Transcription
Journal ofEndocrinologyJ Rodriguez andN M DelzenneGut microbiome, fat mass andskeletal muscles249:1R1–R23REVIEWModulation of the gut microbiota-adiposetissue-muscle interactions by prebioticsJulie Rodriguez and Nathalie M DelzenneMetabolism and Nutrition Research Group, Louvain Drug Research Institute, UCLouvain, Université catholique de Louvain, Brussels, BelgiumCorrespondence should be addressed to N M Delzenne: nathalie.delzenne@uclouvain.beAbstractThe gut microbiota is now widely recognized as an important factor contributing tothe regulation of host metabolic functions. Numerous studies describe an imbalancein the gut microbial ecosystem in response to an energy-dense diet that drives thedevelopment of metabolic disorders. In this context, the manipulation of the gutmicrobiota by food components acting as prebiotics appears as a promising strategy.Several studies have already investigated the beneficial potency of prebiotics, mostlyinulin-type fructans, on host metabolism and key intestinal functions including guthormone release. For the last 20 years, several non-digestible compounds present infood have been shown to modulate the gut microbiota and influence host metabolismin essential organs involved in the control of energy homeostasis. To date, numerousreviews summarize the impact of prebiotics on the liver or the brain. Here we propose todescribe the mechanisms by which prebiotics, through modulation of the gut microbiotaand endocrine functions, modulates the metabolic cross-talk communication betweenthe gut, the adipose tissue and skeletal muscles.Glucose homeostasis disruptions areassociated with changes in the gut microbiotain diabetes and obesityObesity is often associated with a range of metabolicalterations including insulin resistance, type 2 diabetes,dyslipidemia, cardiovascular or non-alcoholic fattyliver diseases. Even if these alterations certainly resultfrom a dysregulation of the balance between energyintake and energy expenditure, it has been now clearlyestablished that some other factors can participate tothe development and progression of cardio-metabolicdiseases. Over the last decade, gut microbial changes(composition and/or function) have been associated withobesity, metabolic disorders, and ‘pre’ diabetes leadingto a ‘dysbiotic state’ (Qin et al. 2012, Allin et al. 2018).This suggests that the gut microbiota can be involved 0.1530/JOE-20-0499 2021 Society for EndocrinologyPublished by Bioscientifica Ltd.Printed in Great BritainKey Wordsff gut microbiotaff fat massff prebioticff skeletal musclesJournal of Endocrinology(2021) 249, R1–R23a cause or consequence) in the insulin resistance process,and therefore in the disruption of endocrine system.Indeed, compared to non-diabetic individuals, thegut microbiota from type 2 diabetic patients (T2D)were characterized by a lower abundance of severalbacteria (Clostridiales spp. SS3/4, Eubacterium rectale,Faecalibacterium prausnitzii, Roseburia intestinalis andRoseburia inulinivorans) able to generate butyrate, oneimportant short chain fatty acid (SCFA) produced uponfermentation of carbohydrates and fibers (Qin et al.2012). The decreased abundance of butyrate-producingbacteria was confirmed in a Chinese cohort and seemedto appear early, in the period of prediabetes (Zhang et al.2013). Indeed, the abundance of some bacteria (such asAkkermansia muciniphila and Faecalibacterium prausnitizii)were higher in individuals with normal glucose tolerance,compared to prediabetic subjects (Zhang et al. 2013).Downloaded from Bioscientifica.com at 05/06/2022 09:55:02PMvia free access
