Transcription
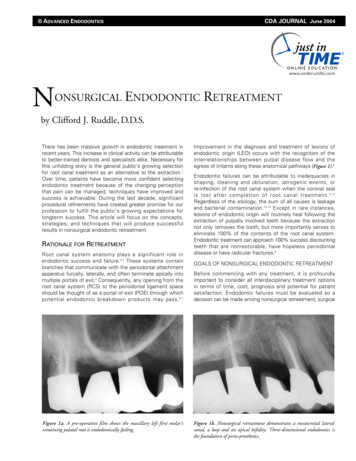
ADVANCED ENDODONTICSNONSURGICALCDA JOURNAL June 2004ENDODONTIC RETREATMENTby Clifford J. Ruddle, D.D.S.There has been massive growth in endodontic treatment inrecent years. This increase in clinical activity can be attributableto better-trained dentists and specialists alike. Necessary forthis unfolding story is the general public's growing selectionfor root canal treatment as an alternative to the extraction.1Over time, patients have become more confident selectingendodontic treatment because of the changing perceptionthat pain can be managed, techniques have improved andsuccess is achievable. During the last decade, significantprocedural refinements have created greater promise for ourprofession to fulfill the public’s growing expectations forlongterm success. This article will focus on the concepts,strategies, and techniques that will produce successfulresults in nonsurgical endodontic retreatment.RATIONALE FOR RETREATMENTRoot canal system anatomy plays a significant role inendodontic success and failure.2-4 These systems containbranches that communicate with the periodontal attachmentapparatus furcally, laterally, and often terminate apically intomultiple portals of exit.5 Consequently, any opening from theroot canal system (RCS) to the periodontal ligament spaceshould be thought of as a portal of exit (POE) through whichpotential endodontic breakdown products may pass. 6,7Figure 1a. A pre-operative film shows the maxillary left first molar’sremaining palatal root is endodontically failing.Improvement in the diagnosis and treatment of lesions ofendodontic origin (LEO) occurs with the recognition of theinterrelationships between pulpal disease flow and theegress of irritants along these anatomical pathways (Figure 1).8Endodontic failures can be attributable to inadequacies inshaping, cleaning and obturation, iatrogenic events, orre-infection of the root canal system when the coronal sealis lost after completion of root canal treatment. 9-12Regardless of the etiology, the sum of all causes is leakageand bacterial contamination. 13,14 Except in rare instances,lesions of endodontic origin will routinely heal following theextraction of pulpally involved teeth because the extractionnot only removes the tooth, but more importantly serves toeliminate 100% of the contents of the root canal system.Endodontic treatment can approach 100% success discountingteeth that are nonrestorable, have hopeless periodontaldisease or have radicular fractures.8GOALS OF NONSURGICAL ENDODONTIC RETREATMENTBefore commencing with any treatment, it is profoundlyimportant to consider all interdisciplinary treatment optionsin terms of time, cost, prognosis and potential for patientsatisfaction. Endodontic failures must be evaluated so adecision can be made among nonsurgical retreatment, surgicalFigure 1b. Nonsurgical retreatment demonstrates a mesiocrestal lateralcanal, a loop and an apical bifidity. Three-dimensional endodontics isthe foundation of perio-prosthetics.
