Transcription
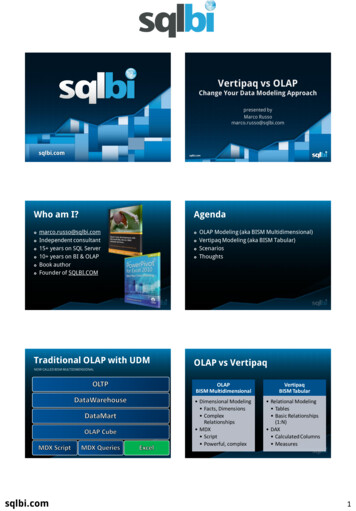
ABC’s or CAB’s: What’sNew in the ResuscitationGuidelines . . . And WhatWas Left OutJill Ley, MS, RN, CNS, FAANClinical Nurse Specialist SurgicalServices, CPMCClinical Professor, UCSF
Learning Outcomes Review key recommendations from TheAmerican Heart Association’s 2015 ECCupdateDiscuss emergency management strategiesthat promote optimal outcomes after inhospital cardiac arrest
Cardiac Arrest Mortality 326,200 out of hospital (OHCA) arrests/yearooSurvival to discharge in 10.6%Good neurologic recovery in 8.3% 209,000 in hospital (IHCA) arrests/yearoSurvival to discharge in 24% 2500-5000 post-cardiac surgery arrests/yearooHigh potential for reversible causes and recoveryWide variation in survival; 40-80%AHA 2015 Heart & Stroke Statistics
Important AHA 2015 Updates Focus on compression fractionoo Capnography recommendationsMedication updatesoooo Rate 100-120 per minuteCompression depth 5-6 cmVasopressin removedLidocaine not routinely recommendedEpinephrine for shockable vs non-shockable rhythmsNaloxone added for suspected opiate overdoseDid NOT address cardiac surgery resuscitationAmerican Heart Association. H I G H L I G H T S of the 2015 American Heart Association GuidelinesUpdate for CPR and ECC. www.heart.org/cpr accessed April 22, 2016
Compressions &High Quality CPR CPR quality affected by both rate and interruptionsCompression fraction portion of total CPR timewhen compressions are performed; goal 60%Optimize by:oooIncreasing rate of compressions ( to 120)Reducing interruptions (frequency and duration)Upper limits for both added in 2015American Heart Association. H I G H L I G H T S of the 2015 American Heart Association GuidelinesUpdate for CPR and ECC. www.heart.org/cpr accessed April 22, 2016
Compressions &High Quality CPRSequence of Interventions Remains C-A-BAmerican Heart Association. H I G H L I G H T S of the 2015 American Heart Association GuidelinesUpdate for CPR and ECC. www.heart.org/cpr accessed April 22, 2016
Self-Assessment Question #1During CPR you note the end-tidal CO2abruptly changed from 15 to 35 mmHg, whichmost likely indicates:1.2.3.4.The person performing CPR is tiredThe patient has expiredEpinephrine should be administeredReturn of spontaneous circulation hasoccurred
Self-Assessment Question #1During CPR you note the end-tidal CO2abruptly changed from 15 to 35 mmHg, whichmost likely indicates:1.2.3.4.The person performing CPR is tiredThe patient has expiredEpinephrine should be administeredReturn of spontaneous circulation hasoccurred
Capnography Provides valuable information aboutpatient response during arrestStrategies should offer continuous monitoring withoutinterrupting compressionsETCO2 remains a Class 1 recommendation to confirmintubation; use for prognostication with other factors
Capnography& CPR Quality Eliminate pulse checks!o Palpation for a pulse is an insensitive indicator of organperfusion with very poor inter-rater reliabilityETCO2 to assess perfusion & response to therapy:oooAssess CPR adequacy; ETCO2 goal 12-15 mmHgETCO2 10 mmHg may be poor quality CPRETCO2 spike to 35-40 mmHg confirms ROSC40200
Electrical Therapy for VF Early defibrillation is critical to survivaloooGuidelines recommend defibrillation within 2 minutesDefibrillation time exceeds 2 min in 30% of US inpatientsSurvival rates are 17% lower when defibrillation timeexceeds 2 min (22.2% vs 39.3%).Chan PS, et al. NEJM 2008;358(1):9-17
Reduce Time to Defibrillation! Defibrillator readily available and standardizedOptimize use of handsfree defibrillator pads Non-code team members can defibrillate
