Transcription
P1: PBULWBK312-FMLWBK312-HudaJune 19, 2009Review ofRadiologicPhysicsThird EditionWalter Huda, Ph.D.Professor of RadiologyMedical University of South Carolina (MUSC)Charleston, SCi10:22
P1: PBULWBK312-FMLWBK312-HudaJune 19, 2009Acquisitions Editor: Brian BrownManaging Editor: Ryan ShawMarketing Manager: Angela PanettaProduction Editor: Beth MartzCreative Director: Doug SmockCompositor: Aptara, Inc.Third EditionC 2010, 2003 Lippincott Williams & Wilkins, a Wolters Kluwer business.Copyright 351 West Camden StreetBaltimore, MD 21201530 Walnut StreetPhiladelphia, PA 19106Printed in ChinaAll rights reserved. This book is protected by copyright. No part of this book may be reproduced ortransmitted in any form or by any means, including as photocopies or scanned-in or other electronic copies,or utilized by any information storage and retrieval system without written permission from the copyrightowner, except for brief quotations embodied in critical articles and reviews. Materials appearing in this bookprepared by individuals as part of their official duties as U.S. government employees are not covered by theabove-mentioned copyright. To request permission, please contact Lippincott Williams & Wilkins at530 Walnut Street, Philadelphia, PA 19106, via email at permissions@lww.com, or via website at lww.com(products and services).9 8 7 6 5 4 3 2 1Library of Congress Cataloging-in-Publication DataHuda, Walter.Review of radiologic physics / Walter Huda.—3rd ed.p. ; cm.Includes bibliographical references and index.ISBN 978-0-7817-8569-31. Radiology, Medical—Outlines, syllabi, etc. 2. Medical physics—Outlines, syllabi, etc.I. Title.[DNLM: 1. Health Physics—Examination Questions. WN 18.2 H883r 2010]R896.5.H83 2010616.07’54076—dc222009008871DISCLAIMERCare has been taken to confirm the accuracy of the information present and to describe generally acceptedpractices. However, the authors, editors, and publisher are not responsible for errors or omissions or for anyconsequences from application of the information in this book and make no warranty, expressed or implied,with respect to the currency, completeness, or accuracy of the contents of the publication. Application of thisinformation in a particular situation remains the professional responsibility of the practitioner; the clinicaltreatments described and recommended may not be considered absolute and universal recommendations.The authors, editors, and publisher have exerted every effort to ensure that drug selection and dosage setforth in this text are in accordance with the current recommendations and practice at the time of publication.However, in view of ongoing research, changes in government regulations, and the constant flow ofinformation relating to drug therapy and drug reactions, the reader is urged to check the package insert foreach drug for any change in indications and dosage and for added warnings and precautions. This isparticularly important when the recommended agent is a new or infrequently employed drug.Some drugs and medical devices presented in this publication have Food and Drug Administration (FDA)clearance for limited use in restricted research settings. It is the responsibility of the health care provider toascertain the FDA status of each drug or device planned for use in their clinical practice.To purchase additional copies of this book, call our customer service department at (800) 638-3030 or faxorders to (301) 223-2320. International customers should call (301) 223-2300.Visit Lippincott Williams & Wilkins on the Internet: http://www.lww.com. Lippincott Williams & Wilkinscustomer service representatives are available from 8:30 am to 6:00 pm, EST.ii10:22
P1: PBULWBK312-FMLWBK312-HudaJune 19, 2009To my parents,Stefan and Paraskevia Huda,for their resolute support and encouragementiii10:22
P1: PBULWBK312-FMLWBK312-HudaJune 19, 2009Ordinary language is totally unsuited for expressingwhat physics really asserts, since the words of everyday lifeare not sufficient y abstract. Only mathematics and mathematicallogic can say as little as the physicist means to say.—BERTRAND RUSSELLiv10:22