ADVANCED ENDODONTICS - www.endoruddle.comretreatment, or extraction. 15-17 The goals of nonsurgicalretreatment are to remove materials from the root canalspace and if present, address deficiencies or repair defectsthat are pathologic or iatrogenic in origin. 18 Additionally,nonsurgical retreatment procedures confirm mechanical failures,previously missed canals or radicular subcrestal fractures.Importantly, disassembly and corrective procedures allowclinicians to shape canals and three-dimensionally clean andpack root canal systems.19,20 Nonsurgical endodontic retreatment procedures have enormous potential for success if theguidelines for case selection are respected and the mostrelevant technologies, best materials and precise techniquesare utilized.21-23NONSURGICAL ENDODONTIC RETREATMENT 2it may be desirable to remove the restoration intact so it canbe re-cemented following endodontic treatment.18 Severalimportant technologies exist which facilitate the saferemoval of a restorative. Coronal disassembly improvesaccess, vision and the retreatment efforts.Clinicians typically access the pulp chamber through anexisting restoration if it is judged to be functionally designed,well-fitting and esthetically pleasing.24 If the restoration isdeemed inadequate and/or additional access is required,then it should be sacrificed. However, on specific occasions,The safe dislodgment of a restoration is dependent on severalfactors such as the type of preparation, the restorative designand strength, the restorative material(s), the cementing agentand knowing how to use the best removal devices. There areseveral important removal devices which may be divided intothree categories: (1) Grasping instruments, such as K.Y.Pliers (GC America) and Wynman Crown Gripper (MiltexInstrument Company), (2) Percussive instruments like thePeerless Crown-a-Matic (Henry Schein) and the Coronaflex(KaVo America), and (3) Passive-active instruments such asthe Metalift (Classic Practice Resources), the Kline CrownRemover (Brasseler) and the Higa Bridge Remover (HigaManufacturing). Clinicians must clearly define the risk versusbenefit with patients before commencing with the safe andintact removal of an existing restorative (Figure 2).Figure 2a. A photograph demonstrates removal of a crown utilizing theK.Y. Pliers. Note the grasping pads have been dipped in emery powder toreduce slippage.Figure 2b. A photograph demonstrates bridge removal utilizing theCoronaflex. The air driven hammer generates the removal force againstvarious prosthetic attachment devices.CORONAL ACCESSFigure 2c. A photograph demonstrates the removal of a PFM crownutilizing the Metalift. This system applies a force between the crown andthe tooth.
ADVANCED ENDODONTICS - www.endoruddle.comMISSED CANALSMissed canals hold tissue, and at times bacteria and relatedirritants that inevitably contribute to clinical symptoms andlesions of endodontic origin.9 Oftentimes, surgical treatmenthas been directed towards “corking” the end of the canalwith the hopes that the retrograde material will incarceratebiological irritants within the root canal system over the lifeof the patient. 14 Although this clinical scenario occursanecdotally, it is not as predictable as nonsurgical retreatment. Endodontic prognosis is maximized in teeth whoseroot canals are shaped and root canal systems cleaned andpacked in all their dimensions (Figure 3).5,8There are multiple concepts, armamentarium and techniquesthat are useful to locate canals. The most reliable method forlocating canals is to have knowledge regarding root canalsystem anatomy and appreciation for the range of variationcommonly associated with each type of tooth.3 Frequentlyused methods for identifying canals include: radiographicanalysis, magnification and lighting (microscopes), completeNONSURGICAL ENDODONTIC RETREATMENT 3access, firm explorer pressure, ultrasonics, Micro-Openers(Dentsply Tulsa Dental), dyes, sodium hypochlorite, colorand texture, removing restorations, and probing the sulcus.However, if a missed canal is suspected but cannot be readilyidentified and treated, then an endodontic referral may beprudent to avoid complications. Caution should be exercisedwhen contemplating surgery due to the aforementionedconcerns, but at times may be necessary to retain the tooth.OBTURATION MATERIALSThere are four commonly encountered obturation materialsfound in root canals. These materials are gutta percha,carrier-based obturators, silver points and paste fillers.Generally it is necessary to remove an obturation material toachieve endodontic retreatment success or to facilitate placinga post for restorative reasons. The effective removal ofan obturation material requires utilizing the most provenmethods from the past in conjunction with the best presentlydeveloped techniques.Figure 3a. A radiograph of a maxillary right second bicuspid revealspins, a post, incomplete endodontics and an asymmetrical lesion.Figure 3b. A photograph at 12x shows the post is out of the buccal canal,thread marks in the gutta percha from the screw post, and evidence of amissed lingual system.Figure 3c. A photograph at 12x demonstrates complete access andidentification of the lingual orifice/system.Figure 3d. A 10-year recall radiograph shows excellent osseous repair, theimportance of 3-D endodontics, and a well-designed and sealed restorative.
