Transcription
Boards & Beyond:Pathology SlidesColor slides for USMLE Step 1 preparationfrom the Boards and Beyond WebsiteJason Ryan, MD, MPH2021 EditionBoards & Beyond provides a virtual medical school curriculm usedby students around the globe to supplement their education andprepare for board exams such as USMLE Step 1.This book of slides is intended as a companion to the videos foreasy reference and note-taking. Videos are subject to changewithout notice. PDF versions of all color books are available via thewebsite as part of membership.Visit www.boardsbeyond.com to learn more.Copyright 2021 Boards and BeyondAll rights reserved.i
ii
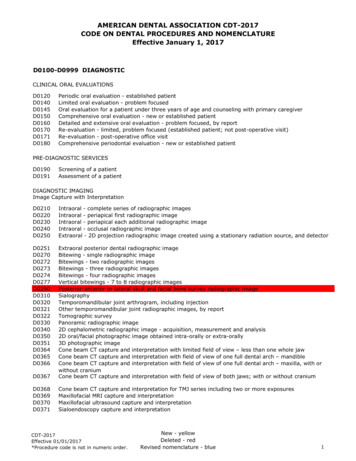
Table of ContentsCellular Adaptations .1Cellular Injury .5Free Radicals .7Apoptosis . 11Necrosis . 15Inflammation Principles . 20Acute and Chronic Inflammation . 26Granulomatous Inflammation . 30Pathologic Calcification . 32Wound Healing and Scar . 35Neoplasia . 41iii
iv
Cellular AdaptationsCellular Response to Stress Stressors Pathologic: ischemia Physiologic: pregnancyCellularAdaptations Adaptation Reversible change in response to stress Injury Reversible irreversible Cell deathJason Ryan, MD, MPHNormalCellular AdaptationsAdaptationInjuryHypertrophy Increase in cell size Hypertrophy Increase in cell size More proteins, filaments Hyperplasia May occur together with hyperplasia Muscle tissue: hypertrophy with more workload Increase in cell number Often occurs with hypertrophy Atrophy Decrease in cell size Metaplasia Change in phenotypeLin Mei/FlikrHypertrophyHyperplasia Physiologic examples Body builders (muscle hypertrophy for use) Uterus in pregnancy (hormone driven) Pathologic example: Left ventricular hypertrophyØyvind Holmstad/Wikipedia Response to hypertension or increased workloadPatrick Lynch/Wikipedia1Increase in cell numberOften due to excess hormone stimulationPhysiologic or pathologicOften accompanied by hypertrophyDeath
Physiologic HyperplasiaPathologic Hyperplasia Breast growth at puberty Endometrial hyperplasia Growth due to estrogen Hyperplasia and hypertrophy of glandular epithelial cells Liver regeneration Prostatic hyperplasia Excessive response to androgens Partial liver donation liver grows back to full size Hyperplasia of remaining hepatocytes Human papilloma virus Bone marrow Skin warts (epidermal hyperplasia) Genital warts (mucosal hyperplasia) Anemia hyperplasia of red cell precursors Red blood cell production may increase by 8xWikipedia/Public DomainWikipedia/Public DomainMalignancy Benign Prostatic HyperplasiaOften develops from hyperplasiaIncreased cell divisionMore chances for error in cell cycle controlUncontrolled growth Pathologic hyperplasia Does not lead to malignancyWikipedia/Public DomainWikipedia/Public DomainHypertrophy vs. HyperplasiaAtrophy Reduction in size of organ/tissue Decrease in cell size and/or number of cells Physiologic examples: Permanent/non-dividing cells Myocytes, skeletal muscle cells, nerves Permanent G0 state (“terminally differentiated”) Hypertrophy Embryonic structures (notochord) Uterus after childbirth (loss of hormone stimulation) Breast/uterus at menopause Cells capable of growth/division Epithelial cells (GI tract, breast ducts, skin) Commonly undergo hyperplasia May lead to dysplasia/cancerFlikr/Public Domain2