P1: PBULWBK312-FMLWBK312-HudaJune 19, 2009ContentsPreface ixAcknowledgementsIntroductionI.II.III.IV.V.13What is Radiologic Physics?Why Study Radiologic Physics?Review Book StructureRadiology Residents and the ABR ExamRadiology Technologists and the ARRT ExamX-Ray ProductionI.II.III.IV.V.VI.2xiBasic PhysicsElectromagnetic RadiationX-ray GeneratorsMaking X-raysX-ray TubesX-ray Tube PerformanceReview TestAnswers and Explanationsxiiixiiixiiixivxivxv113469111416X-Ray terX-rays and MatterAttenuation of RadiationX-ray Filtration EffectsScatter RemovalMeasuring RadiationReview TestAnswers and ExplanationsProjection Radiography ng ScreensDigital BasicsDigital DetectorsDigital RadiographyDigital Image DataReview TestAnswers and Explanationsv10:22
P1: PBULWBK312-FMLWBK312-Hudavi456ContentsProjection Radiography II51I.II.III.IV.V.VI.515356586162666889Mammography Imaging ChainClinical MammographyMQSAImage IntensifiersTelevisionII/TV ImagingReview TestAnswers and ExplanationsComputed agesScanner OperationDosimetryMiscellaneousReview TestAnswers and ExplanationsImage QualityI.II.III.IV.V.7June 19, 2009ContrastResolutionImaging System ResolutionNoiseMeasuring PerformanceReview TestAnswers and Explanations878789929497100102Radiobiology/Patient 120BasicsHigh-Dose EffectsCarcinogenesisHereditary and Teratogenic EffectsPatient DosimetryEffective DoseReview TestAnswers and ExplanationsRadiation 6138Measuring RadiationDose LimitsProtecting WorkersPatient DosesProtecting PatientsPopulation DosesReview TestAnswers and ExplanationsNuclear Medicine139I.RadionuclidesII. RadiopharmaceuticalsIII. Planar Imaging13914314610:22
P1: PBULWBK312-FMLWBK312-HudaJune 19, 2009ContentsIV.V.VI.VII.viiTomographyQuality ControlImage QualityRadiation DosesReview TestAnswers and Explanations15015315415515916110 UltrasoundI.PropertiesII. InteractionsIII. TransducersIV. ImagingV. DopplerVI. Imaging PerformanceReview TestAnswers and Explanations16311 Magnetic ResonanceI.PhysicsII. RelaxationIII. InstrumentationIV. ImagingV. Imaging PerformanceVI. Contrast AgentsVII. Advanced TechniquesReview TestAnswers and Explanations181Examination GuidePractice Examination A: QuestionsPractice Examination A: Answers and ExplanationsPractice Examination B: QuestionsPractice Examination B: Answers and 118318518919219419519719910:22
P1: PBULWBK312-FMLWBK312-HudaJune 19, 2009viii10:22
P1: PBULWBK312-FMLWBK312-HudaJune 19, 2009PrefaceSix years have now passed since the second edition of Review of Radiologic Physicsappeared. The focus of this book remains imaging using x-rays (i.e., projection radiography, fluoroscopy, and CT), as well as nuclear medicine, ultrasound, and magneticresonance (MR). Only essential information is included to help radiology residentsand radiologic technologists understand how images are created, as well as the corresponding risks of the radiation used to make these images. Basic physics topicsrelating to the production and interaction of x-rays have been kept to a minimum,while more important topics of radiation biology, radiation protection, and nuclearmedicine have been expanded.In this third edition, major changes have been made with respect to the organization as well as content of the text, tables, figures, and questions. The first two chaptersdeal with x-ray production and x-ray interactions. Three chapters address how x-rayscan be used to generate projection and tomographic images. Image quality (i.e., contrast, resolution, and noise) is now comprehensively covered in one chapter, whichdescribes both the basic concepts and the specific values of these parameters for allimaging modalities that use x-rays. Radiation biology and radiation protection areboth very important topics that now merit their own chapters. Material on nuclearmedicine, ultrasound, and MR has been updated, but these chapters continue to focus on basic physics. Accordingly, only minimal information is provided on the moreadvanced applications of nuclear medicine, ultrasound, and MR that are currentlyused in clinical practice.One important theme in the revised books is to focus on the material that nonphysicists need to understand to permit them to perform routine clinical duties.Selection of material has been guided by whether the material is necessary to really understand three issues: (a) the essentials (but not details) as to how any imageis created; (b) the factors that impact