ADVANCED ENDODONTICS - www.endoruddle.comNONSURGICAL ENDODONTIC RETREATMENT 4GUTTA PERCHA REMOVALThe relative difficulty in removing gutta percha variesaccording to the obturation technique previously employedand further influenced by the canal’s length, cross-sectionaldimension, curvature and internal configuration. Regardless oftechnique, gutta percha is best removed from a root canalin a progressive manner to prevent inadvertent displacementof irritants periapically. Dividing the root into thirds, guttapercha may be initially removed from the canal in the coronalone-third, then the middle one-third, and finally eliminatedfrom the apical one-third. At times, single cones in largerand straighter canals can be removed with one instrumentin one motion. For other canals, there are a number ofpossible gutta percha removal schemes. 18 The removaltechniques include rotary files, ultrasonic instruments,heat, hand files with heat or chemicals, and paper pointswith chemicals.25 Of these options, the best technique(s)for a specific case is selected based on preoperativeradiographs, clinically assessing the available diameter ofthe orifices after re-entering the pulp chamber, and clinicalexperience. Certainly, a combination of methods are generallyrequired and, in concert, provide safe, efficient and potentiallycomplete elimination of gutta percha and sealer from theinternal anatomy of the root canal system (Figure 4).Figure 4a. A preoperative radiograph of a maxillarycentral incisordemonstrates inadequate endodontics,resorption and apicalone-third pathology.Figure 4b. A photograph at 8x shows a 45 hedstroem mechanicallyremoving the heat softened single cone of gutta percha.Figure 4c. A post-operative radiograph showsthe nonsurgical retreatment result and threedimensional obturation.
ADVANCED ENDODONTICS - www.endoruddle.comNONSURGICAL ENDODONTIC RETREATMENT 5SILVER POINT REMOVALThe relative ease of removing a silver point is based on thefact that chronic leakage reduces the seal and hence, thelateral retention. Access preparations must be thoughtfullyplanned and carefully performed to minimize the risk ofinadvertently foreshortening any given silver point. Initialaccess is accomplished with highspeed, surgical length cuttingtools, then oftentimes ultrasonic instruments are used tobrush-cut away remaining restorative materials and fullyexpose the silver point.Different techniques have been developed for removing silverpoints depending on their lengths, diameters, and positionsthey occupy within the root canal space (Figure 5).23,26,27 Certainremoval techniques evolved to address silver points that bindin unshaped canals over distance. Other techniques arose toremove silver points with large cross-sectional diameters,approaching the size of smaller posts. Finally, othertechniques are necessary to remove intentionally sectionedsilver points lying deep within the root canal space. The moreeffective methods for removing silver points include: graspingpliers utilizing the principles of fulcrum mechanics, indirectFigure 5a. A pre-operative radiograph depicting an endodonticallyfailing maxillary central incisor bridge abutment, a gutta perchapoint tracing a fistulous tract to a large lateral root lesion, and acanal underfilled and slightly overextended.Figure 5b. Magnification at 15x revealslingual access andrestorative build-uparound the coronalmost aspect of theexposed silver point.5a5bFigure 5c. A working radiograph during thedownpack reveals apical and lateral corkage.Figure 5d. A 5-year review demonstrates thatthree-dimensional endodontic treatmentpromotes healing.5c5d
ADVANCED ENDODONTICS - www.endoruddle.comNONSURGICAL ENDODONTIC RETREATMENT 6ultrasonics, files, solvents, chelators, the hedstroem displacement technique, tap and thread option using the microtubulartaps from the Post Removal System kit (SybronEndo), andmicrotube mechanics such as the Instrument RemovalSystem (Dentsply Tulsa Dental).18appreciate the importance of first removing circumferentialgutta percha which will facilitate removing the carrierbased obturator.CARRIER REMOVALWhen evaluating a paste case for retreatment, it is useful toclinically understand that pastes can generally be dividedinto soft, penetrable and removable versus hard, impenetrable,and at times, unremovable. Fortuitously, the paste is moredense in the coronal portion of the canal and the material isprogressively