Pathologic AtrophyAtrophy Mechanisms Unused skeletal muscle Ubiquitin-proteasome pathway Bed rest Immobilization (cast after fracture) Proteins tagged by ubiquitin Transported to proteasomes for degradation Stressors may activate ligases that attach ubiquitin Cachexia Autophagy Poor nutrition “Self eating” Cellular components fused with lysosomes Decreased blood supply Senile atrophy of brain (atherosclerosis) Loss of innervation Neuromuscular disordersCDC/Public DomainMetaplasia MetaplasiaChange in cell type to adapt to stressNew cell type able to withstand stressCommonly from one epithelial cell type to anotherPotentially reversibleCan lead to dysplasia/malignancy Respiratory tract in smokers Pixabay/Public DomainNormal columnar epithelium in trachea/bronchiChanges to squamous epithelium (most common metaplasia)Squamous epithelium more durableLoss of cilia more vulnerable to infectionsCiliated, PS columnarStratified squamous epitheliumOpenStax College/WikipediaMetaplasiaMetaplasia Barrett’s esophagus Myositis Ossificans (heterotopic ossification) Gastric acid (stressor) in esophagus Normal stratified squamous epithelium Changes to columnar epithelium (intestines) Muscle metaplasia to bone (not epithelial cells)Mesenchymal cells osteoblastic tissueForms lamellar bone in musclesFollows trauma (hip arthroplasty)Muscles become stiffTdvorak/WikipediaWikipedia/Public Domain3
Vitamin A DeficiencyApocrine Metaplasia Important for maintaining epithelial cells Deficiency: epithelial metaplasia and keratinization Upper respiratory tract Epithelial metaplasia Epithelium replaced by keratinizing squamous cells Abnormal epithelium pulmonary infections Xerophthalmia (dry eyes)Form of fibrocystic change in breastAlso called “benign epithelial alteration”Alterations to lobular epithelial cellsTake on appearance of apocrine (gland) cellsDoes not lead to dysplasia/cancer Normal epithelium secretes mucus Replaced by keratinized epithelial cellsDysplasiaDysplasia Disordered proliferation Non-neoplastic but can be pre-cancerous Pleomorphism Abnormal nuclei (hyperchromatic, large) Mitotic figures (clumped chromatin) Mild dysplasia may resolve Severe dysplasia may be irreversible cancer Usually occurs in epithelial tissues Usually preceded by hyperplasia or asiaWikipedia/Public DomainCervical DysplasiaNormalDysplasiaEd Uthman/Wikipedia4
Cellular InjuryCell Injury Four general causes of cell injury CellularInjuryCapacity for adaptation exceededExposure to toxic/injurious agentsDeprived of nutrientsMutation disrupts metabolismPixabay/Public Domain Reversible to a point Severe or persistent injury may be irreversible May lead to cell deathJason Ryan, MD, MPHCell DeathReversible Cell Injury Cellular swelling Two ways cells die: Necrosis: inflammatory process Apoptosis: non-inflammatory Necrosis preceded by classic cellular changes Reversible changes irreversible changesReversible Cell InjuryMajor feature of most forms of reversible injuryHydropic change water accumulation in cellHard to see under microscope Na/K ATPase pumpsReversible Cell Injury Fatty change Mitochondrial swelling Membrane blebbing Seen only in systems that heavily metabolize fatty acids Liver, heart, skeletal muscle Lipid vacuoles appear in cytoplasm Disruption of cytoskeleton Dilation of endoplasmic reticulum Public Domain5Ribosomes detach from ER protein synthesis“Polysomal detachment”Polysome cluster of ribosomes