Journal ofEndocrinologyJ Rodriguez andN M DelzenneButyrate has been previously described as a beneficialmetabolite for the intestinal physiology (including gutbarrier function, intestinal inflammation, adherenceof beneficial microbes in colonic epithelial cells, gutpermeability) but it can also be linked with metabolichealth by regulating body weight gain and glucosehomeostasis (Blaak et al. 2020).A higher abundance of opportunistic pathogens(Bacteroides caccae, Clostridium hathewayi, Clostridiumramosum, Clostridium symbiosum, Eggerthella lenta andEscherichia coli) characterizes diabetics from non-diabeticcontrols (Qin et al. 2012). Moreover, the fecal metagenomefrom European women with normal, impaired ordiabetic glucose control revealed positive associations forClostridium clostridioforme with triglycerides and C-peptidelevels, and Lactobacillus gasseri with fasting glucose andhemoglobin A1c (HbA1c), in T2D patients (Karlssonet al. 2013). In addition, 21 metagenomic clusters weredepleted in T2D women, particularly clusters belonging toRoseburia genus, Clostridium species, Eubacterium eligens,several Clostridiales and one Bacteroides intestinalis, thelatter being negatively correlated with waist circumferenceand insulin level. In addition, among a population ofDanish obese individuals, those with a low bacterialrichness seem to be susceptible to have a more markedadiposity, insulin resistance and inflammatory phenotypecompared to the ones with a higher bacterial richness (LeChatelier et al. 2013). Individuals with reduced microbialgene richness were also more susceptible to present dysmetabolism and low-grade inflammation in a cohortof French obese or overweight subjects (Cotillard et al.2013). Interestingly, a diet-induced weight loss improvedthe gut bacterial richness and partially reversed themetabolic alterations. More recently, in the same Frenchcohort, the authors established a link between a lowgut microbiota richness and a high level of ceramides,lipids mediators involved in the development of type2 diabetes (Kayser et al. 2019). They highlighted adecreased abundance of Methanobreviibacter smithii andanti-inflammatory bifidobacteria species associated withhigher ceramides levels. Another recent study highlightedthat Danish adults with prediabetes exhibit an aberrantgut microbiota in which the main differences (comparedto individuals with normal glucose regulation) are a lowerabundance of both Clostridium genus and the mucindegrading bacterium A. muciniphila (Allin et al. 2018).However, the analysis of gut microbiota changes in thecontext of impaired glucose homeostasis is quite difficultsince largely prescribed antidiabetic treatments, such asmetformin, generate confounding effects by i.org/10.1530/JOE-20-0499 2021 Society for EndocrinologyPublished by Bioscientifica Ltd.Printed in Great BritainGut microbiome, fat mass andskeletal muscles249:1R2per se the gut microbiota composition (Forslund et al. 2015,Rodriguez et al. 2018). In this context, a study performedin Swedish subjects naïve for diabetic treatments, showedthat gut microbiota composition was altered in peoplewith impaired glucose tolerance, glucose intolerance(impaired glucose tolerance associated to impaired fastingglucose) and T2D individuals, but not in those withimpaired fasting glucose (Wu et al. 2020). This studyconfirmed a decreased abundance of several butyrateproducers, but also highlighted an alteration of butyrateproduction with glycemic status in both prediabetesand T2D groups. Interestingly, these gut microbiotaalterations were present in prediabetic individuals, butincreased with glucose intolerance and linked with insulinresistance. In addition to