less dense moving apically due to the methodof placement (Figure 7). Before retreating a paste-filled canal,the clinician should anticipate calcifications, resorptions, andthe possibility that the removal efforts may be unsuccessful.Importantly, patients should be advised there could bea higher incidence of flare-ups associated with theseretreatment cases.Gutta percha carriers were originally metal and file-like, yetover the past several years they have been manufacturedfrom easier-to-remove plastic carriers that have a longitudinalgroove. Metal carriers, although no longer distributed, areoccasionally encountered clinically and can be more difficultto remove than silver points because their cutting flutes attimes engage lateral dentin. 28 Successful removal isenhanced by recognizing that the carrier is frozen in a sea ofhardened gutta percha and sealer. The successful removalof carrier-based obturators utilizes the same techniquesdescribed for removing gutta percha and silver points. 18However, successful removal poses additional challenges tothe aforementioned obturation techniques in that the clinicianmust remove both the gutta percha and the carrier (Figure 6).Oftentimes, the biggest secret to remove a carrier is toPASTE REMOVALAn excellent technique for the safe removal of hard,impenetrable paste from the straightaway portion of a canalutilizes abrasively coated ultrasonic instruments in conjunctionwith the microscope. To remove paste apical to canal curvature,Figure 6a. A radiograph of a maxillary right first molar demonstrates“coke bottle” preparations and carrier-based obturation of three canals.Figure 6b. A post-operative radiograph reveals the retreatment efforts,including the identification and treatment of a second MB root canal system.Figure 7a. A pre-operative radiograph of an endodontically failing pastefilled mandibular left second molar. Note the extra DL root.Figure 7b. A 5-year recall film shows the treatment of multiple apicalportals of exit and excellent osseous healing.
ADVANCED ENDODONTICS - www.endoruddle.comNONSURGICAL ENDODONTIC RETREATMENT 7hand instruments should first be utilized to establish orconfirm a safe glide path. Precurved stainless steel handfiles may be inserted into this secured region of the canaland when attached to a “file adapter”, may be activatedutilizing ultrasonic energy.18 Other removal methods includeheat, judicious use of end-cutting rotary NiTi instrumentsand small sized hand files with solvents such as Endosolv Rand Endosolv E (Endoco).29 Additionally, Micro-Debriders(Dentsply Maillefer) and paper points in conjunction withsolvents play an important role in removing paste fromcanal irregularities.post diameter, length and the cementing agent. Other factorsthat will influence removal are whether the post is parallelversus tapered, stock versus cast, actively engaged versusnon-actively retained, metallic versus non-metallic compositions, and the post head configuration. Additionally, otherconsiderations include available interocclusal space, existingrestorations and if the post head is supra- or sub- crestal.Over time, many techniques have been advocated forremoval of posts. 31 Before initiating any post removalmethod, all materials circumferential to the post must beeliminated and the orifice to the canal visualized (Figure 8).ULTRASONIC OPTIONPOST REMOVALEndodontically treated teeth frequently contain posts thatneed to be removed to facilitate successful nonsurgicalretreatment.30 Factors that will influence post removal are8aThe first line of offense to remove a post is to utilize piezoelectric ultrasonic energy. An ultrasonic generator inconjunction with the correct insert instrument will transferenergy, powerfully vibrate, and dislodge most posts. A frequent8bFigure 8a. A pre-operative radiograph of amandibular right second molar bridgeabutment demonstratesthree posts, previousendodontics, andapical pathology.Figure 8b. Followingcoronal disassembly, theisolated tooth revealsthe core sectioned andreduced. Ultrasonicsmay then be utilized toeliminate all restorative materials circumferential to the posts.Figure 8c. The pulpalfloor is shown followingthree-dimensionalcleaning, shaping, andobturation procedures.Note the displacedmost lingual orifice.8c8dFigure 8d. A mesiallyangulated post-operativeradiograph confirmsthe disassembly efforts,demonstrates the packand the displacedlingual system.