on the image quality, and how this featurecan be controlled and optimized; (c) the factors that impact on (any) imaging risksand other imaging costs, and how these characteristics can be minimized withoutadversely affecting diagnostic information. Another important goal has been to simplify the material by minimizing superfluous details as well as streamlining all tablesand simplifying the figures to convey only the most important features. The authorfirmly believes that the provision of an approximate conceptual mental picture ofimage formation is much more valuable than detailed descriptions that may be technically accurate but are of minimal didactic value.Most of the questions in the book have now been revised and, hopefully, improved. Each question relates to a specific piece of information that the author believesto be important for residents and technologists to know. In writing these questions,every effort has been made to ensure that they are clear and unambiguous; as such,the author would expect that any physics teacher would grasp why a particular question was being asked, as well as being able to immediately identify the correct answer.The two practice tests contain 10 questions from each chapter, and are designed toix10:22
P1: PBULWBK312-FMLWBK312-HudaxJune 19, 2009Prefacepermit residents to assess how well they have assimilated the material presented inthis review. As with previous editions, readers need to understand that this reviewbook does not explain any topic in full detail. Accordingly, the material covered inthis book should be read in conjunction with a more comprehensive textbook on thetopic of medical imaging.10:22
P1: PBULWBK312-FMLWBK312-HudaJune 19, 2009AcknowledgementsThe author gratefully acknowledges the assistance ofS Balter, PhDM Bilgen, PhDSC Bushong, PhDC Daniels, PhDRG Dixon, MDS Elojeimy, MD/PhDGD Frey, PhDC Gadsen, RTEL Gingold, PhDNA Gkantsios, PhDK Green-Donnelly, MBA, RTW He, MEngKR Johnson, PhDEM Leidholdt Jr, PhDE Mah, MSM Mahesh, PhDPS Morgan, PhDKM Ogden, PhDRJ Pizzutiello, PhDTL Pope Jr, MDDW Rickey, PhDDWO Rogers, PhDML Roskopf, RTR ShawP Sprawls, PhDNM Szeverenyi, PhDL TheronLK Wagner, PhDAB Wolbarst, PhDCE Willis, PhDMV Yester, PhDxi10:22
P1: PBULWBK312-FMLWBK312-HudaJune 19, 2009xii10:22
P1: PBULWBK312-FMLWBK312-HudaJune 19, 2009IntroductionI. WHAT IS RADIOLOGIC PHYSICS?Radiology is arguably the most technology-dependent specialty in medicine, andwhich has seen significant changes over the past decade. Computer integration withconstant technical innovations have changed the workplace and influenced the roleradiology plays in the diagnosis and treatment of disease. Radiologic physics is not anesoteric subject of abstract equations and memorized definitions, but rather the totalprocess of creating and viewing a diagnostic image. A range of physical principlesinfluence the process of image formation. Radiologists and technologists need tounderstand the technology and the physical principles that constitute the advantages,govern the limitations, and determine the risks of the equipment they use.Radiologic physics covers the important medical imaging modalities of radiographic and fluoroscopic x-ray imaging, computed tomography, magnetic resonance,nuclear medicine, and ultrasound. Radiologic physics provides an understandingof the factors that improve or degrade image quality. Selection of the most appropriate way of generating a medical image is the responsibility of the radiologicimaging team, consisting of the radiologist, technologist, medical physicist, andequipment manufacturer. Optimizing medical imaging performance requires a solidunderstanding of how these images are generated, as well as the most importantdeterminants of image quality.All imaging modalities have a cost associated with their use. For modalities thatuse ionizing radiations, one of the costs is the radiation dose to the patient andstaff working with these systems. Accordingly, radiation protection principles areimportant. Radiologists and technologists should understand the magnitude of theradiation dose to the patient and personnel exposed, and ensure that radiation levelsare kept as low as reasonably achievable (ALARA principle) as well as within anyrelevant