Irreversible Cell InjuryIrreversible Cell InjuryNecrosisClassic Nuclear Changes Membrane damage Karyolysis (loss of basophilic/dark color) Pyknosis (nuclear shrinkage) Karyorrhexis (fragmented nucleus)Contents leakCauses inflammationSerum detection of cell contents (troponin, lipase)Calcium-dependent phospholipases Rupture of lysosomes Enzymes degrade cellular contentsWikipedia/Public DomainWikipedia/Public DomainMechanisms of Injury ATP Depletion Many causesATP depletionCalciumMitochondrial damageFree radicals oxygen supply Mitochondrial damage Direct effect some toxins Loss of membrane pumps Loss of protein synthesisATPCalciumMitochondrial Damage Normally very low compared with outside cell Calcium influx: hallmark of injury Lack of oxygen Reactive oxygen species Mitochondrial permeability transition pore Released from intracellular storage Influx across cell membrane Opened by calcium Loss of membrane potential Failure of oxidative phosphorylation Causes cellular injury Calcium-dependent phospholipases Activated by increased calcium Breakdown of membrane phospholipids Damages mitochondriaBlausen gallery 2014". Wikiversity Journal of Medicine6
Free RadicalsMechanisms of Injury Free RadicalsATP depletionCalciumMitochondrial damageFree radicalsJason Ryan, MD, MPHVocabularyFree Radicals Free radical Single, unpaired electron in outer orbit Highly reactive May damage many cellular components Reactive oxygen species Oxygen free radicalsSeveral formsSuperoxide (O2·)Hydrogen peroxide (H2O2)Hydroxyl radical (OH-)GenerationFree Radical GenerationLow levelFree RadicalsInactivationFree Radical Generation Normal metabolism involving oxygen Oxidative phosphorylation Generated in cells under normal conditionsInactivated in cellsCell maintain low level under normal conditionsHigh level cell injury Yields small levels of superoxide (O2·)Converted to H2O2 by superoxide dismutaseH2O2 more stable and can cross membranesConverted to H2ORadiation (UV light, X-rays)Mechanism of radiation therapy for cancerMetabolism of drugsTransition metalsRespiratory burstO2 O2· H2O2 OH- H2OSuperoxideDismutaseDina Wakulchik/Wikipedia7
Bile Duct Smooth ER in liver Part of phase 1 metabolism Generate “bioactive intermediates” (free radicals)DrugP450Drug-Free-RadicalP450 EnzymesZone IZone IIPeriportalMid ZoneZone IIICentrilobularAcetaminophenLiver LobulesTylenol Metabolized in liver to NAPQI N-acetyl-p-benzoquinone imine2 NAPQI is a reactive oxygen species (ROS) Causes free radical liver damage13CYP450Reytan /WikipediaTransition MetalsTransition Metals Metal storage and transport proteins: Superoxide (O2-) converted to H2O2 for inactivation Fenton Reaction forms hydroxyl radical (OH·) Transferrin/Ferritin/Lactoferrin (Fe) Ceruloplasmin (Cu) H2O2 Fe2 Fe3 OH· H2O2 Cu Cu2 OH· Hemochromatosis/Wilson’s Iron and copper toxicityO2O 2-H2O2OH·TomihahndorfInactivation8Public DomainHepatic VeinPhase 1: drug modificationPhase 2: conjugationPhase 3: additional modification and excretionCytochrome P450 enzymesHepatic Artery Liver ZonesPortal VeinDrug Metabolism
Respiratory BurstRespiratory Burst Phagocytes engulf bacteria in phagosome Generate H2O2 in phagosome to kill bacteria Uses three key enzymes:NADPHOxidase NADPH oxidase Superoxide dismutase MyeloperoxidaseO2O2SuperoxideDismutaseNADPHNADP BacterialDeathH2O2MyeloperoxidaseHOClGraham Colm/WikipediaFree Radical InactivationFree Radical Inactivation Enzymes Spontaneous decay Antioxidants Catalase (peroxisomes) Superoxide dismutase (mitochondria) Glutathione peroxidase (cytoplasm of cells) Free radical scavengers Vitamin E, A, C, glutathioneGenerationLow levelFree RadicalsCl- Requires glutathione: GSH H2O2 H2OCatalaseO2 O2· H2O2 OH- H2OInactivationSuperoxideDismutaseCGDG6PD DeficiencyChronic Granulomatous DiseasePeroxidase Limited supply of glutathione RBC damage by free radicals hemolysis Classic trigger: fava beans Loss of function of NADPH oxidase Phagocytes cannot generate H2O2 Catalase ( ) bacteria breakdown H2O2 Host cells have no H2O2 to use recurrent infections Contain vicine Converted to divicine ROS Depletes glutathione Catalase (-) bacteria generate their own H2O2 Phagocytes use despite enzyme deficiency Five organisms cause almost all CGD infections: Staph aureus, Pseudomonas, Serratia, Nocardia, AspergillusSource: UpToDate9