ADVANCED ENDODONTICS - www.endoruddle.comand intermittent air/water spray is directed on the post toreduce heat buildup and transfer during ultrasonic removalprocedures. The majority of posts can be safely andsuccessfully removed with ultrasonics in about 10 minutes.32PRS OPTIONThe Post Removal System (PRS) is a reliable method toremove a post when ultrasonic efforts using the “10-MinuteRule” prove unsuccessful. 18 In this removal method atrephine is used to machine down the most coronal aspect ofthe post 2-3 mm. The correspondingly sized tap is selectedand an appropriately sized protective bumper is inserted ontothis instrument. The tap is turned in a counterclockwisedirection to form threads and securely engage the post head.Once the tap is firmly engaged on the post and the protectivebumper seated, then the extracting pliers are used to safelyand progressively elevate the post out of the canal.SEPARATED INSTRUMENT REMOVALNONSURGICAL ENDODONTIC RETREATMENT 8a reduced speed of about 750 RPM. Importantly, in multirooted teeth, GG’s may be used from small to big to cut andremove dentin on the outer wall of the canal and away fromfurcal danger. Each larger GG is stepped out of the canal tocreate a uniform tapered and smooth flowing funnel. The goalof radicular access is to optimally prepare a canal no largerthan if there was no broken instrument.ULTRASONIC OPTIONIn combination, microscopes and ultrasonics have driven“microsonic” techniques that have improved the potential,predictability and safety when removing broken instruments.18When access and visibility to the head of the broken instrument are achieved then contra-angled, parallel-walled andabrasively-coated ultrasonic instruments (ProUltra Endo Tips #3,4, 5) may be employed. When energized, these instrumentsmay be used to precisely sand away dentin and trephinecircumferentially around the obstruction. During the ultrasonicprocedure, the broken instrument will typically loosen, unwindand spin, then “jump out” of the canal (Figure 9).Technological advancements have significantly increased thepredictability in removing separated instruments. Theseadvancements include the dental operating microscope, ultrasonic instrumentation, and microtube delivery methods.18 Theability to access and remove a broken instrument will be influenced by the cross-sectional diameter, length and curvatureof the canal, and further guided by root bulk and form includingthe depth of external concavities. In general, if one-third of theoverall length of an obstruction can be exposed, it can usuallybe removed. Instruments that lie in the straightaway portionsof the canal or partially around the curvature can usually beremoved if safe access can be established to its most coronalextent.33,34 If the entire segment of the broken instrument isapical to the curvature of the canal and safe access cannot beaccomplished, then removal is usually not possible.The techniques required to remove a broken instrument beginwith establishing straightline coronal access. To create radicularaccess, hand files may be used serially small to large, coronalto the obstruction, to create sufficient space to safely introducegates glidden (GG) drills. GG’s are used like “brushes” and atFigure 9a. A pre-operative radiograph shows a strategic and endodontically failing mesial root of a mandibular left first molar. Note a shortscrew post, a separated instrument and amalgam debris from thehemisection procedures.Figure 9b. A photograph shows the splint removed, the post out and anultrasonic instrument trephining around the broken file.Figure 9c. An 8-year recall film demonstrates three-dimensional retreatment, a new bridge and excellent periradicular healing.