regulatory limits. MR and ultrasound do not have any specific risks, and thecost is generally the time required to perform the study.II. WHY STUDY RADIOLOGIC PHYSICS?Radiologists and technologists need to acquire an understanding of the underlyingimaging science for each diagnostic modality and be able to pass their respectiveradiologic physics exams. However, neither will actually practice physics and thereis no need to learn how to generate modulation transfer functions in radiographicimaging, write programs to perform filtered back projection algorithms in CT, ordesign RF pulses in MRI.It is important for well-rounded radiologists and technologists to have a basicunderstanding of the following: (i) image quality parameters, such as mottle, spatialxiii10:22
P1: PBULWBK312-FMLWBK312-HudaxivJune 19, 2009Introductionresolution, and contrast; (ii) how image quality is affected by radiographic techniques;(iii) how to evaluate commercial imaging equipment in terms of its ability to performthe required patient examinations; (iv) the radiation dose and risks associated withradiographic exposure; and (v) how to communicate with medical physicists andservice personnel regarding imaging problems.The focus of the text and allied questions is the essential physics underlying thecreation of clinical images. Special emphasis has been given to the factors impacting on image quality, notably image contrast, spatial resolution, and mottle. Radiologists and technologists understand the achievable performance of any imagingequipment and how this equipment should best be used to solve patient imagingproblems.III. REVIEW BOOK STRUCTUREThis review book is designed to help prepare residents and technologists for theradiologic physics portion of their board and registry exams. It provides a sourcefor comprehensive self-study in the area of diagnostic radiologic physics. The textassumes a background of instruction in radiologic physics and is not intended toreplace the standard radiologic physics texts. This book is designed, rather, to providea concise yet complete source of review to refresh and reinforce the concepts ofradiologic physics expected of residents and technologists.The text is divided into 11 chapters, each with approximately six subsections,covering everything from basic physics to image quality. Each chapter begins with asummary of the key information in point form pertaining to the area under review.This is followed by 30 questions designed to provide a self-test of the reader’s knowledge and comprehension in each area. The philosophy adopted by the author is thatmaterial comprehension, rather than rote memorization, will guarantee success inthe exam. The review book also contains two practice examinations with questionsthat range over the topics covered in this book. At the end of the book is a glossaryof key terms commonly used in radiologic physics.Radiation quantities are generally provided using SI units. Use of roentgen tospecify radiation exposure is problematic, and use of the correct conversion factor(i.e., 1 R 2.58 10 4 C/kg) would be inappropriate given current practice in medicalimaging literature. In diagnostic radiology, an exposure of 1 R can be taken to be equalto an air kerma of 8.76 mGy. In the text that follows, exposures have been replacedby air kerma, with an air kerma of 10 mGy taken to be approximately equivalent to anexposure of 1 R. In nuclear medicine, non-SI units predominate in clinical practicein the United States, whereas SI units are prevalent outside of the United States andin the scientific literature. In this book use is made of SI units (i.e., MBq), with thenon-SI equivalent (i.e., mCi) provided in parenthesis. Magnetic fields are generallyexpressed in teslas, with recognition given to the fact that MR personnel are muchmore likely to refer to the 5-gauss line than a 0.5-mT line.IV. RADIOLOGY RESIDENTS AND THE ABR EXAMThe physics portion of the American Board of Radiology (ABR) examination is administered in the fall of each year and taken on a computer. Board-eligible residentsmay register 1 year in advance to take the examination in September of their second,third or fourth year of training. The 4-hour examination contains about 130 multiplechoice questions, similar to the format used in this book. Calculators are not allowed,but one is available on the PC. Most residents comfortably finish the exam in theallowed time, with no need to perform any calculations beyond trivial additions,multiplications, or divisions.10:22