Free Radical Cell DamageReperfusion Injury Peroxidation of lipids Peroxide: O-O Damages membranes Oxidation of proteins Myocardial infarction blood flow (ischemia) Reperfusion blood flowLipid Peroxidation Some reversibly injured cells recover (good) Some cells damaged by reperfusion (bad - paradoxical) Damage enzymes Several mechanisms oxygen supply generation of free radicals Disruption of DNA Breaks, crosslinking Antioxidants lost from injury Damaged mitochondria incompletely reduce oxygenCarbon TetrachlorideLipofuscinCCL4 Industrial solventHistorically used for dry cleaningLiver highly sensitive to damageConverted to CCL3 free radical (CYP450 enzymes) Lipid peroxidation Inhibition of lipoprotein synthesis/secretion Accumulation of lipids Result: fatty liverLipofuscinWikipedia/Public Domain10Insoluble cellular pigmentYellow-brown colorContain oxidized lipidsThought to be derived from lipid peroxidationAccumulates over time in lysosomesNot pathologicalSeen with aging
ApoptosisApoptosis ApoptosisProgrammed cell deathCell activates its own enzymes to destroy cellMembrane remains intactNo inflammationCell ultimately consumed by phagocytesJason Ryan, MD, MPHPixabay/Public DomainApoptosisApoptosisCauses Active process Embryogenesis Hormone withdrawal ATP-dependent Contrast with necrosis Occurs in hormone-dependent tissues Endometrium with progesterone withdrawal Some stimuli cause apoptosis and necrosis Immune cellsExample: myocardial ischemiaEvidence for both forms of cell deathInitial cellular response: apoptosis (avoids inflammation)Later response: necrosis (ATP depleted) ApoptosisT-cells in thymusB-cells in germinal centersDeath of self-reactive immune cellsImmune cells after inflammation resolvesApoptotic MechanismsCauses Caused by caspase enzymes DNA damaged cells Abnormal cells Infected cells (especially viral) Inactive enzymes in cytosol When activated apoptosis Two “pathways” for caspase activation Intrinsic (mitochondrial) pathway Initiated by mitochondriaWikipedia/Public Domain Extrinsic (death-receptor) pathway Membrane death receptors activatedWikipedia/Public Domain11Flikr/luncar caustic
Intrinsic PathwayElectron Transport Opening of mitochondrial membranes Release of cytochrome c Binds to APAF-1 (apoptosis-activating factor) Activation of caspasesInnerMembraneSpace Controlled by BCL2 family of proteins Some pro-apoptotic; some anti-apoptotic Balance determines if cell undergoes apoptosisH Pro-apoptosisAnti-apoptosisH Intrinsic Pathwaye-Cyt c Found in mitochondrial membranes Prevent cytochrome c from entering cytosol Pro-apoptosis: BAX and BAK proteins Bind to anti-apoptotic proteins Open pores in mitochondrial membranes Promote apoptosisInnerMembraneIVIIIBAXBAK As are for ApoptosisOuterMembranee-Intrinsic Pathway Many, many BCL2 family proteins Anti-apoptosis: BCL-2, BCL-XL, MCL1 proteinsCytosolCaspaseBCL-2BCL-XLMCL1Cyt cIntrinsic PathwayBAXBAKBCL-2BCL-XLMCL1Follicular Lymphoma CaspaseCyt cAPAF1CytosolMitochondrialMembrane12Subtype of non-Hodgkin lymphomaB-cell malignancyOverexpression of BCL-2Mitochondrial pores will not openCaspases cannot activateCell will not undergo apoptosisResult: Uncontrolled cell growthcCytosolMitochondrialMembrane