ADVANCED ENDODONTICS - www.endoruddle.comNONSURGICAL ENDODONTIC RETREATMENT 9iRS OPTIONWhen ultrasonic techniques fail, the fall-back option is touse the Instrument Removal System (iRS) (Dentsply TulsaDental). The iRS is composed of variously sized microtubesand screw wedges. Each microtube has a small handle toenhance vision and its distal end is constructed with a 45 beveled end and side window. The appropriately sizedmicrotube is inserted into the canal and, in the instance ofcanal curvature, the long part of its beveled end is orientedto the outer wall of the canal to “scoop-up” the head of thebroken instrument and guide it into its lumen. The screwwedge is then placed through the open end of the microtube and passed down its internal lumen until it contactsthe broken instrument. Rotating the screw wedge handletightens, wedges, and oftentimes, displaces the head of thefile through the microtube’s side window.18 With the brokeninstrument strongly engaged, it can generally be rotatedcounterclockwise and removed (Figure 10).BLOCKS, LEDGES, TRANSPORTATIONS& PERFORATIONSFailure to respect the biological and mechanical objectives forshaping canals and cleaning root canal systems predisposes toneedless complications such as blocks, ledges, external transportations and perforations. These iatrogenic events can beattributable to working short, the sequence utilized for preparing the canal, and the instruments and their method of use.19TECHNIQUES FOR MANAGING BLOCKSTechniques for managing blocked canals begin by confirmingstraightline access and then pre-enlarging the canal coronalto the obstruction. 18 A 10 file provides rigidity and isprecurved to simulate the expected curvature of the canalFigure 10a. A pre-operative radiograph of amaxillary canine demonstrates a temporizedcanal with an instrument broken deep in theapical one-third.and the unidirectional rubber stop is oriented to match thefile curvature. With the pulp chamber filled with a viscouschelator, efforts are directed towards gently sliding the 10file to length. If unsuccessful, the file is used with an apicallydirected picking action while concomitantly re-orienting theunidirectional stop which serves to re-direct the apicalaspect of the precurved file. Short amplitude, light peckingstrokes are best utilized to ensure safety, carry reagentdeeper, and increase the possibility of canal negotiation. Ifthe apical extent of the file “sticks” or engages, then it maybe useful to move to a smaller sized hand file. A workingfilm should be taken and the file frequently removed to seeif its curve is following the expected root canal morphology.Depending on the severity of the blockage, perseverancewill oftentimes allow the clinician to safely reach theforamen and establish patency (Figure 11). If the blockedcanal is not negotiable, then the case should be filled utilizinga hydraulic warm gutta percha technique. Regardless of thepacking result, the patient needs to be advised of theimportance of recall and that future treatment optionsinclude surgery, re-implantation, or extraction.TECHNIQUES FOR MANAGING LEDGESAn internal transportation of the canal is termed a “ledge” andfrequently results when clinicians work short of length and“get blocked”. Ledges are typically on the outer wall of the canalcurvature and are oftentimes bypassed using the techniquesdescribed for blocks.13,18 Once the tip of the file is apical to theledge, it is moved in and out of the canal utilizing ultra-shortpush-pull movements with emphasis on staying apical to thedefect. When the file moves freely, it may be turned clockwiseupon withdrawal to rasp, reduce, smooth or eliminate theledge. During these procedures, try to keep the file coronal tothe terminus of the canal so the apical foramen (foramina) ishandled delicately and kept as small as practical. When theFigure 10b. A working film shows that the 21gauge iRS has successfully engaged and partiallyelevated the deeply positioned file segment.Figure 10c. A post-operative film demonstratesthe retreatment steps and a densely packedsystem that exhibits three apical portals of exit.