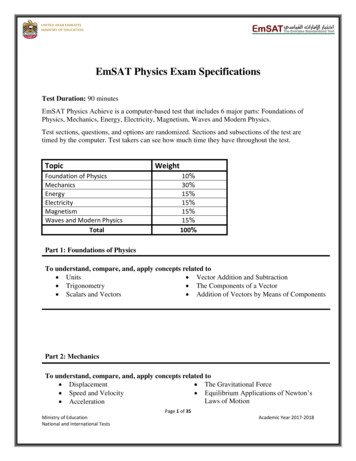
P1: PBULWBK312-FMLWBK312-HudaJune 19, 2009IntroductionxvAbout 60% of the questions cover x-ray-based imaging, image quality, ultrasound, and MR. Approximately 20% of the questions relate to nuclear medicine, and theremaining 20% to issues relating to radiation biology and protection. Results in the formof quartiles are provided to candidates who have taken the physics examination andpertain to each of these three syllabus categories. Further information regarding theAmerican Board of Radiology and the written physics examination can be obtainedat the ABR web site (theabr.org).V. RADIOLOGY TECHNOLOGISTS AND THE ARRT EXAMThe American Registry of Radiologic Technologists (ARRT) administers credentialing examinations and provides continuing registration for radiologic technologistswithin the United States. A multiple-choice test format, consisting of approximately200 questions, is used to assess the following categories: (i) radiation protection,(ii) equipment operation and maintenance, (iii) image production and evaluation,(iv) radiographic procedures, and (v) patient care. Examinees are given 3.5 hoursto complete the exam, and testing centers provide an erasable board and pen (noscratch paper is allowed). A scientific calculator is available on the computer, orone will be provided if requested. Each version of the ARRT exam is score scaled,based on the overall difficulty accounting for slight variations in exam versions. Ascaled test score of 75 is required to pass the ARRT exam. Further information on theAmerican Registry of Radiologic Technologists can be obtained at the ARRT web site(www.arrt.org).10:22
P1: PBULWBK312-FMLWBK312-HudaJune 19, 2009xvi10:22
P1: OSOLWBK312-01LWBK312-HudaMarch 10, 20091ChapterX-RAY PRODUCTIONI. BASIC PHYSICSA. Forces–The mass of a body is a measure of its resistance to acceleration.–Mass is measured in kilograms (kg).–Velocity is the speed of a body moving in a given direction.–Velocity is measured in meters per second (m/s).–Acceleration is the rate of change of velocity.–Acceleration is measured in meters per second squared (m/s2 ).–A force causes a body to deviate from a state of rest or constant velocity (push orpull).–Force mass acceleration, measured in newtons (N).–The four physical forces in the universe are gravitational, electrostatic, strong, andweak.–Relative strengths of these four forces are listed in Table 1.1.–Gravity pulls objects to the Earth, and is important in cosmology.–At the atomic level, effects of gravity are extremely small and are ignored.–The electrostatic force causes protons and electrons to attract each other.–Electrostatic forces hold atoms together.–Strong forces hold the nucleus together.–Weak forces are involved in beta decay.B. Energy–Energy is the ability to do work.–Energy is measured in joules (J).–Energy takes on various forms including electrical, nuclear, chemical, and thermal.–One common form of energy is kinetic energy (KE) caused by motion.–A bullet with mass m and velocity v has a kinetic energy of 1/2 mv2 .–Another form of energy is potential energy (PE), which is the energy of position.–A raised ball has potential energy.–Energy cannot be created or destroyed.–When a ball is released at a height, potential energy is converted into kinetic energyas the ball’s velocity increases.–Einstein showed that mass and energy are interchangeable.–E mc2 where E is energy, m is mass, and c is the velocity of light.–Rest mass energy is the energy equivalence of a particle.–In diagnostic radiology, the electron volt (eV) is a convenient unit of energy.–1 eV 1.6 10 19 J–One electron volt (1 eV) is the kinetic energy gained by an electron when it is acceleratedacross an electric potential of 1 volt (V) as depicted in Figure 1.1.–An electron gains 1,000 eV (1 keV) when accelerated across an electric potential of 1,000V.–An electron gains 1 MeV (1,000 keV) when accelerated across an electric potential of1,000,000 V.–1 MeV 103 keV 106 eVC. Electricity–Electrons are negatively charged and protons are positively charged.–Electric charge of an electron (or proton) is 1.6 10–19 coulomb (C).110:17