Intrinsic PathwayExtrinsic PathwayTriggers Withdrawal of growth factor Death receptors Hormones for hormone-sensitive tissue (uterus) Cytokines for immune cells Embryogenesis All part of TNF family of receptors Span plasma membrane into cytoplasm FAS (CD95) DNA damage Well-described death receptor found on many cells Binds FAS-ligand Triggers sequence that leads to activation of caspases DNA damage (radiation, chemotherapy) P53 can active BAK and BAX Abnormal proteins Caused by heat, hypoxia, low glucoseCD8 T-cellsExtrinsic PathwayKilling of virus infected cells Thymic medulla Activated by presentation of foreign antigens (MHC1) Release perforin and granzymes T-cells that bind to self-antigens die (negative selection) Death occurs via extrinsic pathway FAS-FAS-ligand interactions Lead to activated caspases Produce Fas ligand Binds to Fas (CD95) on surface of cellsWikipedia/Public DomainPublic Domain/WikipediaApoptosisExtrinsic PathwayCellular Changes Autoimmune lymphoproliferative syndrome Cell shrinkage Contrast with necrosis/swellingDefective FAS-FAS-ligand pathway for apoptosisPoor negative selection (more T-cell survival)Overproduction of lymphocytesLymphadenopathy, hepatomegaly, splenomegalyHigh risk of lymphomaAutoimmune diseases Chromatin condensation Pyknosis Hallmark of apoptosisWikipedia/Public Domain13
ApoptosisDNA LadderingCellular Changes Membrane blebbing Formation apoptotic bodies Membrane fragmentsCell organellesLigands for phagocyte receptorsConsumed by phagocytosisWikipedia/Public DomainApoptosis and Necrosis14Apoptotic caspases cleave DNA at specific regionsForms pieces in multiples of 180-185 kbpForms a “ladder” of sizes on gel electrophoresisNecrosis: random fragments
NecrosisNecrosis NecrosisJason Ryan, MD, MPHPixabay/Public DomainNecrosisCoagulative Necrosis Two major types Preservation of tissue architecture for days Injury damages cells and enzymes Coagulative Liquefactive Major difference from liquefactive necrosis Loss of enzymes limits proteolysis Tissue architecture remains intact for days Other types Form of cell deathCell membrane lossLeakage of cellular contentsElicits inflammatory responseAffects tissue bedsResults in gross and microscopic changesCaseousFibrinoidFatGangrenous Phagocytosis of cell remnants (takes time)Pixabay/Public DomainCoagulative NecrosisCoagulative Necrosis Gross: tissue becomes firm Microscopic: Architecture preservedCell nuclei lostRed/pink color on H&E stain (cell takes up more stain)Inflammatory cellsRyan Johnson/Flikr15
Coagulative NecrosisNormal HeartCoagulative Necrosis Seen with infarctions and ischemia Myocardium Kidney SpleenPost myocardial infarction Key exception: brain (liquefactive necrosis)RobinH/WikipediaRyan Johnson/FlikrLiquefactive NecrosisLiquefactive NecrosisLiquefactive NecrosisLiquefactive Necrosis Abscesses (bacterial/fungal) and brain infarctions Gross: liquid/pus or abscess cavity Microscopic: numerous neutrophils Cause in brain infarctions poorly understoodInfection draws inflammatory cellsTissue is “liquefied” into thick, liquid massEnzymes from microbesEnzymes from lysosomes of dying cellsBrain after strokeBrain after strokeR. Geetha/SlideshareWikipedia/Public Domain16
Caseous Necrosis Caseous Necrosis Gross: Cheesy-like (caseating) substance Microscopic: granulomatous inflammation“Cheese like”Rarely occurs outside of tuberculosis infectionMycobacteria resist digestionMacrophages form giant cellsSlow breakdown of infectionMycolic acid and lipids give cheese-like appearance Caseous NecrosisNecrotic centerRing of lymphocytes and macrophagesEpithelioid cellsGiant cells (fused activated macrophages)Caseous NecrosisPublic DomainWikipedia/Public DomainFat NecrosisFat Necrosis Necrosis of fat Classic example: acute pancreatitis Cause: lipases released from pancreatic cellsBreakdown of peritoneal fatFatty acids combine with calcium (saponification)“Chalky-white” tissueWikipedia/Public Domain17