2016 Studies Favor Stacked Shocks Multicenter review: adults w/ IHCA from VF (n 2733) Rapid sequence shocks superior to deferred 2nd shocko ROSC in 62.5% vs 57.4% (Risk Ratio 0.92)o Survival to discharge in 30.8% vs 24.7% (RR 0.80)Bradley SM, Liu W, Chan PS, et al. BMJ 2016; 353:i1653. doi:10:1136/bmj.i1653 Single center review of 3 historical resus protocolso3 SS vs single shock & 2 min CPR vs 3 SS(120j-150j-200j) Worst survival with single shock Highest survival after resuming 3 SS“Our data suggest that in cases of monitoredVF/VT arrest, expeditious defibrillation withuse of stacked shocks is associated with ahigher rate of ROSC and survival to hospitaldischarge.”Davis D, et al. J Hosp Med 2016;11(4):264-268
Recommendations Regarding3 Shock Protocol For refractory VF/pVT in witnessed IHCA, recentdata support use of a 3-shock strategy STS recommends 3 sequential shocks after cardiacsurgery Since 2010 European guidelines recommend 3sequential attempts at defibrillation for witnessedVF/pVT arrest ‘where immediate defibrillation isavailable’ This is currently not recommended in the AHAguidelineSoar J, et al. ERC Guidelines for Resuscitation. Cardiac arrest in special circumstances.Resuscitation 2010; 81:1400-1433.
Medication UpdateWhat’s in, what’s out . . .KISS . . . simplify
Self-Assessment Question #2Which of the following medications does theAHA recommend for a shockable rhythm:1.2.3.4.Epinephrine and AmiodaroneEpinephrine and LidocaineAmiodarone and LidocaineNone of the above
Self-Assessment Question #2Which of the following medications does theAHA recommend for a shockable rhythm:1.2.3.4.Epinephrine and AmiodaroneEpinephrine and LidocaineAmiodarone and LidocaineNone of the above
Drugs forCardiac ArrestEpinephrine notrecommended untilafter 2nd failed shock
Lidocaine Gone
Why? The ALPS The Amiodarone, Lidocaine, or Placebo Study Multicenter RCT; 3026 pts randomly assigned to 1of 3 treatment groups by EMS (out of hospital) Enrolled after at least one failed shock for VF/pVT Results: no significant difference in survival orneurologic recovery between the 3 groupsKudenchuk PJ, Brown SP, Daya M, et al. NEJM.org, April 4, 2016 DOI: 10.1056/NEJMoa1514204.
Important Differences if WitnessedKudenchuk PJ, Brown SP, Daya M, et al. NEJM.org, April 4, 2016 DOI: 10.1056/NEJMoa1514204.
Bye Bye VasopressinAmerican Heart Association. H I G H L I G H T S of the 2015 AmericanHeart Association Guidelines Update for CPR and ECC.www.heart.org/cpr accessed April 22, 2016
The Rationale Important note . Recommendation based on two new studiesshowing lack of clear benefit, not harm No benefit demonstrated for OHCA with VF/pVT Single study showed possible role for vasopressinin IHCA “bundle” combined with epi and steroids?Circulation 2015;132[suppl 2]:S444–S464. DOI: 10.1161/CIR.0000000000000261
Self-Assessment Question #3Which of the following statements aboutEpinephrine is TRUE for a VF arrest:1.2.3.4.Epinephrine is advocated AFTER the 2nd failedshock attempt and not beforeEpinephrine significantly improves neurologicrecovery after arrestEpinephrine is equally effective in shockable vsnon-shockable rhythmsNone of the above
Self-Assessment Question #3Which of the following statements aboutEpinephrine is TRUE for a VF arrest:1.2.3.4.Epinephrine is advocated AFTER the 2nd failedshock attempt and not beforeEpinephrine significantly improves neurologicrecovery after arrestEpinephrine is equally effective in shockable vsnon-shockable rhythmsNone of the above
Epinephrine forShockable Rhythms Multicenter RCT evaluating outcomes when epigiven 2 minutes of first defibrillation failure 2978 patients matched using propensity scores Epinephrine associated with worse outcomesNo BenefitAndersen LW, Kurth T, Chase M, et al. BMJ 2016;353:i1577 doi:10.1136/bmj.i1577
Epinephrine forNon-Shockable Rhythms Improved survival in 3 OHCA trials* (2 large RCT)when epi given within 9-10 minutes of CPR Improved neurologically intact survival in 1 IHCAtrial† (n 25,095) withearly initiationof epinephrineBenefit Seen†Donnino MW, et al BMJ. 2014;348:g3028* Goto Y, et al. Crit Care. 2013;17:R188. doi: 10:1186/cc12872.* Nakahara S, et al. Acad Emerg Med. 2012;19:782-792.* Koscik C, et al. Resuscitation. 2013;84:915-920.