the SCFA production alterations,an elegant review recently summarized the modificationof gut microbiota dysfunctions that are occurring in type2 diabetes patients, namely an increased sugar-relatedmembrane transport that promotes cellular glucoseuptake, a higher transport of the branched-chain aminoacids (BCAA) and a lowered metabolism of cofactors andvitamins (Fan & Pedersen 2020). This strongly supportsthe association between the gut microbiota and theendocrine system, especially in the glucose homeostasiscontrol.The gut microbiota as modulator of hostmetabolism disturbancesThe causal role of the gut microbiota in thedevelopment of obesity and insulin resistanceIn 2004, a pioneering study highlighted that thegut microbiota can control the host metabolism byregulating fat storage in murine model (Backhed et al.2004). Indeed, the colonization of germ-free (GF) micewith cecal microbiota from the conventionally raisedmice was sufficient to promote the triglycerides storagein adipocytes and insulin resistance, despite a reductionof energy intake. This supported for the first time thatthe gut microbiota has a causal role in the occurrenceof adiposity and glucose homeostasis. In addition, thesame group reported that, contrary to conventionalizedmice, GF mice are protected against the obesity inducedby a high-fat/high-sugar (HF/HS) diet (Backhed et al.2007). This protection was associated with a higherphosphorylation of AMP-activated protein kinase, and itsdownstream targets involved in fatty acid (FA) oxidation,in both skeletal muscles and liver from GF mice, comparedto conventionalized ones. The suppression of intestinalDownloaded from Bioscientifica.com at 05/06/2022 09:55:02PMvia free access
Journal ofEndocrinologyJ Rodriguez andN M Delzenneexpression angiopoietin-like protein 4 (Angpt14) in GFmice abolished the protection of mice against the dietinduced obesity and was associated with increased seruminsulin levels. Interestingly, the deficiency of Angptl4in GF fed a high-fat/high-sugar diet is associated with adecreased expression of markers involved in FA oxidationin skeletal muscles, independently of AMPK regulation. In2010, another team confirmed the resistance of GF miceto the high-fat/high-sugar diet-induced obesity (Rabotet al. 2010). They showed that this protection was dueto an improvement of insulin sensitivity and a reducedplasma level of proinflammatory cytokine tumor necrosisfactor alpha (TNF-alpha) in GF mice fed with a HF/HS diet,compared to conventional mice. Indeed, the inflammatoryprocess creates a linkage between the gut microbiota andinsulin resistance. In 2007, it was demonstrated in micethat a HF diet generated endotoxemia, defined as anincrease of plasma lipopolysaccharide (LPS), a bacterialcomponent from the Gram-negative bacteria (Caniet al. 2007a). This endotoxemia was associated withchanges in the gut microbiota. Among these changes, alower abundance of Bifidobacterium spp. and E. rectaleClostridium coccoides group were found. Interestingly,mimicking endotoxemia by infusing LPS induced bodyweight gain, adiposity, liver insulin resistance andtriggered the expression of inflammatory markers inadipose tissue, liver and skeletal muscle. In addition,antibiotic treatment in both high-fat–fed and ob/ob micereduced endotoxemia, glucose intolerance, fat massexpansion and inflammation in adipose tissue. Finally,colonization of GF Swiss Webster mice with a microbiotaobtained from conventionally raised mice has beenshown to promote inflammation in the white adiposetissue (WAT) by favoring the recruitment of macrophages,LPS being involved in this process (Caesar et al. 