Fat NecrosisFat Necrosis Fat necrosis of breast Results from traumaOften biopsy, surgerySports injury, seatbelt injuryCan mimic breast cancerWikipedia/Public DomainWikipedia/Public DomainGangrenous Necrosis Dry GangreneSubtype of coagulative necrosisCaused by ischemiaLost blood supply to limbs or bowelMultiple tissue layers involvedDry gangrene: dry, black, shrunken tissueWet gangrene: Superimposed bacterial infectionCoagulative and liquefactive necrosisMoist, soft, swollenPus, foul smellingJames Heilman, MD/WikipediaWet GangreneFibrinoid Necrosis Occurs in blood vessels Only visible under microscope (no gross findings) Occurs in autoimmune disorders Antibody-antigen complexes deposit in vessel walls Type III hypersensitivity reaction Fibrin leaks into vessel wall (pink on microscopy)S Anand/Slideshare18
Fibrinoid NecrosisFibrinoid Necrosis Classic disorder: polyarteritis nodosa Purpura Renal failure Neuropathy Severe hypertension/preeclampsia Not autoimmune Damage to vessel wall fibrin leakNephron/Wikipedia19
Inflammation PrinciplesInflammation Process for eliminating: Pathogens Damaged tissueInflammationPrinciples Commonly seen with infections, trauma, surgery May cause damage to host: Excessive inflammation (sepsis) Prolonged (infection fails to resolve) Inappropriate (autoimmune disease)Jason Ryan, MD, MPHInflammationCardinal Signs Acute inflammation Described by the ancient Romans Rubor (redness) and calor (warmth) Rapid onset (minutes to hours) Quick resolution (usually days) Caused by vasodilation and increased blood flow Chronic inflammation Tumor (swelling) May last weeks, months, or years Increased vascular permeability Brings cells/proteins (complement) to site of inflammation Dolor (pain) Loss of function Caused by other cardinal featuresVasodilationRubor and Calor Arteriolar vasodilation increased blood flowJames Heilman, MD/WikipediaWikipedia/Public Domain20
VasodilationEicosanoidsRubor and Calor HistamineLipids (cell membranes) Mast cells, basophils, platelets Preformed released quickly ProstaglandinsWikipedia/Public Domain Mast cells, leukocytes Synthesized via arachidonic acidLipoxygenasePhospholipase A2Arachidonic acidArachidonic oxanesPGE2HistamineFactor XIIBradykininHageman Factor Component of clotting cascade (minor role) Also produces bradykinin via the kinin systemXIIPrekallikrein (PK)XIIa ACE inhibitors can raise bradykinin levels Dangerous side effect: angioedemaKallikreinHigh molecular weight kininogenHMWKVasodilatorIncreases vascular permeabilityPain (B is for boo-boo)Degraded by angiotensin converting enzyme (ACE) Also degraded by C1 inhibitor (complement system) C1 inhibitor deficiency hereditary angioedemaBradykininVascular PermeabilityOncotic PressureTumorTumor Oncotic pressure ( ) changes drive fluid into tissue Rises in interstitial space (protein influx) May be caused by direct injury Also many mediators Leukotrienes: LTC4, LTD4, LTE4 Histamine, bradykinin Contraction of endothelial cells creates gaps Occurs in post-capillary venulesPcPiWikipedia/Public Domain21CapillaryInterstitialSpace c i