Summary of Epinephrine Data Controversy persists surrounding the optimal use ofepinephrine for cardiac arrest Improved neurologically intact survival has notbeen demonstrated for VF/pVT but was recentlyreported for non-shockable rhythms For shockable rhythmso Use no earlier than 2nd failed shock in standard dose For non-shockable rhythmso Consider early administration
The Opioid Epidemic 21.5 million Americans age 12 havea substance abuse disorder – 1.9million from prescription pain relievers. Drug overdose is now the leadingcause of accidental death in the US. 47,055 fatal OD in 2014: 18,893 frompain meds vs 10,574 from heroin Almost half a million adolescents usepain relievers and 168,000 wereaddicted to pain relievers in 2014. 48,000 women died of prescriptiondrug overdose between 1999-2010.American Society of Addiction Medicine. 2016 Opiod Addiction Facts & opiod-addition-disease-facts-figures.pdf
First Responders Impact on in-hospital arresto Algorithmso Medication availability
Resuscitation AfterCardiac SurgeryA New STS National Standard
We Know That . . .Standard CPR is ineffective in: CARDIAC TAMPONADE PROFOUND HYPOVOLEMIA / BLEEDINGoTENSION PNEUMOTHORAXWithout effective CPR - IRREVERSIBLE BRAIN DAMAGEoccurs within 5 minutesPerforming a RAPID ( 5 min)EMERGENCY RESTERNOTOMYis essential to survival
Self-Assessment Question #4The STS protocol for resuscitation after cardiacsurgery now endorses which of the followingpractices:1.2.3.4.Perform CPR for only 1 minute prior todefibrillationDefibrillate first, prior to starting CPR, ifavailable within 1 minute of witnessed arrestAdminister high dose epinephrine (10 mg) forcardiac arrest with a shockable rhythmAdminister atropine for asystole/profoundbradycardia
Self-Assessment Question #4The STS protocol for resuscitation after cardiacsurgery now endorses which of the followingpractices:1.2.3.4.Perform CPR for only 1 minute prior todefibrillationDefibrillate first, prior to starting CPR, ifavailable within 1 minute of witnessed arrestAdminister high dose epinephrine (10 mg) forcardiac arrest with a shockable rhythmAdminister atropine for asystole/profoundbradycardia
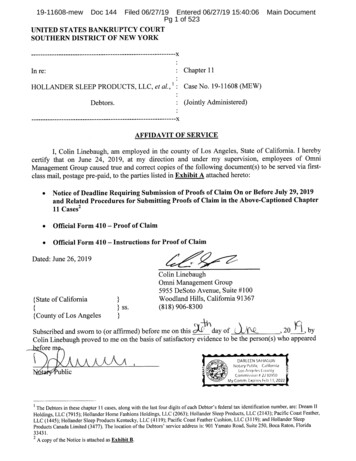
The STS/EACTS Resuscitation Protocol 2003: Two UK surgeons initiate project: J Dunning, A Levine2004: First UK course in Manchester, England2009: EACTS Guideline for Resuscitation After Cardiac SurgeryDunning J, Strang T, Levine A, et al. Eur J Cardiothorac Surg 2009;36:3-28 2009: First US course in San Francisco, California2010: International Liaison Committee on Resuscitation &European Resuscitation Council guidelinesNolan JP, et al. Resuscitation 2010;81:1219-1276 2015: STS Resuscitation Task Force initiated2017: Publication of STS Expert Consensus StatementDunning J, Levine A, Ley J, et al. Ann Thorac Surg, Feb 2017
STS/EACTS Protocol vs ACLSSTS /EACTS ProtocolACLSFor VF/pVTDefibrillation takes priority; maydefer CPR for up to 1 minuteCPR should be performedimmediately on all patients3 successive shocks before CPRCPR 1 shock CPRFor AsystoleDual chamber pacing, maxoutputCPR and EPIFor VF/pVT, Asystole, Pulseless Electrical ActivityNo epi unless by senior clinician;If used pre-arrest reduce doseEpinephrine 1000 mcg every 3-5minutesUse 6 key roles in arrest;2 sterile providers gown & gloveSimilar roles and responsibilitiesRapid resternotomy ( 5 min) if noresponse to pacing/defibrillationN/A
March 2017– Ann Thorac Surg
STS Protocol Implementation Designation of specific roles for team membersClearly defined expectations by roleProtocol implemented without waiting for ordersTEAM-work!
