examination or standard anthropometric measures such asmid-arm muscle or calf circumferences may be used. Functional assessments such as hand-gripstrength may be used as a supportive measure.
GLIM Summary Table (Must have one of each main criteria)Phenotypic CriteriaEtiologic CriteriaWeight Loss(%)BMI(kg/m2)ReducedMuscleMassPO intakeInflammationModerateMalnutr.5% 10% w/inpast 6moor10% 20%6mo 20 if 70 yrs 22 if 70 yrsMild-tomoderatedeficit50% of ER 1 weekorAny reduction for 2 wksorAny chronic GI condition thatadversely impactsfood assimilation or absorptionAcutedisease/injury orchronicdisease-relatedSevereMalnutr. 10% w/inpast 6moor 20% beyond6mo 18.5 if 70 yrs 20 if 70 yrsSeveredeficit50% of ER 1 weekorAny reduction for 2 wks orAny chronic GI condition thatadversely impactsfood assimilation or absorptionAcutedisease/injury orchronicdisease-related
Next StepsFor GLIM: Must be properly vetted on a global scale based on collectivefeedback. Validation studies to be performedFor Practitioners:Educate Collaborate Document
Key Elements in DocumentationE43 Severe - Protein Calorie Malnutrition Hardly ever a Primary DiagnosisMost common cause for denial: Insufficient and/or ONE timedocumentation to support the billing of diagnosis code 43 - Severe proteincalorie malnutrition.Documentation must haves are: Appropriate screening (Validated Screening Tool such as MST?) Clinical evaluation & Therapeutic treatment Diagnostic procedure (consider utilization of objective musclemeasurements) Discharge plan for nutritional needs
Key Elements in Documentation con’t1. Should NOT be a one-time diagnosis!2. Physical appearance – muscle wasting, fat losses, cachexia, emaciation.3. Include ALL body areas examined or observed in your diagnosis!-- “Patient refused nutrition focused physical assessment at this time.”4. History of nutritional intake – (degree and timeframe)5. Reduced functional capacity (“Weakness” is not objective enough)6. Unintended weight loss (Degree and time frame)a. Insure reference weight is documented (Usual Body Weight)7. Supportive items: Non-healing wound, micronutrient deficiencies, BMI should all beincluded in documentation.8. Documentation among healthcare professionals should be CONSISTENT throughoutthe medical record.
Golden Rule“If it’s not documented by thephysician/provider, it didn’t happen.”
References1. Coats KG et al. J Am Diet Assoc 1993; 93: 27-33; Giner M et al. Nutrition 1996; 12: 23 29; Thomas DR et al. Am J ClinNutr 2002; 75: 308-313; Somanchi M, et al. JPEN. 2011; 35:209-216; Guigoz Y. J Nutr Health Aging. 2006; 10:466-487.Jensen GL, et al. JPEN J Parenter Enteral Nutr. 2010;34:156-159.2. Aging Network Staff. Malnutrition and Older American. National Resource Center on Nutrition, PhysicalActivity & Aging. Available at:http://nutritionandaging.fiu.edu/aging network/malfact2.asp. Accessed February 3, 2015.3. Fingar KR, Weiss AJ, Barrett ML, et al. All-Cause Readmissions Following Hospital Stays for Patients withMalnutrition, 2013. HCUP Statistical Brief #218. December 2016. Agency for Healthcare Research andQuality, Rockville, MD. 218-MalnutritionReadmissions-2013.pdf.4. Braunschweig C, et al. J Am Diet Assoc. 2000;100 (11):1316-1322. Impact of declines in nutritional statuson outcomes in adult patients hospitalized for more than 7 days.5. Barker LA et al. Hospital malnutrition: Prevalence, identification, and impact on patients and thehealthcare system. Int J of Environ Res and Public Health. 2011;8:514-527.6. Weiss AJ et al. Characteristics of Hospital Stays Involving Malnutrition, 2013. HCUP Statistical Brief #210.Rockville, MD: Agency for Healthcare Research and Quality. Available at: 10-Malnutrition-Hospital-Stays-2013.pdf. Accessed March 18, 2016.32
References con’t7. Guenter P et al. The Joint Commission Journal on Quality and Patient safety 2015; 41(10): 469-473. Addressing Disease-Related Malnutrition in Hospitalized Patients: A Call for aNational Goal8. Using Outcomes Data to Advocate for the Nutrition Care Process presented byBridget Drapeaux, MA, RDN, LD, Abbott Nutrition. Retrieved from www.anhi.org.9. 2014 Alliance to Advance Patient Nutrition; www.malnutrition.com10. www.cms.gov11. https://www.novitas-solutions.com/12. Novitas Solutions Medicare Part A Presents: Targeted Probe and Educate: E43 – Severe – ProteinCalorie Malnutrition; June 27, 201813. Jensen GL et al. GLIM Criteria for the Diagnosis of Malnutrition: A Consensus Report From theGlobal Clinical Nutrition Community Journal of Parenteral and Enteral Nutrition. 2018;0:1–9.14. Cederholm T, et al., GLIM criteria for the diagnosis of malnutrition e A consensus report from the global clinicalnutrition community, Clinical Nutrition (2018), https://doi.org/10.1016/j.clnu.2018.08.002
Sep 08, 2019 · inflammation: malignant dz, COPD, CHF, CRF, or any dz with chronic or recurrent inflammation. CRP may be used. GLIM Criteria for the Diagnosis of Malnutrition MUST have 1 phenotypic and 1 etiologic criteria to diagnose the PRESENCE of maln