2012). Inaddition to the involvement of gut microbiota, the typeof dietary lipids in the diet also plays a crucial role in thedevelopment of WAT inflammation. Indeed, mice fedlard for 11 weeks exhibit WAT inflammation, increasedToll-like receptor (TLR) activation and reduced insulinsensitivity compared with mice fed fish oil (Caesar et al.2015). Actually, this result was associated with a differentregulation of gut microbiota composition in response todifferent dietary fat sources. For instance, lard inducedan increase of Bilophila, Bacteroides, Turicibacter generawhereas fish-oil favored the growth of bacteria associatedwith beneficial effects on health such as Akkermansia,Bifidobacterium or Lactobacillus genera (Caesar et al. 2015).The causal role of the gut microbiota in insulinsensitivity has also been reported supported by /10.1530/JOE-20-0499 2021 Society for EndocrinologyPublished by Bioscientifica Ltd.Printed in Great BritainGut microbiome, fat mass andskeletal muscles249:1R3material transfer (FMT) interventions in humans(Vrieze et al. 2012). By infusing the intestinal microbiotafrom lean donors to individuals with metabolic syndrome,an improvement of insulin sensitivity and an increasedabundance of butyrate-producing bacteria was observedin recipient patients after 6 weeks. Five years later, thesame group repeated the intervention on other patientsand demonstrated that insulin sensitivity improvementwas accompanied by changes in plasma metabolitesprofiling (including modifications of γ-aminobutyric orlysophosphatidic acid) but no change in fasting plasmaSCFA was reported (Kootte et al. 2017). Interestingly, theauthors demonstrated that the baseline fecal microbiotacomposition has a determinant role in the improvementof peripheral insulin sensitivity since its composition canpredict the success of the allogenic FMT. Indeed, metabolicresponders were characterized by a lower microbialdiversity, a higher abundance of Subdoligranulum variabileand Dorea longicatena and lower abundance of Eubacteriumventriosum and Ruminococcus torques, compared tonon-responders. Finally, recent works highlighted theimportance for identifying and studying the impact of gutbacterial metabolites on health. Indeed, current researchin the field of metabolic diseases focus on the relation ofsome bacterial products derived from carbohydrates orprotein fermentation and the obesity-associated insulinresistance (Canfora et al. 2019).Focus on bacteria prone to improve glycemic controland metabolic disturbancesIn addition to the beneficial effects observed by transferringthe fecal gut microbiota from lean donors into recipientswith metabolic syndrome, it has been demonstrated thatsome specific bacteria can also improve the obesity andassociated disorders, these bacteria being thus proposedas probiotics. Probiotics have been defined as ‘livemicroorganisms that, when administered in adequateamounts, confer a health benefit on the host’ (Hill et al.2014). For instance, the administration of Bifidobacteriumand Lactobacillus strains in HF-fed mice lowered the bodyweight gain, and improved glycemic control (Wang et al.2015, Alard et al. 2016). Lactobacillus acidophilus NS1(LNS1) inhibited the development of insulin resistance inHF mice by restoring the phosphorylation of Akt protein(involved in the insulin pathway) in the liver, adiposetissues and skeletal muscles (Park et al. 2018). Similarly, atreatment with a mix of probiotics containing Lactobacillusand Bifidobacterium strains also improved blood glucosein mice by regulating the phosphorylation of Akt proteinDownloaded from Bioscientifica.com at 05/06/2022 09:55:02PMvia free access