P1: OSOLWBK312-01LWBK312-Huda2March 10, 2009X-ray ProductionTABLE 1.1 Relative Strength of Physical ForcesType of ForceGravitationalWeakElectrostaticStrongRelative Strength1 1024 1035 1038DescriptionBinds earth to the sunInvolved in beta decayBinds electrons and protons in atomsBinds protons and neutrons in the nucleus–Applying a voltage in an electrical circuit causes electrons to move.–The positive region of an electrical circuit is called the anode.–The negative region is called the cathode.–Electrons are repelled from the cathode and attracted to the anode.–Any voltage source in a complete circuit results in a flow of electrons in the circuit.–Electric current, measured in amperes (A), is the flow of electrons through a circuit.–An ampere is the amount of charge that flows divided by time.–1 ampere 1 coulomb per second–Power supplies in any domestic home have a minimum of two wires and are singlephase.–Single-phase power supplies have one wire that has an oscillating voltage, with theother carrying no voltage.–If there is a third wire, this is an “earth connection’’ for safety.–In the United States, the electric power supply from utility companies is normally 110volts (V).–U.S. electricity is an alternating current (AC) that oscillates at a frequency of 60 cyclesper second (60 Hz).–In Britain, AC voltage is 220 V and oscillates at a frequency of 50 cycles per second(50 Hz).–Three-phase power supplies have three lines of voltage, each 120 degrees out of phasewith the others.–Three-phase power supplies provide much more power than single phase.D. Power–Power is the rate of performing work.–Power is the energy used divided by time, measured in watts (W).–1 watt 1 joule per second–Table 1.2 lists the power and energies of a range of sources.–1 horsepower (HP) corresponds to 750 W.–In electric circuits, the power (P) dissipated is the product of electric current (I) andvoltage (V).–Power (watt) current (ampere) voltage (volt)–If the voltage is 100,000 V (100 kV) and the current is 1 A (1,000 mA), the power dissipatedis 100,000 W (100 kW).–A typical household in North America uses a few kW of electrical power.–X-ray generators use up to 100 kW of electrical power, or the power required for 30U.S. households.FIGURE 1.1 At the negatively charged plate, the electron has potential energy of 1 eV, which isconverted into a kinetic energy of 1 eV as the electron is accelerated from the cathode to the anode.10:17
P1: OSOLWBK312-01LWBK312-HudaMarch 10, 2009Electromagnetic Radiation3TABLE 1.2 Common Power SourcesSourceFlashlightDomestic light bulbMicrowaveAverage U.S. homeX-ray generatorPower (W)Energy Used per Second (J)2505003,000100,0002505003,000100,000–The total energy generated is the product of power and time.–Energy (joule) power (watt) time (second)–X-ray generators are only switched on for short periods of time.–A typical exposure time for a chest x-ray examination is 10 ms.–Energy utilization in making x-rays is therefore low because of the very short exposuretimes that are used.II. ELECTROMAGNETIC RADIATIONA. Waves–A wave is an entity that varies in space and time.–A common example of a wave is the variation of the water level in the ocean.–Waves are characterized by a wavelength, frequency, and velocity.–Wavelength (λ) is the distance between successive crests of waves.–Wavelengths are measured in meters (m).–Frequency (f) is the number of wave oscillations per unit of time.–Frequencies are measured in cycles per second, where one cycle per second is equalto one hertz (Hz).–The wave period is the time required for one wavelength to pass.–Wave period is 1/f.–The wave velocity (v) is the product of the wavelength and frequency, and measured inmeters per second (m/s).–Velocity (m/s) frequency (Hz) wavelength (m)–Electromagnetic radiation is a wave that is associated with oscillating electric and magnetic fields.–Visible light is a form of electromagnetic radiation.–The sun emits (loses) the energy that it generates in nuclear processes by radiating visiblelight.B. X-rays–X-rays are a form of electromagnetic radiation.