Tissue EdemaTissue Edema Exudate Transudate Inflammatory edema from high vascular permeabilitySeen in infection, malignancy (leaky vessels)High protein content (similar to plasma)High specific gravity (concentrated)Cause: hydrostatic pressure or oncotic pressureFluid leak NOT due to inflammationLow protein content (albumin remains in plasma)Low specific gravity (dilute, not concentrated)PcPi Exudate (infection, malignancy) Transudate (heart failure, low albumin) Thoracentesis Fluid tested for protein, LDH Light’s Criteria – Exudate if:InterstitialSpace c iPainPleural Effusion Causes:CapillaryDolor Key mediator: PGE2 Increases skin sensitivity to pain Also causes feverJames Heilman, MDFPGE2 Pleural protein/serum protein greater than 0.5 Pleural LDH/serum LDH greater than 0.6 Pleural LDH greater than 2/3 upper limits normal LDHAINSystemic InflammationVERFFever Fever Leukocytosis Acute phase reactants Pyrogens cyclooxygenase activity in hypothalamus prostaglandins in hypothalamusLipopolysaccharide: exogenous pyrogenIL-1 and TNF: endogenous pyrogensPGE2AIN Prostaglandins alter temperature set point Especially PGE2PGE222VER
Leukocytosis Normal WBC: 11.000/mm3 Infection: 15,000-20,000/mm3 Raging infection: 40,000-100,000/mm3 “Leukemoid reaction” Resembles leukemiaLeft Shift Normal response to infection More bands and neutrophilsBruceBlaus/Wikipedia Cytokines (TNF and IL-1) cells from bone marrow Bacterial infections: neutrophils (neutrophilia) Viral infections: lymphocytes (lymphocytosis)Acute Phase Reactants C Reactive Protein (CRP)Serum proteinsLevels rise with inflammation (acute or chronic)Mostly produced by liverSynthesis increased by cytokines often IL-6C-reactive proteinSerum amyloid AFerritinHepcidinFibrinogen Liver synthesis in response to IL-6 (macrophages)Binds bacterial polysaccharidesActivates complement systemChronic increased levels associated with CADPixabay/Public DomainSerum Amyloid A ProteinsFerritinSAA Proteins Apolipoproteins Many roles in inflammatory response Causes AA (secondary) amyloidosis Occurs in chronic inflammatory conditions Rheumatoid arthritis, ankylosing spondylitis, IBDBinds ironIron storage proteinStored intracellularly as ferritinStored in macrophages of liver and boneClinical significance: Diagnosis of iron deficiency during infectionEd Uthman, MDTomihahndorf23
HepcidinFibrinogen Anti-bacterial properties Inhibits iron transport Factor I of the clotting cascade Promotes cellular adhesions Platelets, endothelial cells Binds to ferroportin in enterocytes, macrophages Iron trapped in cells as ferritin Contributes to anemia of chronic diseasePublic DomainESRESRErythrocyte Sedimentation RateErythrocyte Sedimentation Rate Rate of RBC sedimentation in test tube Determined by balance of factors Normal 0-22 mm/hr for men; 0-29 mm/hr for women Pro-sedimentation: APRs, especially fibrinogen (sticky) Anti-sedimentation: negative charge of RBC Increased by acute phase reactants in inflammation High levels APRs red cells stick together Faster sedimentation increased ESRMechESR/WikipediaESRESRErythrocyte Sedimentation RateErythrocyte Sedimentation Rate ESR 100 (normal 30) seen in: Reduced ESR ( 5) Hypofibrinogenemia Heart failure (controversial; mechanism unclear)EndocarditisTemporal arteritisPolymyalgia rheumaticaTrauma/surgeryMalignancy Abnormal red cell shapes Sickle cell anemia Spherocytosis Microcytosis Anemia: Increased ESR Sedimentation of red cells slower with more red cells Red cells impeded one another’s sedimentation Polycythemia (opposite of anemia) Result: ESR may be normal despite inflammation Renal disease (some due to anemia)24
Negative APRs Levels fall in inflammationSynthesis inhibited by cytokinesAlbuminTransferrinTransthyretin25