Journal ofEndocrinologyJ Rodriguez andN M Delzenneboth in the liver and skeletal muscles (Bagarolli et al. 2017).The treatment with A. muciniphila in HF-fed mice alsoreduced fasting glycemia and improved glucose tolerance(Everard et al. 2013, Plovier et al. 2017). This bacteriumreduced the macrophage infiltration and improved theFA oxidation in visceral fat depots. Interestingly, theadministration of pasteurized form of A. muciniphilaenhances energy expenditure, oxygen consumption andphysical activity in HF mice (Depommier et al. 2020). A.muciniphila reduces fat mass accumulation and decreasesthe expression of perilipin 2 – a factor associated withlipid droplets – in both brown and white adipose tissues.Finally, in small cohort of obese human volunteers,three months of supplementation with pasteurizedA. muciniphila improved insulin sensitivity, reducedinsulinemia and plasma total cholesterol (Depommieret al. 2019). Other bacteria seem interesting in the contextof insulin resistance such as Eubacterium hallii (now calledAnaerobutyricum hallii). Daily oral gavage with A. halliiduring 4 weeks significantly improved adiposity, insulinsensitivity and increased energy expenditure in db/db mice(Udayappan et al. 2016). Additionally, oral treatment withF. prausnitzii in HF-fed mice improved hepatic fat content,both insulin sensitivity and inflammation in adiposetissues and increased skeletal muscle mass (Munukkaet al. 2017). All these studies support the idea thatspecific bacteria isolated from the human gut microbiotaparticipate to the regulation of host metabolism inperipheral tissues, targeting the liver, the adipose tissueand the muscle.Finally, it is now obvious that the gut microbiotacontributes to metabolic function in healthy individualsand disruption of this ecosystem promoted a diseased stateassociated with some detrimental metabolic outcomes:systemic inflammation, altered gut barrier function,insulin resistance, increased adiposity and plasmacholesterol or triglycerides (Green et al. 2020). To date,there are different ways by which the gut microbiotacan modulate the mechanisms of obesity includingthe processes of energy extraction and absorption, theinduction or prevention of metabolic endotoxemia, andthe production of bacterial metabolites such as SCFAwhich are able to stimulate the release of the satietyinducing hormones peptide YY (PYY) and glucagon-likepeptide-1 (GLP-1) (da Silva et al. 2020). In this context,the modulation of gut microbiota by promoting thegrowth of some specific bacteria by a prebiotic approachcan be an effective strategy to reverse some features ofthe microbial dysbiosis and improve some metabolicalterations. A recent review summarized the doi.org/10.1530/JOE-20-0499 2021 Society for EndocrinologyPublished by Bioscientifica Ltd.Printed in Great BritainGut microbiome, fat mass andskeletal muscles249:1R4work and the available human intervention studies thatevaluated the anti-obesity effect of prebiotics (Cerdo et al.2019). In our review, we describe the influence of prebioticinterventions on the gut microbiota composition andfunction, with a focus on the endocrine system regulationand consequences in the metabolism of the adipose tissuesand skeletal muscles.Prebiotic approach in the modulation of thegut microbiota in obesity: gut endocrinesystem, adipose tissue and muscles ashost targetsOver the past decade, numerous studies have investigatedthe beneficial impact of gut microbiota modulationby prebiotics in the context of obesity and metabolicdisorders. Prebiotics are defined as a ‘substrates that areselectively utilized by host microorganisms conferring ahealth