The STS/EACTSResuscitationProtocolFor PostoperativeCardiac SurgicalArrest
Role Functions inPostop Arrest# 1: Defib or pace, then start CPR# 2: Airway, O2 to 100%, no PEEP# 3: External defibrillator - switch tointernal defib; pacemaker# 4: Run code, in charge of arrest# 5: Amiodarone, stop other drips# 6: Run unit, delegate resources#7 and #8: Prepare for re-entryDunning J, Alessandro F, Phillippe HR, et al. Eur J CTS 2009;36:3-28
“Mini” Resternotomy Set1.2.3.4.5.6.ScalpelWire cutterWire pullerRetractorSuction tubing/yankauerOptional: scissor, forcepsClass IRecommendation
Protocol for Reopening1.“Sterile OR personnel” 2.3.4.Apply large sterile drape over entire bedReceive “mini” instrument set onto sterile fieldStand back when surgeon ready with scalpelScalpel used along prior incision down to wired sternumRemove wires; cut/pull (side w/knot)Insert closed chest retractor carefully Crank retractor until sternum open widelyAssess for bleeding; ready with suctionInternal massage 1 minInternal defibrillator paddles 20j x 3
Impact on Failure To RescueBenchmark60%Ley SJ, Gaudiani VG, Egrie GE, Shaw RE, Brewster J. Poster presentedat STS 51st Annual Meeting, January 2015, San Diego, CA
Potential Cath Lab Emergencies Procedure related Rhythm related Vessel dissectionPneumothoraxTamponadeBrady arrhythmias/tachyarrhythmiasHypotension/ST changes Preload/volumePump – problemAfterloadTamponadeCo –morbiditiese.g.e.g.e.g.e.g.e.g.femoral blood lossIschemia, dissection, stunningdrug reaction or GTNcardiac and pneumothoraxCVA, DMDrug Related Sedation- airway compromise, respiratory depressionAnaphylaxisDrug errorsHypotension (i.e. secondary to NTG)
CPR after TAVR
Cardiac Catheterization Lab: Responseto EmergenciesCath Lab Team – What is Your Immediate Response toThese Complications?Does the room/equipment configuration lend itself toemergency resuscitation?Does your team train for / rehearse these emergencies?
Personnel Positioning21. Massage/Defib412. Airway3. Team Leader64. Drugs35. Resource Manager6. Scrub Nurse577. Runners
Personnel Positioning
Summary Shockable rhythmso Early defibrillation saves lives - shock without delayo Consider stacked shocks for witnessed IHCAo Amiodarone is the only recommended antiarrhythmico Epinephrine has no survival benefit Nonshockable rhythmso Epinephrine may be of benefit, if given early New protocol recommended post-cardiac surgery Simplify arrest management to what works:o High quality CPR saves liveso Capnography is our best monitor for ETT placementand ongoing response
“Universal” ACLS 014/11/Updated-2015-ACLS-Algorithm.jpg
ABC’s or CAB’s: What’s New in the Resuscitation Guidelines . . . And What Was Left Out Jill