Transcription
Beyond Intent, Plan, andAccess to Means: BasicInterventions for AdvancedAssessmentsREAL LIFE CRISIS WORKERS WITH A NERDY STREAK
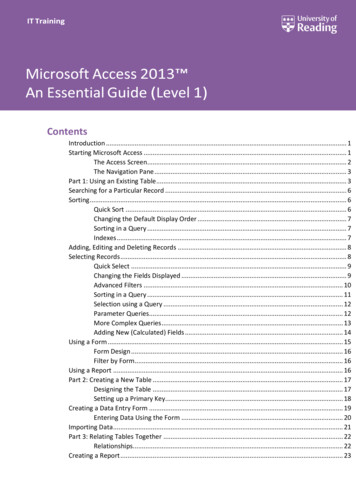
SUICIDE/DEPRESSION SCREENING TOOLS!ACORN!COLUMBIA SUICIDE SCREENING!SAFE-T!PHQ-9!ASQ!SAD PERSONS!Beck Hopelessness Scale!AND MOREALERT TO RISK BUT DON’T RESOLVE SITUATION
Our focus today is to introduce or reviewinterventions that will aid the clinician inhaving a collaborative conversation with theclient. These conversations are vital inunderstanding the critical details of anindividual’s suicidal crisis and leading to anappropriate and safe outcome.
GOALS FOR SUICIDE ASSESSMENTS!We have found that most suicide assessments in our world have two goals:!Determining the current degree of risk based on history, current symptoms/behaviors, and demographics !Static verses dynamic risk factorsSwiftly building a therapeutic alliance with the client that may provide enoughshort-term relief from their pain to avoid hospitalization and safely carry them tothe next stage of treatment
Barriers to Suicide Assessments!The assessor’s mental state!Arousal!Vicarious trauma!Countertransference!!The Suicidal Patient and Countertransference Hate by John Malsberger and Daniel Buie(1974)Sparse information!Little is known about the client due to a lack of records or people to interview!Client, friends, or family can have a difficult time remembering details!Because they weren’t important, memory loss due to trauma (physical or emotional), dueto natural forgetting, due to an individual being “activated” (mid-brain vs. frontal lobe)
Barriers to Suicide Assessments
Barriers to Suicide Assessments!Secondary Gains!!Clients, their friends, and their family can have secondary gains, such as:!Emotional needs!Physical needs!Protectiveness (client’s protecting someone and vice versa)Client is guarded or misrepresenting information!Due to shame!Stigma!Cultural attitudes!Psychosis and paranoia!High intent to suicide
Interventions with the client –The fluidity of the assessment.Rapport building, assessing, and moving at the same time.
“I believe the greatest gift I canconceive of having from anyone is to beseen by them, heard by them, to beunderstood and touched by them”– Virginia Satir
“In my early professional years I was askingthe question: How can I treat, or cure, orchange this person? Now I would phrase thequestion in this way: How can I provide arelationship which this person may use for hisown personal growth?”– Carl Rogers
3:00 am in the Emergency Room
Assessor’s Attitude and Presentation!Cash Metaphor – Build credit to spend later!Gentle and unconditional positive regard vs. detachedinformation gathering!Calm demeanor, calm voice!Acknowledging the client’s experience while advocating for change
Relationship Building Interventions!Slow it down! Time is your friend.!Reflective listening/empathic reflection!Affirming for change. Acknowledge the difficulty of theclient’s situation and affirm feelings but then advocate forchange!Genuineness!Open ended questions
Information Gathering and ClinicalConceptualization Interventions!!Shame Attenuation!Phrasing questions, the answers to which, help to alleviate any possible judgement. The question isasked from the client’s own framework and rationale!Example: “That sounds really lonely. With all those feelings of loneliness, have you ever consideredkilling yourself?”Gentle Assumptions!Asking as if a given behavior has occurred as opposed to asking whether or not it has occurred!Example: “How many times have you tried to suicide in the past?” vs. “Have you ever tried to suicide?”!Also, looking for subtle assumptions the client may be making (“The last time this happened, it never gotthis out of hand”)
Information Gathering and ClinicalConceptualization Interventions!!Normalization!Helping the client feel “normal” by placing their experience in perspective withothers who have had similar experiences!Example: “Sometimes when people talk about feeling hopeless or about death, theyare thinking about suicide. Are you having thoughts of suicide?”Symptom Amplification!Limiting a client’s tendency to minimize certain behaviors by setting an overstatedupper limit!Example: “How much alcohol do you drink daily? A fifth? A half-gallon?”!Setting the upper limit helps to address possible reluctance to share informationdue to fear of judgement and helps to make the conversation seem like it’s morecommonplace