benefit’ (Gibson et al. 2017). Indeed, several nondigestible carbohydrates can be fermented by the gutmicrobiota, including oligosaccharides, arabinoxylans,glucans, resistant dextrin or resistant starch. Table 1summarizes the main studies performed in vivo in rodentssupplemented with prebiotics. The outcomes reportedrelate to the gut microbiota composition (Fig. 1), and ofbiological markers of metabolic alterations.From those data, we can elaborate the molecularmechanisms evoked to explain how prebiotics controlenergy homeostasis in obesity, which are summarized inFig. 2. Due to the high number of reviews focusing onthe impact of prebiotics on the liver steatosis and relatedmetabolic disorders, we chose to present the existingliterature related to the effects on the adipose tissueand the skeletal muscles, two organs playing a key rolein storage vs oxidation of fatty acids. The modulationof the endocrine function by prebiotics is often cited asan important mechanism behind the systemic effects onlipid and glucose homeostasis, as well as on food relatedbehavior.In 2007, our team demonstrated that dietarysupplementation with oligofructose (OFS) – a shortchain inulin-type fructan – in HF-fed mice restored theamount of Bifidobacteria in the cecal content, normalizedthe endotoxemia and reduced fat mass accumulation(Cani et al. 2007b). This was linked to an improvementof glucose homeostasis through a better glucose-inducedinsulin secretion. Interestingly, OFS supplementation inob/ob or high fat fed mice reduced adipose tissue weights,increased muscle mass and regulated both pancreaticDownloaded from Bioscientifica.com at 05/06/2022 09:55:02PMvia free access
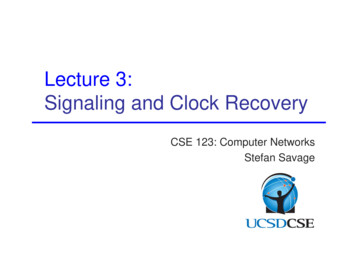
530/JOE-20-0499 2021 Society for EndocrinologyPublished by Bioscientifica Ltd.Printed in Great BritainDewulfet al. 2011HF-fed miceHumanizedgnotobioticdiet-inducedobesity miceITF (oligofructose)for 4 weeksITF (scFOS)for 7 weeksGut microbiota changes4 weeks7 weeks8 weeks5 weeks5 weeksHF-ITF vs HF: BW gain Glucosetolerance ColonproglucagonmRNAGlobal healthHF-ITF vs HF (qPCR):HF-ITF vs HF: Bifidobacterium spp. HOMA-IR Roseburia spp. E. rectale/C. coccoidesgroupob-ITF vs ob-cellulose ob-ITF vs(qPCR):ob-cellulose: Bifidobacterium spp. Intestinal E. rectale/C. coccoides permeabilitygroupImproved Lactobacillus spp.systemic andhepaticinflammationob-ITF vs ob-cellulose ob-ITF vs ob-CT:(16S rRNA): Glucose Bifidobacterium spp.,toleranceTannerella, PlasmaBarnesiella,triglyceridesSubdoligranulum, colonParasutterellaproglucagonmRNA Anaerofilum, BW FOS vs HF:HF-scFOS vs HF: Bifidobacterium spp. BW gain C. coccoides Clostridium leptum14 weeks HF-ITF vs HF (qPCR): Bifidobacterium spp. Eubacteriumrectale/Clostridiumcoccoides group EnterobacteriaceaeDurationHF-scFOS vsHF: plasmaleptin plasmaadiponectinob-ITF vsob-CT: plasmaGLP1HF-ITF vs HF: glucoseinducedinsulinsecretion fastingplasmainsulinob-ITF vsob-cellulose: GLP1, GLP2 GIP Pancreaticpolypeptide AmylinEndocrinesystemSkeletal muscleHF-ITF vs HF: SAT mass SAT adipocytes size Basal SAT lipolysis SAT Grp43 mRNA Cd36, Lpl mRNA SAT inflammation(Tlr4, F4/80 mRNA) SAT adipocytesdifferentiation (aP2,CEBPα mRNA)(Continued) Lean mass Adiposity indexHF-scFOS vs HF: EAT massob-ITF vs ob-CT: muscle mass Lipids contentandtriglyceridesob-ITF vs ob-CT: VAT mass EAT mass SAT mass oxidative stressob-ITF vs ob-cellulose: ob-ITF vs VAT massob-cellulose: EAT mass muscle mass SAT massHF-ITF vs HF: VAT mass EAT mass SAT massAdipose tissueJ Rodriguez andN M DelzenneRespondeket al. 2013For 8 weeksHF-fed miceITF (oligofructose)for 5 weeksITF (oligofructose)for 5 weeksob/ob miceCani et al. 2009ITF (oligofructose)for 14 weeksPrebioticsupplementationob/ob miceHF-fed miceCani et al.2007bEverardet al. 2011ModelReferenceTable 1 Experimental data supporting the impact of prebiotic supplementation on endocrine system, adipose tissues and skeletal muscles in rodent models of obesity.Journal ofEndocrinologyGut microbiome, fat mass andskeletal muscles249:1R5Downloaded from Bioscientifica.com at 05/06/2022 09:55:02PMvia free access