Acute and Chronic InflammationInflammation Acute inflammation Rapid onset (minutes to hours) Quick resolution (usually days)Acute & ChronicInflammation Chronic inflammation May last weeks, months, or yearsJason Ryan, MD, MPHAcute InflammationInnate Immune System Part of innate immunity Three hallmark features Phagocytes (debris clearing) Macrophages Neutrophils Increased blood flow (vessel dilation) Increased vascular permeability Emigration of neutrophils into tissues Rapid onset/short duration Occurs within minutes of trigger Resolves in minutes/hours/daysMacrophages ComplementNatural Killer CellsEosinophilsMast cells and BasophilsMacrophages Recognize molecules that are “foreign” “Damage-associated molecular patterns” (DAMPs)Macrophages: guardians of innate immunityFound in tissues; capable of phagocytosisRecognize cellular damage, microbes, foreign bodiesInitiate acute inflammatory responseSimilar role played by mast cells, dendritic cells Present only when tissue damage occurs Example: mitochondrial proteins, DNA “Pathogen-associated molecular patterns” (PAMPs) Present on many microbes Not present on human cellsDr Graham Beards/Wikipedia26
MacrophagesInflammasome Key receptors: “Toll-like receptors” (TLRs) Cytosolic protein complex found in many cells Key for recognition of cell damage Activated by components of damaged cells:Macrophages, dendritic cells, othersFound on cell membrane and endosomesPattern recognition receptorsRecognize PAMPs/DAMPs secrete cytokinesActivation cytokines, inflammatory signals Uric acid Extracellular ATP Free DNA Other activators: Leads to production of IL-1 Leads to release of inflammatory mediators Fc portion of antibodies Complement proteinsInflammatory MediatorsNeutrophil “Vasoactive amines” Histamine Serotonin Lipid products (arachidonic acid derived) Prostaglandins Leukotrienes ComplementDerived from bone marrowCirculate 5 days and die unless activatedDrawn from blood stream to sites of inflammationEnter tissues: phagocytosisProvide extra support to macrophagesDr Graham Beards/WikipediaNeutrophilAcute InflammationBlood stream exitTypical Timeline Exit vascular system at post-capillary venules Four steps to extravasation (exit vessels to tissues) Neutrophils dominate early ( 2 days) Many in blood stream Attach firmly to adhesion molecules Apoptosis after 24-48hrs Rolling, crawling, transmigration, migration Monocytes/macrophages dominate late ( 2 days) Live longer Replicate in tissuesWikipedia/Public Doainm27
Acute InflammationTypical TimelineNeutrophilsTypical Timeline: ExceptionsMacrophages &Monocytes Pseudomonas infection Neutrophils dominate for days Viral infections Lymphocytes often appear first Hypersensitivity reactionsActivityEdemaAcute Inflammation Eosinophils dominate1Days2Acute InflammationChronic InflammationResolution Three potential outcomes #1: Resolution of inflammation Removal of microbes/debris Tissue returns to normal #2: Healing/scar Tissue damage too extensive for regeneration Connective tissue growthProlonged inflammation (weeks/months)May follow acute inflammationMay begin slowly (“smoldering”) on its ownTissue destruction and repair occur at same time #3: Chronic inflammationChronic InflammationChronic InflammationCausesCells Mononuclear cells Persistent infections Macrophages Lymphocytes (T and B cells) Plasma cellsDifficult to clear microbesMycobacteriaParasitesProlonged infection type IV hypersensitivity reaction Macrophages are dominant cell type Autoimmune diseases P
Pathology Slides Color slides for USMLE Step 1 preparation from the Boards and Beyond Website Jason Ryan, MD, MPH 2021 Edition Boards & Beyond provides a virtual medical school curriculm used by students around the globe to supplement their ed