Information Gathering and ClinicalConceptualization Interventions!!Denial of Specific!Soliciting information which can only have a binary (yes/no) response!Example: “How many drugs have you used?” vs “Have you ever used THC? Meth? Heroin?”Behavioral Incident!Ask the client about the concrete details of the suicide attempt while avoiding emotional orinterpretive accounts!!!!!!!!Focus on the concrete events and drilling down to the specifics of what happenedAt what point did you decide you were going to kill yourselfWhat thoughts did you have when you decided to kill yourself?Did you harm yourself with the intention of killing yourself? What was your goal in trying to harm yourself?How were you discovered/who called for help?How long had you been thinking about killing yourself? Have you been thinking about doing this for a whileor was this something you thought of in the moment?Was anyone else with you when you tried to kill yourself?What was the means by which you tried to kill yourself? Exactly how and in what way?!!!Identify the number of pills, the speed of the car, the height of the bridge, the strength of the rope/the hangingapparatus, or the depth/extent of the cutsLesser lethality means DOES NOT necessarily mean lower level risk of suicide“and then what happened?”
Information Gathering and ClinicalConceptualization Interventions!Identifying Causal Factors!Determining the events andcircumstances which have initiated thecrisis!Example: “What happened TODAY thatbrought you in to the EmergencyDepartment?” “When did you decide tokill yourself?”!Shae’s CASE Model: ChronologicalAssessment of Suicide Events
Information Gathering and ClinicalConceptualization Interventions!Cross Referencing Information!Comparing information from all sources, including:!!Client and collateral cials/index.html!Historical records!Verbal and non-verbal cluesFinding discrepancy and determining validity!Internal Validity – The client’s account makes sense with other elements of their account!External Validity – The client’s account makes sense with other known facts and accountsabout the case
Internal Validity – Does the article make sense with itself?External Validity – Does the article make sense with other articles?
Information Gathering and ClinicalConceptualization Interventions!Leveling with the Client!Helping the client make an informed decision by giving them an account of the current situation, possiblechoices, and the impact of their choices!Can be helpful if client is “stonewalling” or not providing any information!Example: “I want to help you but if we’re not able to figure out what happened then we might beobligated to hold you in the emergency department until we can make sure you’re safe”! NO!THREATENING!!!Non-Confrontational Resolution of Discrepancy!Making sense of facts which seem inconsistent or contradictory while maintaining therapeutic rapport!Example: “Help me understand” or “I’m confused”
Information Gathering and ClinicalConceptualization Skills
Information Gathering and ClinicalConceptualization Interventions!Scaling Questions!Assertive Consultation!!Consult, consult, consult, then document!Wake ‘em up, interrupt the meeting, make the phone call!Consultation is like looking at the blind spot in your car. If you’re only looking through yourown vantage point without changing your perspective, it’s more likely something will bemissed in your blind spotObserve Countertransference!Countertransference is evidence.!Does something feel off? Not adding up? Look into it.
Interventions to Promote Client Change! Compliments/encouragement! Reducingcognitive constriction by helping the client toenvision alternatives besides suicide! Reducing! Youcognitive fusionare not your thoughts! MiracleQuestion! CopingQuestion! Howdo you cope?