530/JOE-20-0499Inulin: BW gain for onedonor Hepatic lipidsaccumulation fortwo donorsHF/HS-ITF vsHF/HS-G: Glutenimmunogenicpeptide in thececal content Cell renewal inthe jejunum(Intectin)EndocrinesystemHF-Inulin vsHF-cellulose: EAT mass SAT mass SAT adipocytes size Browning process inSAT (Ppargc-1α, Ucp1,Cidea)Adipose tissueInulin: SAT and EAT massfor two donors SAT adipocytes sizefor one donorIn SAT, inulin: Cd36 mRNA for onedonor Pparγ for two donorsIn BAT, inulin: Browning process(Ppargc-1α, Ucp1,Prdm16 mRNA) forone donor3 months With GOSWith GOS:With GOS:With GOS:(pyrosequencing):Glucose tolerance Fasting SAT and VAT Bacteroidetessimilar to theinsulincompared to ActinobacteriaHF-diabetescompared toHF-diabetic mice Parabacteroidesresistant mice,HF-diabetes Phospho-Akt in VAT Oscillibacter, Alistipes, but lowerresistantcompared toOlsenella,compared tomiceHF-diabetic miceMuscispirillumHF-diabetic mice. Leptin and Plasma LPSresistincompared tocompared toHF-diabetic mice. HF-diabetic Triglyceridesmicecompared toHF-diabetic mice.4 weeksHF/HS-ITF vs HF/HS-G: erella,Butyricimonas Clostridium XI,Oscillibacter,Peptococcus, Alistipes,Pseudoflavonifractor18 bacterial generaregulated by inulin(donor-dependenteffects)HF-Inulin vsHF-cellulose: BW gain PlasmacholesterolGlobal healthInulin: Intramuscularlipidsaccumulationandtriglyceridesfor one donor Cd36 andCpt-1β mRNAfor one donor Pparγ for twodonorsHF/HS-ITF vsHF/HS-G: FA transport(Cd36) FA oxidation(Cpt1)Skeletal muscleJ Rodriguez andN M Delzenne 2021 Society for EndocrinologyPublished by Bioscientifica Ltd.Printed in Great BritainGlucooligosaccharides(GOS)for 30 monthsHF-fed miceGut microbiota changes30 weeks HF-Inulin vsHF-cellulose: alisDurationITF (fructo8 weeksoligosaccharides)for 8 weeksSerino et al.2012HF/HS with 5%gluten-fedmiceOlivareset al. 2019Inulinfor 30 weeksHumanITF (Inulin)associated gut for 4 weeksmicrobiotamice (4 groupsof miceinoculatedeach with 1differentdonor)HF-fed miceWeitkunatet al. 2017PrebioticsupplementationRodriguezet al. 2020ModelContinued.ReferenceTable 1Journal ofEndocrinologyGut microbiome, fat mass andskeletal muscles249:1R6Downloaded from Bioscientifica.com at 05/06/2022 09:55:02PMvia free access
530/JOE-20-0499HF-fed miceWang et al.2018a 2021 Society for EndocrinologyPublished by Bioscientifica Ltd.Printed in Great BritainHF-fed miceChitin-glucanfor 4 weeksGut microbiota changes4 weeksHF-MO vs HF: BW gain Liver lipidsaccumulation Plasma LBP Intestinalpermeability BW gain HOMA-IRHF-GAL vs HF: BWgainImprovesinsulin tolerance Plasmacholesterol andtriglycerides GLP-1 mRNA inproximalintestineHF-MOS vs HF: BW gain HOMA-IR Serumcholesterol, HDLand triglyceridesGlobal healthEndocrinesystemHF-I vs HF: Liver lipidsaccumulation Plasma LBP IntestinalpermeabilityHF-CG vs HF (qPCR):HF-CG vs HF:HF-CG vs HF: Bifidobacterium spp., BW gain InsulinemiaRoseburia spp., E. Fasting glycemia,rectale/C. coccoidesHOMA-IRgroup Glucose Bacteroides/Prevotella tolerancespp., Lactobacillus Total and HDLspp.cholesterol HepatictriglyceridesaccumulationHF-MO and HF-I vs HF(16S rRNA): Bifidobacterium andLactobacillus in theileum11 weeks HF-MOS vs HF (NGS): Akkermansia,Bifidobacterium spp.,Sutterella illumNo data16 weeks