ADVANCED ENDODONTICS - www.endoruddle.comNONSURGICAL ENDODONTIC RETREATMENT 10Figure 11a. A pre-operative radiograph of a maxillary left secondbicuspid reveals previous access and pre-enlargement of the canal in itscoronal two-thirds.Figure 11b. The post-operative radiograph provides an explanation as tothe etiology of the original block. Note the canal bifurcates apically andthis system has four portals of exit.ledge can be predictably bypassed, then efforts are directedtowards establishing patency with a 10 file. Gently passing a.02 tapered 10 file 1 mm through the foramen insures itsdiameter is at least 0.12 mm and paves the way for the 15 file.22or perforate the root. Not all ledges can or should beremoved. Clinicians must weigh risk versus benefit andmake every effort to maximize remaining dentin (Figure 12).A significant improvement in ledge management is theutilization of nickel-titanium (NiTi) hand files that exhibittapers greater than ISO files.18 Certain NiTi instruments havemultiple increasing tapers over the length of the cuttingblades on the same instrument (ProTaper, Dentsply TulsaDental). Progressively tapered NiTi files can be introducedinto the canal when the ledge has been bypassed, the canalnegotiated and patency established. Bypassing the ledgeand negotiating the canal up to a size 15, and if necessary a20, file creates a pilot hole so the tip of the selected NiTiinstrument can passively follow this glide path. To move theapical extent of a NiTi hand file past a ledge, the instrumentmust first be precurved with a device such as Bird Beakorthodontic pliers (Hu-Friedy). Ultimately, the clinician mustmake a decision based on pre-operative radiographs, rootbulk and experience whether the ledge can be eliminatedthrough instrumentation or if these procedures will weakenA canal that has been transported exhibits reverse apicalarchitecture and predisposes to poorly packed canals that areoftentimes vertically overextended but internally underfilled.8,13In these instances, a barrier/restorative can be selected tocontrol bleeding and provide a backstop to pack against duringsubsequent obturation procedures. The barrier of choice for atransportation is generally mineral trioxide aggregate (MTA)(Dentsply Tulsa Dental), commercially known as ProRoot. MTAis an extraordinary material which can be used in canals whichexhibit reverse apical architecture, such as in transportations orimmature roots, nonsurgical perforation repairs, or in surgicalrepairs.18,35,36 Remarkably, cementum grows over this nonresorbable and radiopaque material, thus allowing for a normalperiodontal attachment apparatus.37-39 Although a dry fieldfacilitates visual control, MTA is apparently not compromisedby moisture and typically sets brick-hard within 4-6 hours,creating a seal as good as or better than other materials.40-42Figure 12a. A pre-operative radiograph shows an endodontically failingposterior bridge abutment. Note the amalgam in the pulp chamber andthat the mesial root appears to have been ledged.Figure 12b. A post-treatment film demonstrates ledge management withthe obturation materials following the root curvature.TECHNIQUES FOR MANAGING APICAL TRANSPORTATIONS
ADVANCED ENDODONTICS - www.endoruddle.comNONSURGICAL ENDODONTIC RETREATMENT 11Techniques for managing apical transportations are facilitatedwhen the coronal two-thirds of the canal is optimally prepared and radicular access is available for placing a barrier.ProRoot is easy to use and the powder is mixed withanesthetic solution or sterile water to a heavy cake-likeconsistency. MTA may be picked up and efficiently carriedinto more superficial regions of the tooth on the side of aWest Perf Repair Instrument (SybronEndo). To moreprecisely introduce MTA deep into a prepared canal microtube carrying devices or the Lee carrier method (G. Hartzell& Sons) are appropriately sized to accomplish this task.18,35,43ProRoot is then gently tamped down the canal to approximatelength using a customized nonstandard gutta percha cone asa flexible plugger. In straighter canals, ProRoot can be gentlyvibrated, moved into the defect and adapted to the canalwalls with ultrasonic instruments (ProUltra Endo Tips,Dentsply Tulsa Dental) Direct ultrasonic energy will vibrateand generate a wave-like motion which facilitates movingand adapting the cement into the apical extent of the canal.Prior to initiating subsequent procedures, a dense 4-5 mmzone of ProRoot in the apical one-third of the canal shouldbe confirmed radiographically (Figure 13).13aIn the instance of repairing a defect apical to the canalcurvature, ProRoot is incrementally placed deep into a canalthen shepherded around the curvature with a flexible, trimmedgutta percha cone utilized as a plugger. A precurved 15 or 20stainless steel file is then inserted into the ProRoot and to
Figure 1a. A pre-operative film shows the maxillary left first molar’s remaining palatal root is endodontically failing. Figure 1b. Nonsurgical retreatment demonstrates a mesiocrestal lateral . Three-dimensional end