Interventions to Promote Client Change!Findexceptions to the problem! Havethere ever been times when the problem wasless difficult than it is now?!Elicitingchange talk! Elicitingefficacy!Develop! Partself-motivating statements to build self-discrepancy and highlight ambivalenceof you wants to be done but I also sense that partof you
10 Commonalities in the Majority ofSuicides (Shneidman)!The common goal of suicide is cessation of consciousness!The common purpose of suicide is to seek a solution!The common stimulus of suicide is unbearable psychological pain!The common stressor in suicide is frustrated psychological needs!The common emotion in suicide is hopelessness-helplessness!The common cognitive state in suicide is ambivalence!The common perceptual state in suicide is constriction!The common action in suicide is escape!The common interpersonal act in suicide is communication of intention!The common pattern in suicide is consistency of lifelong styles
Interventions to Promote Client Change!General psychoeducation about distress tolerance and coping skills!Accepting distressing emotions or sensations!!Grounding techniques!!Counting tiles on the floor, listing as many states as they can remember, finding colors in the room,etc.Regulation of the nervous system!!Example: “You don’t have to like it but that’s the way it is” or “It doesn’t make it right, it makes itreal”Diaphragmatic breathing, progressive muscle relaxation, guided meditation, yoga, a warm bath,exercise, etc.Distraction techniques!Focusing on “no emotion lasts forever”!Watch TV, read a book, listen to music, play a board game, talk to a friend, go shopping, etc.
Barriers to Suicide Assessments
Interventions with the System!Advocacy for the clientWith police, with the hospital, with inpatient treatment, with family,etc.! Find resources within community!!Navigating systems with/for the clientInsurance coverage and programs! OHP presumptive!!Advocacy does not require knowing it all.Psychoeducation about suicide, educating individuals about suicide,planning with family and friends about suicidal risk, etc
Selected Bibliography!AMSR Task Force (2014). Assessing and Managing Suicidal Risk: Core Competencies forBehavioral Health Professionals [Training Manual]. Developed by the Suicide PreventionResource Center Education Development Center!Linehan, M. (1993). Special Treatment Strategies for Crisis and Suicidal Behaviors.In Cognitive-Behavioral Treatment of Borderline Personality Disorder. New York: TheGuilford Press.!Malsberger, J., & Buie, D. (1974). The Suicidal Patient and CountertransferenceHate. Archive of General Psychiatry, 30(5), 625-633.!Pisani, A. R., Murrie, D. C., & Silverman, M. M. (2015). Reformulating Suicide RiskFormulation: From Prediction to Prevention. Academic Psychiatry.!Podolak, E. (2015). Suicide Risk Assessment: Searching for True Positive. InternationalJournal of Adolescent Medicine and Health, 27(2).!Roos, L., Sareen, J., & Bolton, J. M. (2013). Suicide Risk Assessment Tools, PredictiveValidity Findings and Utility Today: Time for a Revamp? Neuropsychiatry, 3(5).
Selected Bibliography!Shea, S. C. (2011). The Practical Art of Suicide Assessment: A Guide for MentalHealth Professionals and Substance Abuse Counselors. Lexington, KY: MentalHealth Presses.!Shea, S. C. (2017). Psychiatric Interviewing: The Art of Understanding: APractical Guide for Psychiatrists, Psychologists, Counselors, Social Workers,Nurses, and Other Mental Health Professionals. New York: Elsevier!Shea, S. C. (2009). Uncovering Suicidal Intent: A Sophisticated Art and Usingthe Chronological Assessment of Suicide Events (CASE Approach). PsychiatricTimes, 26(12).!Shneidman, E. S. (1998). The Suicidal Mind. New York: Oxford University Press.!Suicide Prevention Resource Center. Counseling on Access to Lethal Means[Online Training Module]. https://training.sprc.org/enrol/index.php?id 20
OHP presumptive Advocacy does not require knowing it all.! Psychoeducation about suicide, educating individuals about suicide, . In Cognitive-Behavioral Treatment of Borderline Personality Disorder. New York: The Guilford Press. ! Malsberger, J., & Buie