HF-GAL vs HF (16SrRNA): ella Olsenella, ementationfor 4 weeks withstandard dietbefore 7 weeks ofHFDMilk6 weeksoligosaccharides(MO) andInulin (I)for 6 weeksMannanoligosaccharides(MOS)for 11 weeksβ-galactooligosaccharides(β-GAL)for 16 weeksPrebioticsupplementationHF-CG vs HF: VAT mass EAT mass SAT massHF-MO vs HF: Total Fat mass Mesentericadipocytes size Number of crownlike structures inmesenteric adiposetissueHF-I vs HF: Mesentericadipocytes sizeHF-MOS vs HF: WAT Adipocytes size WAT Leptin andadiponectin mRNA Inflammatorymarkers (Tnf-α, Tlr4,Itgax)HF-GAL vs HF: Perirenal mass EAT massIn BAT: Ucp1Adipose tissue(Continued)Skeletal muscleJ Rodriguez andN M DelzenneNeyrinck et al.2012aHF-fed miceHF/HS-fed miceMistry et al.2020Hamiltonet al. 2017ModelReferenceJournal ofEndocrinologyGut microbiome, fat mass andskeletal muscles249:1R7Downloaded from Bioscientifica.com at 05/06/2022 09:55:02PMvia free access
530/JOE-20-0499 2021 Society for EndocrinologyPublished by Bioscientifica Ltd.Printed in Great BritainHF/HS-fed miceHF-fed miceNeyrinck et al.2012b8 weeks8 weeks4 weeksGlobal healthHF-AXOS vs HF (qPCR): HF-AXOS vs HF: Bifidobacterium spp. BW gain Lactobacillus spp. Plasma Il6 andLPS Claudin 3 in thecolon (gutbarrier)HF/HS-AXOS vs HF/HS(16S rRNA): Bifidobacterium spp.,Butyricicoccus Turicibacter,Clostridium sensustrictoHF-AX vs HF: BW gainImproves glucosetolerance Serumtriglycerides,NEFA,cholesterol, LDL,VLDL Serum LPS Hepatic lipidsaccumulationandinflammationHF-AX vs HF (qPCR):HF-AX vs HF: Bifidobacterium spp., BW gainRoseburia spp., InsulinBacteroides/Prevotella resistance indexspp. Total, LDL andHDL cholesterolGut microbiota changes10 weeks HF-AX vs HF(metagenomic): BlautiaHF-AX vs HF (qPCR): Lactobacillus spp.and Roseburia spp.DurationHF-AXOS vsHF: PYY, GLP1HF-AX vs HF: AdiponectinHF-AX vs HF: OS vs HF: EAT massHF-AX vs HF: VAT mass EAT mass SAT massIn SAT: Inflammatorymarkers (F4/80, Il6) Lipogenesis (Fasn) Fatty acid oxidation(Pparγ, Aco, Cpt-1) Adipocytesdifferentiation (aP2) Fatty acid uptake(Cd36, Lpl) Lipolysis (MGL,Gpr43)HF-AXOS vs HF: EAT mass SAT massIn VAT: Inflammatorymarkers (F4/80)In VAT: Inflammatorymarkers (F4/80, Il6,Mcp1, Il6, NFkB) Lipogenesis (Fasn) Fatty acid oxidation(Pparγ) Adipocytesdifferentiation(C/EBPα)HF-AX vs HF: VAT massAdipose tissueSkeletal muscleGut microbiome, fat mass andskeletal musclesArabinoxylanoligosaccharidesAXOSfor 8 weeksArabinoxylanoligosaccharidesAXOSfor 8 weeksArabinoxylans AXfor 4 weeksArabinoxylans AXfor 10 weeksPrebioticsupplementationJ Rodriguez andN M DelzenneSuriano et al.2017HF-fed miceHF-fed miceSarma et al.2018Neyrincket al. 2011ModelContinued.ReferenceTable 1Journal ofEndocrinology249:1R8Downloaded from Bioscientifica.com at 05/06/2022 09:55:02PMvia free access
530/JOE-20-0499ArabinoxylanoligosaccharidesAXOSfor 8 weeksPrebioticsupplementationHF/HS-AXOS vs HF/HS-G (16S rRNA): erella,Clostridium IV Clostridium XI,Oscillibacter,Peptococcus, Alistipes,OdoribacterGut microbiota changes 2021 Society for EndocrinologyPublished by Bioscientifica Ltd.Printed in Great BritainDFs, barley8 weeksβ-glucan, applepectin, inulin,inulin acetateester (A), inulinpropionate ester(P), inulinbutyrateester (B) or acombination ofinulin propionateester and inulinbutyrate (PB)for 8 weeksFor all vs HF (16SrRNA): OTUs belonging toParabacteroides,Parasutterella OTUs belonging toAlistipes,Mucispi
factor alpha (TNF-alpha) in GF mice fed with a HF/HS diet, compared to conventional mice. Indeed, the inflammatory process creates a linkage between the gut microbiota and insulin resistance. In 2007, it was demonstrated in mice that a HF diet generated endotoxemia, defined as an