–Electromagnetic radiation represents a transverse wave, in which the electric and magnetic fields oscillate perpendicular to the direction of the wave motion.–Electromagnetic radiation travels in a straight line at the speed of light (c).–The value of c is 3 108 m/s in a vacuum.–The product of the wavelength (λ) and frequency (f) of electromagnetic radiation is equalto the speed of light (c fλ).–Low-frequency electromagnetic radiation has a long wavelength.–High-frequency electromagnetic radiation has a short wavelength.–Figure 1.2 shows the electromagnetic spectrum that ranges from radio waves to gammarays.C. Photons–Electromagnetic radiation is quantized, meaning that it exists in discrete quantitiescalled photons.–Photons may behave as waves or particles but have no mass.–Photon energy (E) is directly proportional to frequency.–Photon energy is inversely proportional to wavelength.–Photon energy is E h f h (c/λ), where h is Plank’s constant.–A 10-keV photon has a wavelength of 0.1 nm, comparable to the size of a small atom.–A 100-keV photon has a wavelength of 0.01 nm.10:17
P1: OSOLWBK312-01LWBK312-Huda4March 10, 2009X-ray ProductionFIGURE 1.2 Electromagnetic spectrum ranging from radio waves to gamma rays showing that thephoton energy is directly proportional to frequency.–Radio waves have low frequencies (low photon energies) and gamma waves have highfrequencies (high photon energies) as depicted in Figure 1.2.–High energy photons are called x-rays if produced by electron interactions but gammarays if produced in a nuclear process.–There are no physical differences between x-rays and gamma rays of the same energy.D. Inverse square law–The intensity of an x-ray beam is proportional to the number of photons crossing a givenarea (e.g., square millimeter).–X-ray beam intensity decreases with distance from the x-ray tube because of the divergence of the x-ray beam.–The decrease in intensity is proportional to the square of the distance from the source.This nonlinear falloff in intensity with distance is called the inverse square law.–Doubling the distance from the x-ray source decreases the x-ray beam intensity by afactor of 4.–Halving the distance increases the x-ray beam intensity by a factor of 4.–Table 1.3 shows how increasing and decreasing the distance from a source of radiationchanges the radiation intensity.–In general, if the distance from the x-ray source is changed from x1 to x2 , then the x-raybeam intensity changes by (x1 /x2 )2 .III. X-RAY GENERATORSA. Generator role–X-ray generators provide electrical power to the x-ray tube.–A small fraction of this power ( 1%) is converted into x-rays.–Virtually all current x-ray generators in Radiology departments use three-phase powersupplies.TABLE 1.3 Relative Radiation Intensity as a Function of Distance from the RadiationSource (Inverse Square Law)Distance from Radiation Source (m)0.10.250.512410The intensity at 1 m has been arbitrarily set to 1.0.Intensity (Relative to Intensity at 1 m)10016411/41/161/10010:17
P1: OSOLWBK312-01LWBK312-HudaMarch 10, 2009X-ray Generators5–A generator uses a transformer to increase the voltage that is applied across the x-raytube.–The generator also rectifies the waveform from AC to direct current (DC).–Generators permit x-ray operators to control three key parameters of x-ray operation.–The tube voltage (kV) that is applied across the x-ray tube.–The current (mA) that flows through the x-ray tube.–The total exposure time (seconds) for which the tube current flows.–The power dissipated equals the product of tube voltage (V) in volt and current (I) inamps, or VI, and is measured in watts (kW).–Typical transformer ratings in x-ray departments are 100 kV and 1,000 mA, which correspond to a power of 100 kW.B. Generator types–Generators consist of an input power supply, transformer, and rectification circuit.–Single-phase generators use a single-phase power supply.–Single-phase generators use a bridge rectifier circuit that
IV. Radiology Residents and the ABR Exam xiv V. Radiology Technologists and the ARRT Exam xv 1 X-RayProduction 1 I. Basic Physics 1 II. Electromagnetic Radiation 3 III. X-ray Generators 4 IV. Making X-rays 6 V. X-ray Tubes 9 VI. X-ray Tube Performance 11 Review Test 14 Answers and Explanati